The Dental Renaissance
Using art and science to restore function and esthetics in the edentulous patient.
By Wilson J. Kwong, DMD
Treating edentulous patients evolved recently with improved techniques, material science advances, and greater understanding of the physiological effects of tooth loss.1 Conventional prostheses provided little support to patients often suffering from loss of chewing efficiency, phonetics, collapse of vertical dimension, and the appearance of premature aging.1 Lost orofacial support also coincided with impaired oral function, pain, lack of retention, instability, and nutritional and psychological changes, including lowered self-esteem and altered self-image.2 Although prosthetic retention could potentially solve these issues, early attempts to fix metal framework-based prostheses to surrounding dentition did not provide long-term restorative stability, often leading to fractured abutment teeth, additional restorative work or tooth extraction.3
As dental professionals realized the need to address edentulous patients’ esthetic and functional demands, a renaissance in prosthetic dentistry occurred, ushering in a new standard of care.2 Combining the science of function and the art of esthetics, implant-supported fixed prostheses garnered greater acceptance.2 Although early attempts at implant placement failed to provide viable retention, new implant materials and techniques offer edentulous patients enhanced function and stability.2
Implant techniques and materials that osseointegrate reduce the loss of orofacial support caused by bone loss. Stability improves by placing two to four implants.2 Patients benefit from the support and comfort, since they no longer struggle to keep their prosthesis in place with their cheek, tongue, and gums.2 However, the mastication forces created by implant support—in addition to patient esthetic demands—required stronger framework materials and more lifelike denture teeth.3,4 Utilizing CAD/CAM technologies, all-ceramic frameworks composed of materials like zirconia offer improved strength and durability, while the addition of highly esthetic layering ceramics veneered on frameworks creates implant retained prostheses indistinguishable from surrounding dentition.3,4
Technique and Material Considerations
A variety of implant techniques, implant materials, and all-ceramics are available. Those selected should provide edentulous patients with optimal function and natural esthetics.
All-on-4
The All-on-4™ treatment concept (Nobel Biocare, www.nobelbiocare.com) provides an immediately loaded full-arch fixed dental prosthesis with four implants.5-8 Indicated for mandibular and maxillary arches, the All-on-4 concept improves stability, function, and comfort while preventing excessive bone loss.5-7
The technique can safely be used even when patients present with minimal bone volume.2 Two posterior implants are tilted to allow use of longer implants when there is minimum bone volume.6,9 When the implants are tilted and longer, bone-to-implant contact is improved, without negatively affecting load distribution,6,9 which reduces the need for vertical bone augmentations.6,9 The technique enables dentists or surgeons to anchor the implants in higher quality anterior bone to reduce cantilevers and improve prosthesis support.6,9
The All-on-4 technique benefits patients by allowing immediate-supported restorations.6-8 Provisional prostheses can be screwed onto the implants directly after surgery.6-10 The technique also selection from various dental prostheses for cost-effective and beneficial solutions, including implant bridges with acrylic or ceramic veneering, overdentures, and implant bar overdentures.
NobelReplace Implants
The implant surface design and composition is crucial to stability, functionality, and biocompatibility. NobelReplace implants (Nobel Biocare) are ideal for single-tooth restorations, fixed partial dentures, full arch fixed and removable solutions, and implant bridges. NobelReplace performs well in soft and hard bone, one- or two-stage procedures, flapless and flapped surgeries, and immediate and delayed loading procedures.11 NobelReplace implants can be utilized in all indications, especially the esthetic zone where bone ridges are typically thin.10,12 NobelReplace implants allow clinicians to redirect the implant during placement to ensure maximum flexibility.11,13-15
Created with a unique tip and thread design, NobelReplace implants improve osseointegration by incorporating a specially formulated biomaterial (TiUnite, Nobel Biocare) and surface texture (Groovy).12-17 The implant surface accelerates osseointegration compared to other implant designs with a machined surface.11,13 The macroscopic surface grooves along the implant operate in conjunction with the TiUnite surface to encourage bone development on the implant surface.11,13 NobelReplace implants may be used to develop a broad range of NobelProcera CAD/CAM (Nobel Biocare) prosthetics.14-17
IPS e.max Ceram
All-ceramic frameworks layered with highly esthetic ceramic materials enable fabrication of dental prostheses with improved durability, function, and longevity that meet patients’ esthetic demands.16
IPS e.max® Ceram (Ivoclar Vivadent Inc., www.ivoclarvivadent.us) was specifically developed for layering over high-strength implant and dental prosthetic frameworks composed of lithium disilicate (IPS e.max) or zirconia that have been pressed or CAD/CAM fabricated.18 To simplify the layering process, only one layering ceramic is required for both glass-ceramic and zirconium-oxide materials.18 All veneered IPS e.max Ceram restorations exhibit similar wear properties and surface gloss regardless of the framework material selected.18 The material offers high bond strength to zirconia and lithium-disilicate cores and frameworks to ensure stability and longevity.19
IPS e.max Ceram mimics natural dentition with exact shade matching.20,21 The material masks dark backgrounds caused by tooth, core, or framework color.20,21 IPS e.max Ceram also incorporates nano-fluorapatite to improve color parameters, luminosity, and translucency of veneered all-ceramic restorations and prostheses.20,21
IPS e.max Ceram is indicated for characterization and/or veneering of all IPS e.max component materials, layered veneers on zirconia frameworks, and designing gingival segments in implant-retained restorations or dental prostheses.
Case Presentation
A 79-year-old woman presented with a previously fitted cast partial denture with broken clasps and the major complaint of pain in her maxillary arch (Figure 1). A preoperative panoramic radiograph and clinical photographs were taken, from which it was apparent that her upper lip was largely unsupported and had subsequently shrunk over time (Figure 2 and Figure 3). The remaining abutment teeth demonstrated fractures and recurrent decay. The patient’s mandibular anterior dentition remained in good condition.
Treatment Plan
To correct function, esthetics, and relieve the patient’s pain, a comprehensive treatment plan was discussed and agreed upon with the patient. The failing upper abutment teeth would first be extracted and implants (NobelReplace Tapered Groovy) immediately placed using the All-on-4 technique. A sinus lift allograft and connective tissue grafts would also be completed while the healing and cover screws were in place.22
To restore function and esthetics, a 12-unit implant bridge would be fabricated from a CAD/CAM yttrium-stabilized zirconium-oxide block and layered with highly esthetic veneering ceramic (IPS e.max Ceram). Zirconia and ceramic were chosen to provide a better fit and finish than conventional acrylic denture materials. Soft-tissue response to ceramic materials is typically greater compared to acrylic restoratives, because ceramics demonstrate higher polishability and an overall smoother surface. Ceramics also provide excellent optical qualities and are esthetically superior to conventional acrylics.
Clinical Protocol
Before extraction, the tooth shade was determined to aid in fabricating the definitive zirconia implant bridge. The teeth were then extracted and implants were immediately placed using the All-on-4 technique. The healing and cover screws were placed, and an allograft sinus lift and soft tissue grafts were completed (Figure 4). After all of the surgical procedures, the patient was dismissed to allow healing and osseointegration.
Six months after implant placement, the patient returned for the second stage of treatment. Healing abutments were placed on the maxillary left and right molar implants. Open tray impressions were taken of both arches (Figure 5). Models were poured, the case was waxed-up, and a verification jig with non-engaging cylinders was fabricated.
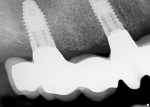
During jig fabrication, the patient’s central incisors were mocked-up with cold-cure acrylic and secured to the jig to verify the incisal edge position and midline on the model. The jig was transferred to the mouth and radiographs were taken to verify fit. A bite registration was taken to ensure proper vertical and anterioposterior positioning. A stick bite was also taken to confirm the horizontal positioning of the maxillary set-up.
Using these records, the verification jig was evaluated to ensure proper fit, function, and esthetics (Figure 6). Although fabrication of the verification jig is often completed in two separate appointments, it was completed in one in this case.
Once the verification jig was complete, the restoration wax-up was tried-in to reconfirm fit, esthetics, and provide the patient with a “trial smile” on the same day (Figure 7). To reconfirm the horizontal position of the dentition, a new horizontal stick bite was taken with the trial wax-up in place (Figure 8). All diagnostic information, including clinical photographs, was then used in the in-house laboratory to fabricate a cut-down model that was then scanned for creation of the ceramic-layered zirconia implant bridge.
Laboratory Protocol
The implant bridge was mocked-up in wax and placed on the articulator in preparation for scanning with a high accuracy three-dimensional CAD/CAM scanning (Optimat 3D scanner, NobelBiocare). After creating a copy of the set-up, the wax was cut back to ideal dimensions and then scanned. After scanning, the zirconia 12-unit bridge was designed and milled with the CAD/CAM system (NobelProcera). The completed bridge was scrutinized against the substructure mock-up to ensure the proper dimensions were obtained. Upon confirmation of proper size and characterization, the 12-unit zirconia implant bridge was placed on the model. The zirconia 12-unit bridge was designed and milled with the CAD/CAM system (NobelProcera), then scrutinized against the mock-up to ensure accuracy and placed on the model (Figure 9). Because of the implant position and angulation, a lithium-disilicate crown (NobelProcera e.max CAD) was required on the maxillary right canine. The model and zirconia substructure were scanned, the crown designed and milled from a lithium-disilicate block (IPS e.max CAD), and the milled restoration layered with veneering ceramic (IPS e.max Ceram) in the necessary Essence and Shade materials. Although an angled abutment could have been used, crown placement was simpler and more cost-effective for the patient.
Ceramic Layering
Once the crown was complete, the 12-unit zirconia bridge was layered with a highly esthetic ceramic veneering material. The zirconia bridge was cleansed with water and air-dried to remove contaminants. To prevent surface damage, the framework was not blasted with aluminum particles or with the polishing jet on medium.
Before layering, the specialized liner material (ZirLiner, Ivoclar Vivadent) was mixed to a creamy consistency, and a thin layer applied to the entire framework to ensure a sound bond, depth of color, and fluorescence. During application, the margins were sufficiently covered and the entire framework appeared green. The liner was allowed to briefly dry and then fired, after which it demonstrated a thickness of approximately 0.1 mm.
The veneering process began by conducting a wash firing of dentin ceramic material to control veneering material shrinkage and ensure a homogeneous bond to the underlying liner material. After confirming the entire zirconia framework surface was covered, the restoration was placed on the firing tray and fired.
Before additional layering, model sealer (IPS Model Sealer, Ivoclar Vivadent) was placed on the model before additional layering and allowed to dry. Corresponding areas were isolated with separating liquid (IPS e.max® Ceramic Separating Liquid, Ivoclar Vivadent), and the zirconia framework was placed on the model. The required shade of veneering ceramic was mixed with the necessary build-up liquids on the mixing pad. To prevent the organic components from accumulating, distilled water was used to rewet the layering materials as necessary.
The pontics were layered with the next lighter shade of Deep Dentin, ensuring the necessary thickness was achieved. After layering the pontic areas with the lighter shade of dentin, they were layered with Deep Dentin and other Dentin shades. Once the entire dentin core was layered, the desired Occlusal Dentin shade was applied to complete the occlusal surfaces. The completed dentin layers were carefully reduced to provide sufficient space for incisal layers. To further characterize the restoration, Transparent and Impulse materials were applied, which were then covered with the desired shades of Incisal veneering ceramic. In addition, a pink-layered porcelain was used to create a shade match to the existing gingiva.
After the incisal layers were applied, the implant bridge was removed from the model, contact points were supplemented, and all interproximal spaces separated down to the framework. The layered zirconia framework was fired, then cleansed in an ultrasound water bath and thoroughly dried. Using layering ceramics, incomplete or missing areas were corrected, specifically in the interdental areas and contact points, and the restoration was fired.
Before stain and glaze firing, the restoration was finished and polished with finishing diamonds to ensure a natural shape and surface structure. Natural characterizations were created and smoothed where necessary using the diamonds. To prevent discoloration during firing, the restoration was thoroughly cleaned with the steam jet and evaluated to ensure that all contaminants were removed.
An even layer of the desired shade of glaze was carefully applied to the entire restoration, focusing on the basal and pontic areas. The fissures were characterized with the desired Essence stain, and contact points were supplemented with a 1:1 mixture. The supplemented areas were polished to high gloss with a silicone polisher. After glazing and staining, any required adjustments were made and the restoration was fired. The restoration was placed on the model to confirm fit, function, and esthetics, after which the case was ready for delivery to the patient for final seating (Figure 10 and Figure 11).
Seating
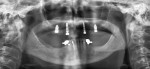
The zirconia implant bridge was seated in the patient’s mouth, and periapical films confirmed proper fit. Panorex radiographs demonstrated anatomical structures (Figure 12 and Figure 13). The crown and zirconia implant bridge screw access hole was filled with polyvinyl siloxane material (Figure 14). The crown was temporarily cemented in place using transparent temporary cement (Teliolink, Ivoclar Vivadent) while the abutment screws were torqued to 35 Ncm and covered with flowable composite (Tetric EvoFlow, Ivoclar Vivadent) (Figure 15). The composite was then light-cured (Demetron, Kerr Corporation, www.kerrdental.com).
Upon completion, the 12-unit ceramic-layered zirconia bridge, with a lithium-disilicate crown on the maxillary right canine abutment, appeared lifelike and blended well with the surrounding dentition (Figure 16, Figure 17 and Figure 18). Returning for the follow-up appointment 8 months later, the patient was extremely pleased with the function and form of her new fixed partial restoration and had gained 8 pounds, since she could now eat without experiencing pain. The crown that had been temporarily cemented with a “soft” cement for retrievability was now removed, cleaned, and then bonded on with a “hard” cement (Multilink, Ivoclar Vivadent) after the patient confirmed comfort with the prosthesis.
Conclusion
Through advancements in material science and improvements to techniques, the dental industry is on the threshold of a renaissance-like understanding of providing optimal care to edentulous patients.2 By using an advanced implant technique and design, CAD/CAM technology, and highly esthetic ceramic layering material over an all-ceramic bridge, dentists and technicians can provide patients with stable and durable dental prostheses that appear indistinguishable from the surrounding dentition. The case demonstrated here reflects a combination of functional science and ceramic artistry that satisfies the stability, strength, and esthetic demands of today’s patients.2
Acknowledgment
The author wishes to thank his ceramist, Mr. Seiji Ato (from Tokyo, Japan) at Oakridge Esthetic Dental Studio for fabricating the restorations in this case.
References
1. Fiske J, Davis DM, Frances C, et al. The emotional effects of tooth loss in edentulous people. Br Dent J. 1998;184(2):90-93.
2. Vogel RC. Implant overdentures: a new standard of care for edentulous patients–current concepts and techniques. Compend Contin Educ Dent. 2008;29(5):270-278.
3. Henry K. Q&A on the future of implants. Dent Equip Mater. September/October 2006.
4. Rossein KD. Alternative treatment plans: implant-supported mandibular dentures. Inside Dentistry. 2006;2(6):42-43.
5. Onodera K, Sato T, Nomoto S, et al. Effect of connector design on fracture resistance of all-ceramic fixed partial dentures. Bull Tokyo Dent Coll. 2011;52(2):61-67.
6. Agliardi E, Panigatti S, Clericò M, et al. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: interim results of a single cohort prospective study. Clin Oral Implants Res. 2010;21(5):459-465.
7. Malò P, Nobre Mde A, Lopes I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: a pilot study. J Prosthet Dent. 2008;100(5):354-366.
8. Malò P, de Araújo Nobre M, Lopes A, et al. A longitudinal study of the survival of all-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011;142(3): 310-320.
9. Cehreli S, Ozçipici AA, Yilmaz A. Tilted orthodontic micro implants: a photoelastic stress analysis. Eur J Orthod. 2010 July 11. [Epub ahead of print].
10. Malò P, Rangert B, Nobre M. All-on-4 immediate-function concept with Brånemark system implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005; 7(Suppl 1):S88-S94.
11. Malò P, Friberg B, Polizzi G, et al. Immediate and early function of Brånemark system implants placed in the esthetic zone: a 1-year prospective clinical multicenter study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):37-46.
12. Cosyn J, Eghbali A, De Bruyn H. Single implant treatment in healing versus healed sites of the anterior maxilla: An aesthetic evaluation. Clin Implant Dent Relat Res. 2010 Jul 17. [Epub ahead of print].
13. Malò P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Branemark system implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 (Suppl 1):2-9.
14. Malò P, Nobre Mde A, Petersson U, et al. A pilot study of complete edentulous rehabilitation with immediate function using a new implant design: case series. Clin Implant Dent Relat Res. 2006;8(4):223-232.
15. Babbush CA, Kutsko GT, Brokloff J. The All-on-Four immediate function treatment concept with NobelActive implants–a retrospective study. J Oral Implantol. 2011;37(4): 431-445.
16. Kielbassa AM, Martinez-de Fuentes R, Goldstein M, et al. Randomized controlled trial comparing a variable-thread novel tapered and a standard tapered implant: interim one-year results. J Prosthet Dent. 2009; 101(5):293-305.
17. Irinakis T, Wiebe C. Initial torque stability of a new bone condensing dental implants. a cohort study of 140 consecutively placed implants. J Oral Implantol. 2009;35(6):277-282.
18. Kielbassa AM, Martinez-de Fuentes R, Goldstein M, et al. Randomized controlled trial comparing a variable-thread novel tapered and a standard tapered implant: interim one-year results. J Prosthet Dent. 2009;101(5):293-305.
19. Ivoclar Vivadent. IPS e.max Ceram: Instructions for Use. (2009). [Brochure]. Amherst, NY.
20. Ishibe M, Raidgrodski AJ, Flinn BD, et al. Shear bond strengths of pressed and layered veneering ceramics to high-noble alloy and zirconia cores. J Prosthet Dent. 2011;106(1):29-37.
21. Aboushelib MN, Dozic A, Liem JK. Influence of framework color and layering technique on the final color of zirconia veneered restorations. Quintessence Int. 2010;41(5): e84-e89.
22. Luo XP, Zhang L. Effect of veneering techniques on color and translucency of Y-TZP. J Prosthodont. 2010;19(6):465-470.
About the Author
Wilson J.Kwong, DMD
Cosmetic & Restorative Dentistry
Vancouver, British Columbia, Canada
Director
Vancouver Dental Education Centre
Burnaby, British Columbia, Canada
Program Director
California Center for Advanced Dental Studies
Pleasanton, California