Intraoral Occlusal Adjustment and Polishing for Modern Ceramic Materials
Clinical performance depends more on surface finish than the type of ceramic used
John C. Kois, DMD, MSD | Yada Chaiyabutr, DDS, DSc, MSD
During the past decade, newer dental materials, such as lithium disilicate and zirconia-based ceramic, have become widely used along with the technology used to process them—computer-aided design (CAD) and computer-aided manufacturing (CAD/CAM). Lithium disilicate is common for use in all-ceramic restorations both as a core and as a monolithic full-contour restoration, with successful restorations fabricated by using a pressed technique or milling through a CAD/CAM system.1 Lithium disilicate can be acid-etched and bonded to the tooth structure, giving it a clinical advantage that it has been shown to exhibit over zirconia. As a result, lithium-disilicate restorations demonstrate good durability, with fewer restorations chipping after short periods in service.1,2-4
Zirconia-based ceramics have excellent mechanical properties due to their unique transformative abilities and toughening capabilities. Dentists generally use three systems: 3 mol% yttria-stabilized tetragonal zirconia polycrystals (3Y-TZP), magnesia-partially stabilized zirconia (Mg-PSZ), and zirconia-toughened alumina (ZTA).5,6 Due to zirconia’s poor translucency, zirconia-based ceramics were veneered with feldspathic porcelain to better match natural teeth. Studies reported that these restorations fractured after short service periods and under low loading forces.7,8 Chipping of veneering porcelain was common, and framework fractures were observed in the pre-sintered stage of zirconia.9,10 To address these chipping problems with the veneering porcelain, monolithic full-contour zirconia with improved opacity was introduced as an alternative restorative material.11,12 Because monolithic zirconia is harder than feldspathic porcelain, the excessive wear of enamel when in function opposite zirconia has been attributed to its hardness relative to feldspathic porcelain. Recent studies, however, have revealed enamel wear could be significantly affected by the amount of zirconia surface finish.13-17 Polished zirconia resulted in the least wear of opposing enamel, even after simulated aging.15,16 Glazed zirconia revealed higher enamel wear rates than that of polished zirconia because the thin glaze layer disappeared after a period of function.15,16 Consequently, a rough zirconia surface appeared to act as an aggressive abrasive. Specific clinical protocols for surface finishing after occlusal adjustment of all-ceramic restorations should be considered.
Chairside Occlusal Adjustment
In general, chairside occlusal adjustment of all-ceramic restorations involves selective grinding and finishing or polishing procedures. This is done not only to minimize enamel wear, but also to prevent ceramic fracture or failure. Surface imperfections, such as grooves and scratches, created by natural grinding forces can act as stress initiators in the materials. As a result, materials can fracture, starting with a crack followed by crack propagation at stress levels that are well below the yield strength. Surface polishing can reduce this effect and is influenced by a number of factors, such as the structure and mechanical properties of the ceramic, the size and shape of the abrasive, the difference in hardness between the abrasive and the ceramic, the physical properties of the material that is used to carry the abrasive material, and what type of lubrication is used during the application of the abrasive.18
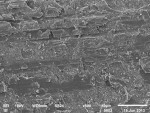
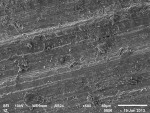
Surface roughness of ceramic materials depends on its homogeneity and microstructure (grain size).5,6 The grinding rotary instrument for zirconia contains a highly dense diamond abrasive. Although relatively hard, zirconia is still not as hard as alumina and diamond. The rotary instrument should be changed sequentially from coarse (large grain size) to fine (small grain size) diamond abrasives (Figure 1 and Figure 2) to achieve the maximum smooth surface. Larger diamond grains have higher abrasiveness for ceramic, which also increases the amount of surface roughness.
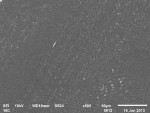
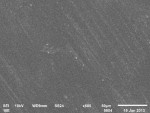
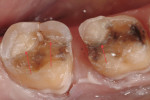
Occlusal adjustment on ceramic restorations should be performed with a fine diamond bur at slow speed and a water coolant to minimize the risk for crack propagation. Polished, anatomically contoured restorations may be indicated in high load-bearing areas; however, glazing the restorations should be avoided unless high esthetics is needed. Recently, a polyurethane bur impregnated with fine diamond particles was introduced into the market. A study examined the effects of occlusal adjustment on the surface roughness after occlusal adjustment of three ceramic crowns: feldspathic, lithium disilicate, and zirconia ceramic. A silicone point polisher and two different polyurethane rubber polishers were used. All occlusal adjustments and polishing were performed continuously for 20 seconds on the flat occlusal surfaces of the crowns at 10,000 rpm. The results revealed that polishing with fine polyurethane rubber polisher burs led to the least surface roughness (Figure 3 through Figure 8).19 Friction-grip brownie points work similarly; however, the silicone point would wear faster.
Polishing Procedures
For polishing procedures, an application of polishing paste can be used at the final polishing step. The most common abrasives found in polishing pastes include:
• Aluminum oxide
• Pumice
• Silica
• Silicon dioxide
• Tin oxide
• Diamond particles
In general, aluminum-oxide pastes are safe for porcelains.20 Aluminum and aluminum oxide can both be used on stain-free surfaces. However, if ceramic restorations need to be polished to improve shine or luster, a product containing diamond particles should be chosen. Always follow the manufacturer’s recommendations for specific polishing agents to ensure proper results and success; see Case 1 (Figure 9 through Figure 13) and Case 2 (Figure 14 through Figure 20).
Conclusion
Excellent clinical performance depends more on surface finish than the type of ceramic used. Grinding while performing occlusal adjustment adversely affects the mechanical properties of lithium disilicate and zirconia ceramic. When grinding on ceramics, lower temperatures (air-water coolant) and a less-aggressive diamond grit (<150 µm) are recommended to minimize the risk for crack propagation. Finish or polish the ceramics with fine polyurethane rubber polishing burs.
Acknowledgment
We would like to thank Steve McGowan from Arcus Dental Laboratory for providing the laboratory work for these cases.
Disclosure
John C. Kois, DMD, MSD and Yada Chaiyabutr, DDS, DSc, MSD, have no conflicts of interest to disclose relative to this article.
References
1. Lin WS, Ercoli C, Feng C, Morton D. The effect of core material, veneering porcelain, and fabrication technique on the biaxial flexural strength and weibull analysis of selected dental ceramics. J Prosthodont. 2012;21(5):353-362.
2. Silva NR, Thompson VP, Valverde GB, et al. Comparative reliability analyses of zirconium oxide and lithium disilicate restorations in vitro and in vivo. J Am Dent Assoc. 2011;142(Suppl 2:):4S-9S.
3. Pieger S, Salman A, Bidra AS. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 2014;112(1):22-30.
4. Toman M, Toksavul S. Clinical evaluation of 121 lithium disilicate all-ceramic crowns up to 9 years. Quintessence Int. 2015;46(3):189-197.
5. Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008;24(3):299-307.
6. Miyazaki T, Nakamura T, Matsumura H, et al. Current status of zirconia restoration. J Prosthodont Res. 2013;57(4):236-261.
7. Vult von Steyern P. All-ceramic fixed partial dentures. Studies on aluminum oxide- and zirconium dioxide-based ceramic systems. Swed Dent J Suppl. 2005;(173):1-69.
8. Vult von Steyern P, Carlson P, Nilner K. All-ceramic fixed partial dentures designed according to the DC-Zirkon technique. A 2-year clinical study. J Oral Rehabil. 2005 32(3):180-187.
9. Raigrodski AJ, Chiche GJ, Potiket et al. The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: a prospective clinical pilot study. J Prosthet Dent. 2006;96(4):237-244.
10. Larsson C, Vult von Steyern P, Sunzel B, Nilner K. All-ceramic two- to five-unit implant-supported reconstructions. A randomized, prospective clinical trial. Swed Dent J. 2006;30(2):45-53.
11. Baldissara P, Llukacej A, Ciocca L, et al. Translucency of zirconia copings made with different CAD/CAM systems. J Prosthet Dent. 2010;104(1):6-12.
12. Alghazzawi TF, Lemons J, Liu PR, et al. Evaluation of the optical properties of CAD-CAM generated yttria-stabilized zirconia and glass-ceramic laminate veneers. J Prosthet Dent. 2012;107(5):300-308.
13. Preis V, Behr M, Kolbeck C, et al. Wear performance of substructure ceramics and veneering porcelains. Dent Mater. 2011;27(8):796-804.
14. Rosentritt M, Preis V, Behr M, et al. Two-body wear of dental porcelain and substructure oxide ceramics. Clin Oral Investig. 2012;16(3):935-943.
15. Burgess JO, Janyavula S, Lawson NC, et al. Enamel wear opposing polished and aged zirconia. Oper Dent. 2014;39(2):189-194.
16. Albashaireh ZS, Ghazal M, Kern M. Two-body wear of different ceramic materials opposed to zirconia ceramic. J Prosthet Dent. 2010;104(2):105-113.
17. Kontos L, Schille C, Schweizer E, Geis-Gerstorfer J. Influence of surface treatment on the wear of solid zirconia. Acta Odontol Scand. 2013;71(3-4):482-487.
18. Jefferies SR. Abrasive finishing and polishing in restorative dentistry: a state-of-the-art review. Dent Clin North Am. 2007;51(2):379-397.
19. Chaiyabutr Y, Kois JC, Kois DE. Effects of occlusal adjustment on surface roughness of all-ceramic crowns. J Dent Res. 2015;94(spec iss a):3633.
20. Sen D, Göller G, Işsever H. The effect of two polishing pastes on the surface roughness of bis-acryl composite and methacrylate-based resins. J Prosthet Dent. 2002;88(5):527-532.
About the Authors
John C. Kois, DMD, MSD
Founder and Director of Kois Center
Seattle, Washington
Yada Chaiyabutr, DDS, DSc, MSD
Research Director of Kois Center
Seattle, Washington