A Mandibular Implant Screw-Retained Bridge as a Partial Denture Replacement
Coordination of care between the prosthodontist, oral surgeon, and laboratory technician makes this a viable option for a natural look with good occlusal function.
In the case presented in this article, a 75-year-old woman presented with an ill-fitting partial she wanted replaced with fixed restorations. The clinician performed a complete dental evaluation using a cone-beam computed tomography (CBCT) scan to assess the possibility of placing two implants in the mandibular anterior component.
The CBCT scan helped determine that the patient had relatively good bone density. Surgical sites were placed in the area of teeth Nos. 23 and 25 using a stereo lithographical stent. Two BioHorizons® 3- x 15-mm tapered implants (BioHorizons, Inc., www.biohorizons.com) were then successfully placed in the mandibular anterior component as planned.
From the technician’s viewpoint, the first question about the case was which tooth to color match for balance: No. 22 or No. 27? The crown on tooth No. 27 was old and had a fake appearance; therefore, the patient and clinician both asked the technician to match tooth No. 22 but in a slightly lighter color because of the ochre staining that showed through on the natural tooth. The technician decided to base his restoration color on A-1 but add a multiple number of colors into the final result.
The second question was the position of the teeth for the screw-retained implants. The technician ordered titanium CAD/CAM abutments from Nobel Biocare (www.nobelbiocare.com) and applied a wax design for proper contour. Titanium has become a viable alternative to gold because of the fluctuating, high prices of gold, while titanium has one low set price. The material also saves time because it requires no waxing, investing, divesting, or degassing.
Next, the size of the teeth from the incisal edge to the gingival as well as the mesial and the distal was considered. He did not want the teeth to be too long in size and also did not want to create “piano teeth.” Because a natural appearance was desired in the occlusal view, a protruding view to the incisal one-third position between teeth Nos. 23 and 24 and again between teeth Nos. 25 and 26 was added. The gingival size of the teeth was also decreased in consideration of creating a more lifelike exterior.
Case Study
Implants were surgically placed in the areas of teeth Nos. 24 and 25 in the lower anterior (Figure 1). Note a blue marking to the gingival area around tooth No. 23. This discoloration is not an artifact but an amalgam tattoo associated with long-standing amalgam, which was trapped in the patient’s tissue. It is not significant, but if it was in a critical zone a bone grafting process could have been instituted for esthetic purposes.
Using implant protocol, a heavy/light-body viscosity impression material was used in a custom tray (Figure 2). Standard operating procedure was carried out with facebow centric relation transfer using a Panadent® Articulator (Panadent Corporation, www.panadent.com). It was decided that teeth Nos. 22 and 27 would receive full coverage at a later date to compliment the color scheme of the mandibular.
To ensure stability in the transfer of information from the mouth to the stone working model, the clinician wrapped dental tape securely around the teeth in a figure eight position (Figure 3). The technician was able to check for correct tissue color using the Chairside Shade Guide™ (LSK121 Oral Prosthetics, www.lsk121.com) during this stage. The clinician applied Primopattern LC gel (Primotec® USA, www.primogroup.net) over and around the dental tape for stability and accuracy of the implant transfer to the model (Figure 4). A small amount of wax was placed on the open-tray impression screws to avoid the impression material flowing into the opening. A sample of the Primopattern LC gel was then used to check the stability of the implant transfer stage.
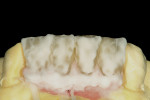
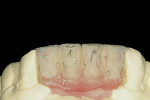
The copings on the four-unit bridge were tried on the model to check occlusion (Figure 5) after the opaque stage. GC Initial™ Ti Porcelain (GC America Inc, www.gcamerica.com) was the porcelain of choice for the author/technician (Figure 6). The size of teeth from the incisal to the gingival to the pontic was given a shorter appearance (Figure 7) by adding a pink porcelain application and enamel overlay, which closely mimics natural tissue. After firing, the technician applied his enamel build-up with pink porcelain and the clear fluorescence/translucency (Figure 8).
Figure 9 shows the appearance of the enamel and translucency application after baking. The surface texture and line angles were drawn onto the model next (Figure 10). After finishing the texture application and baking for the third time (Figure 11), the restorations were nearly complete. After the final glaze was applied and the incisal one third anterior translucency modification was checked using the Chairside Shade Guide (Figure 12), the implant bridge was ready to be placed.
The technician performed a fit check on the model (Figure 13 ) before it was placed in the mouth (Figure 14). Figure 15 shows the placement in the mouth compared with the partial. The dentist then permanently screwed the implant bridge into place (Figure 16).
Conclusion
When planning the finished results for the case, the clinician was careful to note the trajectory of the implants to allow perfect placement of the screw-retained prosthesis with precise lingual trajectory. Through careful planning and cone-beam stereolithography, the patient’s bone parameters were accurately measured and memorized leading to a successful outcome. It is an excellent example of coordination between the prosthodontist, oral surgeon, and the laboratory technician.
The first step the technician took was to check the patient’s color balance and the position of the implants to create correct wax design. Upon evaluation of the patient’s existing dentition, it was clear to the technician that to create a natural look for this case the teeth needed to be decreased in size gingivally. Therefore, he carefully measured the teeth from the incisal to the gingival and the mesial to the distal. When checking the occlusal view, he was careful not to create “piano teeth.” A more natural look was achieved by adding to the protrusion of the teeth, moving them forward and backward across the mandibular area. A proportion check helped with the final evaluation of the patient’s case result, leading to an excellent finish.
Disclosure
Mr. Kahng is a paid consultant for GC America.
About the Authors
Joseph L. Caruso, DDS, MS
Private Practice
Chicago, Illinois
Luke S. Kahng, CDT
Owner LSK121 Oral Prosthetics
Naperville, Illinois