Polishing Monolithic IPS e.max® and Zirconia Restorations
The first part of a pilot study examining materials and methods
Edward A. McLaren, DDS, MDC | Johan Figueira, DDS | Luis Sanchez, DDS | Carlos Trujillo, DDS
Many improved ceramics have been delivered to the dental market throughout the years. With innovations in strength and translucency and the ability to internally color ceramics, modern monolithics can satisfy patients’ esthetic desires. The term monolithic means something formed from a single block of stone. In dental ceramics, the definition refers to the restoration being made from a monolayer material that is either machined or pressed, to which no second layer such as porcelain is added.
Two major forms of monolithic ceramics are used in dentistry today. One of them is glass ceramic, which is created from a controlled crystallization of glass with the crystalline phase consisting of about 70% lithium disilicate crystals in a matrix of approximately 30% SiO2-based glass. The most well-known product in this category is IPS e.max® (Ivoclar Vivadent, www.ivoclarvivadent.com).1 These products can be pressed by a lost-wax process or machined from a partially crystallized “blue block,” and then undergo final crystallization in a porcelain oven. The other more recently developed type of monolithic ceramic material is a form of solid-sintered zirconia-based ceramics (eg, Lava™ Plus, 3M ESPE, www.3mespe.com or BruxZir, Glidewell Laboratories, www.bruxzir.com)2 that is more translucent than original versions delivered to the market. These materials are dense polycrystalline solids with no glass phase and with an average particle size less than 0.5 µm. Both materials have essentially replaced metal ceramic restorations as the first choice for posterior full-crown restorations.
As with any dental restoration, the characteristics of smoothness and high polish are important for several reasons. Mainly, rough areas collect and maintain plaque and stain,3 which can lead to secondary caries and periodontal problems.4 Also, rougher areas are more abrasive to opposing teeth and/or restorations, which can lead to accelerated occlusal wear.3 One challenge with these newer monolithic materials is that they are much harder materials than natural tooth structure, which makes them more difficult to re-polish after occlusal adjustment than earlier conventional porcelains. Also, harder surfaces won’t self-adjust;5 even though a smooth zirconia surface left in supra-occlusion might not be abrasive, the potential risk for impact fracture may be increased. Polishing well prior to delivery of the restoration is important, and having an effective system to adjust and re-polish after cementation of the restoration is also essential. Special polishers have been developed for these harder materials, as polishers used for the softer porcelains were not ideal. Another challenge of effective post-cementation re-polishing is generating sufficient torque from chairside air-driven handpieces.
The aim of this pilot study. which will be followed up with a larger study and subsequent report, was to test the efficacy of manual polishing procedures of a specific polishing system developed specifically for IPS e.max and zirconia on roughened surfaces of IPS e.max and Lava Plus. Then the researchers compared the quality of polish with the same polisher but using air-driven versus electric handpieces, which generated much higher torque.
Materials and Methods
For the initial part of this polishing study, 10 specimens of IPS e.max (Figure 1) were fabricated to 4 mm x 10 mm x 16 mm by using a sectioning saw for IPS e.max C16 blocks. Ten specimens of Lava Plus (Figure 2) were also fabricated with the dimensions of 4 mm x 10 mm x 10 mm. Both materials were processed according to the manufacturers’ directions. After processing, grinding of the surfaces of all 20 specimens was performed to simulate occlusal adjustment. A new fine diamond was used for each specimen. A Brasseler 8881 fine diamond with water in an electric high speed was utilized uniformly on the whole surface (Figure 3). The specimens were divided into four groups.
Group 1
The specimens were polished with air-driven contra angle clinical handpieces (Figure 4) with water using the special intraoral polishing system designed for IPS e.max, the Dialite LD Extra-Oral Polisher System (Brasseler), following the directions of the manufacturer (Figure 5 through Figure 8). In Figures 9 through Figure 11, a new polisher, Dialite Feather Lite, was used, as this system allows better access to polish grooves. One operator did all the polishing so as to better calibrate the manual results. Also, with air-driven it is not possible to control the speed, or RPMs, so 60 seconds was allotted for each polished piece. The air pressure was calibrated to 4.5 bars to get as much torque as possible. Dialite Extra-Oral Polishing Paste (Brasseler) was used with a small round brush 60 seconds with each grit (Figure 12 and Figure 13).
Group 2
The IPS e.max specimens were polished with electric contra-angle handpieces (Figure 14) with water using the same special intraoral polishing system designed for IPS e.max following the manufacturer’s directions. This was done as electric handpieces deliver much more torque; the hypothesis is that the electric handpieces will polish better. The same operator performed all the polishing. The speed was set to the manufacturer’s recommendations of 8,000 RPM. The same allotted time of 60 seconds per instrument was used. Medium and fine diamond polishing paste was used with a small round brush for 60 seconds with each grit.
Group 3
The Lava specimens were polished with air-driven contra angle clinical handpieces (Figure 4) with water using the special intraoral polishing system designed for zirconia, the Dialite ZR Zirconia Intra-Oral Adjustment/Polishing System (Figure 15 through Figure 18), following the manufacturer’s directions. One operator performed all the polishing. A total of 60 seconds was allotted for each polished, but the air pressure was calibrated to 4.5 bars to get as much torque as possible. This time was chosen, as few dentists would spend more than 60 seconds per polisher to repolish an occlusal adjustment per tooth. Medium and fine diamond polishing paste was used with a small round brush for 60 seconds with each grit.
Group 4
The Lava specimens were polished with electric contra-angle handpieces with water using the same special intraoral polishing system designed for zirconia following the manufacturer’s directions. The same operator performed all the polishing. The speed was set to manufacturer’s recommendations of 8,000 RPM. The same allotted time of 60 seconds per instrument was used. Medium and fine diamond polishing paste was used with a small round brush for 60 seconds with each grit.
Results and Discussion
In this initial part of the study, a micro-surface roughness test to measure Ra was not done; this will be addressed in a full-length paper. Scanning electron microscope (SEM) images and close-up photographic analysis clearly show the differences between groups.
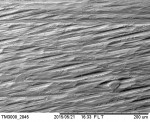
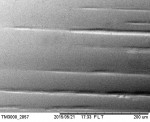
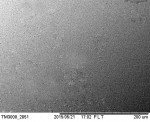
SEM images and photographic analysis of post-grinding/adjustment with an 8881 fine diamond clearly demonstrate a rough surface (Figure 19 and Figure 20). The SEM and visual images of the zirconia specimen after adjustment using air-driven handpieces clearly show some significant groves that were not removed (Figure 21 and Figure 22). This is believed to be due to the relatively low torque generated with air-driven handpiece and the hardness of the zirconia. In the authors’ experience, this is true with other specialized systems on the market to polish zirconia. Air-driven handpieces don’t generate enough torque to adequately re-polish zirconia. The SEM and visual images of the zirconia specimen after adjustment using electric handpieces with the same polishers as used for air-driven clearly show a much smoother surface (Figure 23 and Figure 24).
Figure 25 and Figure 26 show visual images and SEM analysis of IPS e.max after adjusting with an 8881 fine diamond, which clearly shows a roughened surface similar to a post intraoral adjustment. The SEM images of air-driven versus electric polishing of IPS e.max don’t demonstrate a significant difference (Figure 27 and Figure 28). and both images demonstrate a very smooth surface (at least in the area scanned, which was a 0.5-mm-square area). The images tell a slightly different story. In the visual image of the air-driven polished specimen versus the electric polished specimen (Figure 29), a slightly smoother overall surface can be seen. Also, remember the air pressure was 4.5 bars, which is higher than most dental offices that have the air pressure set mainly to protect turbine life.
Summary
Newer and better ceramics are being developed all the time. Two new versions used as monolithic final restorations have been in wide use. Due to these products’ high strength and hardness, special polishers have been developed to assist dentists in post-cementation occlusal adjustment. The Dialite LD Extra-Oral Polisher System and Dialite ZR Zirconia Intra-Oral Adjustment/Polishing System were tested and found to be extremely effective when used with higher torque electric handpieces. These systems also offer special diamonds and stones (grinders) that are recommended for gross reduction if necessary. They generate less heat when grinding than conventional stones and diamonds, which helps minimize potential for post-processing adjustment. IPS e.max, which has a lower strength and hardness, also polished reasonably well with air-driven handpieces but set at a higher air pressure that might not be practical in a private dental office.
Disclosure
Edward A. McLaren, DDS, MDC; Johan Figueira, DDS; Luis Sanchez, DDS; and Carlos Trujillo, DDS, have no conflicts of interest to disclose relative to this article.
References
1. Kelly JR, Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Aust Dent J. 2011;56(Suppl 1): 84-96.
2. McLaren EA, Giordano RA. Zirconia-based ceramics: material properties, esthetics, and layering techniques of a new veneering porcelain, VM9. QDT. 2005(28):99-111.
3. Aykent F, Yondem I, Ozyesil AG, et al. Effect of different finishing techniques for restorative materials on surface roughness and bacterial adhesion. J Prosthet Dent. 2010;103(4):221-227.
4. Scotti R, Zanini Kantorski K, Scotti N, et al. Early biofilm colonization on polished- and glazed-zirconium ceramic surface. Preliminary results. Minerva Stomatol. 2006;55(9):493-502.
5. Lawson NC, Janyavula S, Syklawer S, et al. Wear of enamel opposing zirconia and lithium disilicate after adjustment, polishing and glazing. J Dent. 2014;42(12):1586-1591.
About the Authors
Edward A. McLaren, DDS, MDC
Professor
Founder and Director
UCLA Postgraduate Esthetics
Director
UCLA Center for Esthetic Dentistry
Founder and Director
UCLA Master Dental
Ceramist Program
Private practice limited to Prosthodontics and Esthetic Dentistry
UCLA School of Dentistry
Los Angeles, California
Luis Sanchez, DDS
Senior Graduate Student
Advanced Esthetic and Restorative Dentistry
UCLA School of Dentistry
Los Angeles, California
Johan Figueira, DDS
Graduate and Guest Instructor
UCLA Center for Esthetic Dentistry
Los Angeles, California
Carlos Trujillo, DDS
Senior Graduate Student
Advanced Esthetic and Restorative Dentistry
UCLA School of Dentistry
Los Angeles, California