The Virtual Dental Patient: Digitally Designed All-on-X
Immediate full-arch, implant-supported surgical prosthetics
David Lee Hill, Jr., DDS; Michael A. Pikos, DDS; Daniel R. Llop, CDT
The process of providing functional, esthetic treatment for the terminally dentate or edentulous patient has been changed dramatically due to the innovative and immediate approach of cone-beam computer tomography-guided full-arch surgery (CBCT-GFA). Computed tomography-guided treatment planning allows for instantaneous biomechanical, biological, patient-specific diagnosis, consequently reducing the possibility for complications significantly and increasing the probability for predictable results, such as as substantial grafting procedures and bone osteotomy augmentation.1 This focused planning is driven by two major factors: virtually advanced kinesiology concepts and virtual facially driven esthetics. Because the inherent maxillofacial skeleton (ie, the evaluation of the centric relationship [CR] of the condyles as compared to vertical dimension and interocclusal space) provides enormous potential as an already-existing tissue anchor,2-7 we are able to use an approach that builds on the more conventional denture conversion technique using functional CT-guided surgery. This provides an opportunity to direct the attention to “the virtual dental patient” to provide the clinical patient with an already-perfected, functional, multidisciplinary treatment plan. The following is a case presentation of an existing physiologic treatment for a CT-guided candidate (Figure 1).
Case Presentation
A 49-year-old man was referred by his general dentist for comprehensive evaluation and to discuss possible implant reconstruction and fixed options. According to the patient’s report, he had had a long-standing dental history with numerous restorative and prosthodontic needs. His concern for his failing dentition led him to seek a more fixed type of solution. Research led him to discover the All-on-4® technique (Nobel Biocare; www.nobelbiocare.com), which presents a permanent solution to a worsening problem.
The protocol for placement of dental implants followed by immediate loading with placement of a prefabricated fixed, bar-supported polymethyl methacrylate acrylic (PMMA) prosthesis, which included the biologic and physiologic benefits of this treatment option, was reviewed with the patient.The immediate-load technique helps prevent continued resorption of the alveolus and jaw, aids in the ability to chew (or masticate), improves speech, and helps sustain the patient’s overall bony and soft-tissue anatomy fencing to improve the natural facial contour.8,9 Using the virtual work-up, the already strategically placed implants can be delivered to the patient predictably in a controlled 90-minute to 3-hour surgical appointment.
Appreciation for the concept of immediate loading is well understood. In 1969, Brånemark first suggested topographically positioning four implants in the edentulous maxilla and four implants in the edentulous mandible. Malo et al introduced the All-on-4 treatment concept that involves immediate loading of a full-arch fixed prosthesis secured with four implants in the maxilla or mandible.8,10-12
However, the treatment of the resorbed edentulous maxilla and mandible is not without an inherent and unique set of problems.13,14 The placement of implants by the practitioner is limited by the posterior maxilla due to bilateral maxillary sinuses, thus limiting the necessary anterior and posterior distribution to support the occlusal load placed on the maxillary fixed prosthesis. Establishing adequate anterior and posterior distribution of the implants is further limited by the presence of residual alveolar bone, which is typically seen secondary to loss of both bone and soft tissue as a result of tooth removal and generalized periodontitis.7,10 A comprehensive evaluation of the patient and CT-guided virtual workup of the patient’s DICOM data can help to identify and address problems with the missing teeth, bony defects, and resorbed tissue as well as offer tremendous benefit to the surgical, prosthodontic, and restorative teams.
The virtual dental patient work-up modality helps to address several of the key factors in treatment of the terminally dentate and edentulous patient population. An assessment of the patient’s smile line, transition zone of the maxillary alveolar ridge and prosthesis secondary to the presence or absence of a composite defect, facial flange requirements due to the presence or lack of residual ridge crest, vertical dimension of occlusion (VDO), and the amount of bone available in three separate zones of the maxilla are determined with the CBCT scan and virtual workup. The evaluation of these three radiographic zones allows for preoperative determination of whether the patient has adequate arch.
Based on early Malo All-on-4 treatment principles and using Pikos’ “Same Day Teeth®” evaluation and treatment philosophy, these facially driven treatment principles include the evaluation of 1) facial and dental midline; 2) occlusal plane; 3) VDO; 4) force factors; 5) cantilever elements; 6) anterior-posterior spread; 7) bone volume and density; 8) implant and abutment selection and placement; 9) screw-access holes; 10) path of prosthesis insertion; 11) bone reduction; and 12) discussion and virtual implementation of provisional and definitive prosthetic materials. Implants, abutments, and all other pertinent components are then ordered for the patient-specific digital treatment plan.1,7,8,10-12
To initiate the Virtual Dental Patient®, the authors used the proprietary, patent-pending nSequence stackable surgical and prosthetic guides and protocol to accurately translate the virtual surgical and restorative work-up to the oral environment. They took a set of excellent clinical photographs with the shade tab in view and then scanned the patient using the CBCT-GFA dual-scan method, which involves the first scan being set in centric relation (CR) in the final established VDO and the second scan with the patient smiling to overlay onto the DICOM data sets. What followed was a set of intraoral scans of the upper and lower arch in the proper VDO/CR position, to be evaluated skeletally during the GoToMeeting™ (GTM) (www.gotomeeting.com) during the temporomandibular joint (TMJ) analysis. Next, digital prescription notes were completed and sent off with the digital data sets to nSequence (Reno, Nevada) to process the data and pre-plan the full-arch virtual patient case according to the diagnosis and treatment plan.
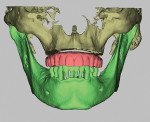
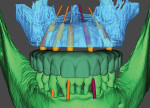
At nSequence, the digital data is processed and composed symphonically to create an accurate virtual dental patient, with both hard and soft tissues, to start the multidisciplinary workup with the restoring dentist, the oral-maxillofacial surgeon, and the dental technician at the GTM stage of the treatment planning session (Figure 2). The dental laboratory pre-plans by preparing an excellent rendition of the patient’s skeletal topography, condyles, tooth and root anatomy, nerves, sinus, and facial anatomy. From the overlay of the clinical photographs of the patient smiling, one can evaluate the new implant-supported, screw-retained fixed prosthetic as it relates to final esthetics, function, interocclusal room for strength, prosthetic soft-tissue smile line, high lip line, midline, lip support, buccal corridor, and occlusal plane to the established final VDO of the opposing dentition. This painstaking virtual process that highlights the skeletal TMJ in CR analysis, VDO, ostectomy, implant placement, cantilever forces, force factors, dental materials, and esthetics greatly increases predictability both in the short- and long-term stages of the patient’s dental health.
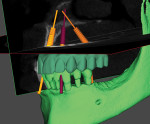
Once the multidisciplinary team has completed the virtual workup during the GTM using nSequence’s Maven Pro implant-planning software (Figure 3 and Figure 4), the case then goes into production to design the proprietary nSequence Guided Prosthetics that guide the entire treatment planning of the osteotomy, implant placement, and long-term provisional/final bridge. The proprietary stackable system allows the Bone Foundation Guide® (BFG; proprietary to author Llop) to be placed directly onto the bone after the teeth have been extracted and the soft tissue has been reflected (full-thickness flap required) (Figure 5 through Figure 7). It is important to note that the BFG does not rest on any portion of the patient’s soft tissue, as it is entirely bone-borne. Once the BFG with proprietary attached-removable clear teeth mock-up has been properly seated, the patient is then instructed to bite down onto the built-in occlusal stops, and the VDO, esthetics, and final seat of the BFG are evaluated and anchored with three pins into the patient’s bone horizontally.
Once the BFG is properly seated, the removable clear mock-up teeth are removed, exposing the deformed alveolar bone that was pre-planned for removal (osteotomy) to accommodate the dental implants and final prosthetics for strength and esthetics (Figure 8). The alveolar bone is then flattened as planned virtually, and the proprietary stackable surgical guide is placed onto the BFG. The dental implants are then guided to depth, trajectory, and rotation using the set of implant-guided surgical instruments (Figure 9). Once the implants are completely seated and noted to be in the correct rotation, the implant mounts are removed and the surgical guide is taken off the BFG. At this point, the bone is profiled away from the coronal aspect of the implants and the multiunit abutments, and temporary cylinders are seated so the proprietary silicon gasket can be placed over the multiunit abutments and temporary cylinders to close off any excess acrylic or cement leaking onto the alveolar bone and lock in the prosthetic. The proprietary gasket cradles the prosthesis in the pre-planned VDO/CR position so the practitioner can inject temporary or cement material into the holes on the facial and buccal aspects to afix the temporary cylinders to the prosthesis in the proper orthodontic position (Figure 10 through Figure 12). Once the long-term PMMA and milled support titanium provisional is “picked up,” the practitioner unscrews the long-term provisional and repeats the process with a second set of temporary cylinders and a clear duplicate record base (Figure 13). This eliminates the need for multiple appointments, such as the open-tray impression, screw-retained bite block, verification jig, and screw-retained try-in patient appointments. The clear duplicate record base includes all of the aforementioned and adds approximately 15 minutes to the prosthetic phase of the surgical appointment (ie, the second appointment).
The next appointment (ie, the third appointment) will simply be to deliver the final prosthesis or elect to try-in a mock-up before going to final (Figure 14 and Figure 15). This usually is to evaluate the final esthetics and VDO/CR and to pick up the resorbed tissue after healing. Generally, all that is necessary to complete treatment are three to four patient appointments.
Conclusion
By proactively taking the necessary time using the nSequence protocols to create the virtual dental patient during the record-taking process at appointment one, the results far outperform the conventional, reactive, semi-guided, or freehand techniques. Chairtime is greatly reduced as are the number of office visits, resulting in very happy patients. Furthermore, any time one can use the skills of a multidisciplinary team approach, accuracy and predictability are greatly increased, leading to a more competitive, cost-effective approach to full-arch, screw- or cement-retained implant-supported prosthetic rehabilitation.12,15-20 By using a proactive virtual approach to diagnosing and treatment planning full-arch immediate reconstruction cases, the treating clinician can analyze in advance the required important parameters, such as as TMJ, VDO/CR, bone quality, any required bone augmentation, precise implant placement, facial esthetics, force factors, and material choices before picking up a scalpel or handpiece.
References
1. Pikos MA, Magyar CW, Llop DR. Guided full-arch immediate-function treatment modality for the edentulous and terminal dentition patient. Compend Cont Educ Dent. 2015;36(2)116-128.
2. Schnitman PA. Ten-year result for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12:495-503.
3. Chow J, Hui E, Lee P, et al. Zygomatic implants—protocol for immediate loading: A preliminary report. J Oral Maxillofac Surg. 2006;64:804-811.
4. Zhao Y, Skalak R, Brånemark PI: Analysis of a dental prosthesis supported by zygomatic fixtures. The Institute for Applied Biotechnology, Gothenberg, Sweden, unpublished.
5. Bedrossian E. Immediate function with the zygomatic implant: A graftless solution for the patient with mild to advanced atrophy of the maxilla. Int J Oral Maxillofac Implants. 2006;21(6):937-942.
6. Brånemark PI. Introduction to Brånemark Novum concept. In: Brånemark P-I, editor. The Brånemark Novum protocol for same-day teeth. A global perspective. Berlin: Quintessenz; 2001.
7. Maló P, Rangert B, Nobre M. All-on-4 immediate-function concept with Brånemark system implants for completely edentulous maxillae: A 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S88-S94.
8. Malo P, de Araujo Nobre M, Rangert B. Implants placed in immediate function in periodontally compromised sites: a five-year retrospective and one-year prospective study [published correction appears in J Prosthet Dent. 2008;99(3):167]. J Prosthet Dent. 2007;97(6 suppl):S86-S95.
9. Khatami AH, Smith CR. “All-on-Four” immediate function concept and clinical report of treatment of an edentulous mandible with a fixed complete denture and milled titanium framework. J Prosthodont. 2008;17(1):47-51.
10. Malo P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark system implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):2-9.
11. Malo P, Nobre Mde A, Petersson U, Wigren S. A pilot study of complete edentulous rehabilitation with immediate function using a new implant design: case series. Clin Implant Dent Relat Res. 2006;8(4):223-232.
12. Malo P, de Araujo Nobre M, Lopes A. The use of computer-guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow-up period of thirteen months [published correction appears in J Prosthet Dent. 2008;99(3):167]. J Prosthet Dent. 2007;97(6 suppl):S26-S34.
13. McGarry TJ, Nimmo A, Skiba JF, et al. Classification system for complete edentulism. J Prosthodont. 1999;8:27-39.
14. Salinas T. Implant treatment and the edentulous maxilla. Pract Periodontics Aesthet Dent. 2004;6(3):247-248.
15. Rosenfeld AL, Mandelaris GA, Tardieu PB. Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 1: diagnostics, imaging, and collaborative accountability. Int J Periodontics Restorative Dent. 2006;26(3):215-221.
16. Pikos MA, Mattia AH. Implant surgery interventions: three dimensional reverse tissue engineering for optimal dental implant reconstruction. In: Jokstad A, ed. Osseointegration and Dental Implants. 1st ed. Ames, IA: Wiley-Blackwell; 2009:197-204.
17. Worthington P, Rubenstein J, Hatcher DC. The role of cone-beam computed tomography in the planning and placement of implants. J Am Dent Assoc. 2010;141(suppl 3):19S-24S.
18. Rosenfeld AL, Mandelaris GA, Tardieu PB. Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 3: stereolithographic drilling guides that do not require bone exposure and the immediate delivery of teeth. Int J Periodontics Restorative Dent. 2006;26(5):493-499.
19. Vrielinck L, Politis C, Schepers S, et al. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int J Oral Maxillofac Surg. 2003;32(1):7-14.
20. Sarment DP, Sukovic P, Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants. 2003;18 (4):571-577.
About the Authors
David Lee Hill, Jr., DDS
Oral Maxillofacial Surgeon
Private Practice
Chapel Hill, NC
Michael A. Pikos, DDS
Oral Maxillofacial Surgeon
Private Practice
Palm Harbor, FL
Founder
Pikos Institute
Trinity, FL
Daniel R. Llop, CDT
Inventor, nSequence® Guided Prosthetics™
Founder
nSequence Center for Advanced Dentistry
Reno, NV