The Details of Team Communication: A Case Study Report
Nasser Barghi, DDS, MA; Elaheh Mohebzad, DDS; Rene C. Aguirre
The multidisciplinary approach is a team effort focused on accomplishing a specific task using various entities, disciplines, and manpower. The nature of the task may dictate the size of the team and the degree of involvement of each member. The micromanagement of a task assigned to a member is often left to the individual while the main focus is directed toward the final outcome. Communication between restorative dentists and ceramists mainly includes (but is not limited to): the type of restoration, design of the restoration, shade information, impression, smile design, form, margins, and occlusion. Details are left to the individual to decide at his/her discretion. Rarely a restorative dentist is interested in knowing the firing temperature of the porcelain, numbers of firing, or the investment materials used. Advancements and expansion in restorative materials, laboratory techniques, and information technologies have made this detail information voluminous and laborious to collaborate on unless ceramists and dentists work in very close proximity.
Both dentists and ceramists rely on instructional information for using materials. In the absence of detailed information and instruction, one may use previous knowledge or general information to use a specific material. Instructions are more often read when the expected outcome is not reached. In spite of efforts to provide patients with durable restorations, unexpected and less desirable clinical outcomes occasionally occur. Bonding a debonded veneer without searching for the cause of debonding is an anecdotal approach to the problem.
Porcelain veneers bonded to etched enamel provide the most durable restorations with more than a 93% survival rate over 15 years of clinical observation.1-4 These observations overwhelmingly support the conservative nature of porcelain veneers bonded to enamel as a key to the success of these unique and durable restorations. In vitro examination and long-term in vivo observation have further proved their esthetics and longevity. Several steps involving the surface treatment of porcelain, such as etching and silanization, as well as steps involved in bonding ceramic veneers have been explored and researched fully but are not widely used.5-7 Proper surface treatment of porcelain before bonding to enamel is fundamental to achieving a durable porcelain-composite bond.6 Having knowledge of the microstructure of porcelain (ie, pressed, high-leucite, medium-leucite, and low-leucite), types and concentration of etchants (ie, hydrofluoric acid gel, fluoride liquid, or ammonium bifluoride), and, finally, silane and silanization is critical for both dentists and ceramists.5-8 Excessive sandblasting before etching, failure to remove the crystalline residue after etching, and failure to eliminate nonreactive organic contaminants after silanization have an irreversible effect on the porcelain-composite bond.6-8 Inconsistency exists between manufacturers’ instructions for using similar materials, ie, ceramic etchants, silane, and other surface treatments.6 A careful analysis of unexpected clinical outcomes and a willingness to communicate and discuss failures as well as successes is empirical to make further progress.
This case presentation is an example of a multidisciplinary team approach where the desired outcome was not reached as planned and unexpected problems arose. Lessons were learned to expand the degree of communication with ceramists and the need to implement a well-defined protocol based on sound research for surface treatment before bonding.
Case Study
Abstract Report
A 47-year-old Hispanic woman, who was treated orthodontically and then restored with four maxillary incisor ceramic veneers, was referred with the chief complaint of multiple debondings 4 weeks after placement. It was revealed that the veneer placed on tooth No. 8 debonded 2 weeks after placement, was retrieved by the patient, and was rebonded by the restorative dentist. The veneer on tooth No. 7 debonded at 4 weeks after placement. The patient was content, but not overwhelmed, with the appearance of the veneers. Initial examination of the site revealed that the debonding of the veneer on tooth No. 7 took place adhesively at the porcelain interface. This observation was further confirmed by visual examination of the bonding surface of a debonded veneer that was devoid of luting resin with a trace of marginal leakage. Although the incident of debonding and rebonding of the ceramic veneer placed on tooth No. 8 was recorded in the patient’s chart, the debonded interface was not revealed.
Two debonded veneers, 2 weeks apart and 4 weeks after placement, were sufficient reason to further examine the status of the two veneers still in place (teeth Nos. 9 and 10). Tissue around the gingival margin was slightly inflamed interproximally. Marginal adaptation of the veneers was not clinically acceptable because there was evidence of microleakage. The remaining two veneers (teeth Nos. 9 and 10) became debonded upon finger manipulation with moderate twisting force exerted at the incisal edge of the restorations. Visual observation of the site revealed adhesive failure at the ceramic interface. Luting resin remained on the prepared teeth, while the bonding surface of debonded veneers appeared free of resin.
Faced with four debonded veneers, three at the porcelain interface and one debonded/rebonded veneer (unknown interface), a task was developed to examine the full history of this case and further analyze the debonded sites of veneers with scanning electron microscopy (SEM) before making any attempt to provide the patient with a new set of ceramic veneers.
Clinical History
Initially the patient was referred to the Advanced Education General Dentistry (AEGD) Clinic with the chief complaint of long upper canines, negative smile line, excessive show of lower anterior teeth, and minimal display of upper anterior teeth. A history of lemon sucking was evident from the enamel pitting of the maxillary incisors (Figure 1). Incisal wear was present on both maxillary and mandibular incisors likely caused by mild bruxism as confirmed by the patient. The patient was referred to and treated by an orthodontic resident before restoration with porcelain veneers by the restorative dentist. Two sets of veneers were fabricated; the first set was rejected by the patient and the second set was cemented, but bonding failures occurred as described. The patient then was referred to the Esthetic Dentistry Division for the third set of ceramic veneers.
Treatment Analysis
Having access to the full written documentation of the case made by AEGD restorative dentists and orthodontic residents, as well as cephalometric evaluation, radiographs, preoperative casts, and more than 100 images, it was possible to reassemble and fully analyze the case before making any attempt to provide the patient with the third set of ceramic veneers.
The patient presented as a class I skeletal, class I dentition, orthognathic and pleasing profile with mild 1-mm mandibular crowding and 3-mm maxillary spacing (Figure 2, Figure 3, and Figure 4). Incisal wear was present on both maxillary and mandibular anterior teeth, and the facials of the maxillary centrals presented with enamel pitting. The patient’s primary concern was the reverse smile line and the irregular gingival architecture. Overjet and overbite were 4 mm and 3 mm, respectively. Maxillary and mandibular midlines presented relatively centered with the facial midline, although a small Bolton’s tooth size discrepancy was measured with slightly excess mandibular anterior tooth mass.
Esthetically, the patient’s incisor display in repose was appropriate (3 mm) while there was 0 mm of gingival display of incisors on full smile. Request for orthodontic treatment before veneering included: redistribution of the spaces in the upper dentition, leveling of the upper arch, as well as leveling and aligning the lower dentition. A primary goal of orthodontic treatment was to level the maxillary arch with mostly canine intrusion with some mild relative incisor extrusion. Bite turbos were used on the maxillary canines to assist with leveling.
Initially, the patient was treated orthodontically for a total of 20 months, during which multiple consultations with AEGD restorative dentists were accomplished to refine the pre-restorative outcome. Orthodontic treatment was completed with 1 mm of overbite, allowing for the restoration of the incisal edges of the maxillary incisors (Figure 5). The maxillary midline was slightly to the right after orthodontic treatment. This was deemed within the range to be corrected with porcelain veneers. Spaces between teeth Nos. 5 and 6 as well as Nos. 11 and 12 were closed and distributed among the maxillary incisors (Figure 6, Figure 7, and Figure 8). Additional intrusion of the mandibular incisors would have been ideal. Superimposition of lateral cephalograms showed that the orthodontic result was 1 mm to 1.5 mm of maxillary and mandibular incisor intrusion; however, the patient may have benefited from more bite opening before restoration (Figure 9). Overall, the orthodontic results were satisfactory for initiating the restorative treatment.
Restorative Treatment
After orthodontic treatment, the patient was returned to the AEGD restorative dentist for veneering of the maxillary incisors. The teeth were prepared on enamel with margins placed slightly subgingivally (Figure 10). Four feldspathic ceramic veneers were fabricated and tried in (Figure 11). The first set of veneers were found totally unacceptable to the restorative dentist and the patient for the following reasons: monochromatic appearance, improper contour, improper anatomy, improper smile design, improper shade, and improper embrasures. A new impression was obtained and the second set of veneers was fabricated by the same ceramist. Although the new veneers showed improvement in shade, design, contour, and anatomy, they were far short of ideal (Figure 12). The patient reluctantly accepted the second set of veneers and they were bonded.
Two weeks after bonding, the patient returned with a debonded ceramic veneer from tooth No. 8 in her hand. The site of debonding (tooth or porcelain) was not recorded in the daily treatment. Both debonded interfaces (tooth and porcelain) were cleaned, and the veneer was rebonded. At 4 weeks after initial cementation, the veneer on tooth No. 7 debonded (Figure 13). The patient returned with the debonded veneer. She was referred to the Division of Esthetic Dentistry for further assessment of the remaining veneers and placement of new veneers if necessary. Visual evaluation of the sites revealed debonding at the porcelain interface. The tooth-surface preparation was covered with luting resin (Figure 14). No trace of resin was found on the bonded surface of the veneer. Bonded veneers on teeth Nos. 9 and 10 were further examined for marginal adaptation, gingival response, and retention. The two veneers became debonded with moderate finger pressure exerted at the incisal edges and at the gingival margins when scaling force was applied with a Discoid-Cleoid UW-D5 (American Eagle Instruments, Inc, Missoula, MT). The debonded sites (tooth and porcelain) were visually examined. Once again, the enamel preparations were found covered with luting resin, with no trace of resin on the bonding surfaces of the two veneers (adhesive failure at the porcelain interface) (Figure 15 and Figure 16).
SEM Evaluation of Debonded Sites
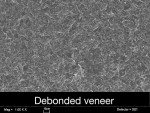
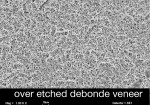
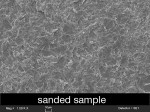
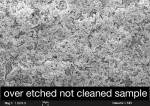
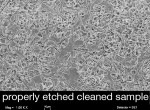
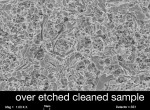
The three debonded veneers were mounted, coated, and examined under SEM at 1,000x magnification. SEM examination of the debonded veneer from tooth No. 7 revealed a sandblasted, divested surface with no evidence of ceramic etching (Figure 17). On the contrary, examination of the debonded veneers from teeth Nos. 9 and 10 showed evidence of over-etched porcelain covered with crystalline and a salts residue (Figure 18). To support this observation, three samples (10 mm x 10 mm x 12 mm) of a medium-leucite content porcelain (Ceramco® II, DENTSPLY Ceramco, Burlington, NJ) were prepared: one sanded with 50 µm Al2O3 at 30 psi, one etched for 2 minutes, and one etched for 5 minutes (Figure 19).
Samples were visually examined, steam cleaned, mounted, and viewed under SEM. Photomicrographs were obtained and compared with images taken from the debonded sites. Figure 20 depicts a view of the sanded sample. Note the close similarity between this photomicrograph and the one obtained from the veneer from tooth No. 7 (Figure 17). Figure 21 shows a 5-minute etched but not steamed-cleaned porcelain sample. Comparison of this image with images taken from the debonded, over-etched veneer reveals the presence of excess residue covering the entire over-etched surface. As evident from this figure, an over-etched surface traps and retains various residue and crystalline fragments. Steam cleaning appears to remove all residue, leaving the over-etched surface free of debris (Figure 22 and Figure 23).
Final Restoration
Final preparation involved the removal of luting resin from teeth Nos. 7, 9, and 10 as well as removal of the rebonded veneer on tooth No. 8. This veneer was not as easily debonded as the other veneers. It was removed by grinding with a diamond bur. Margins were reestablished and provisionalized with composite resin. Final veneers were fabricated with a high-leucite content stacked porcelain and bonded with a 100% light-cure luting resin (Choice™ 2 LC, Bisco, Inc, Schaumburg, IL). The patient was very satisfied with the final esthetic outcome (Figure 24 and Figure 25).
Discussion
This multidisciplinary case is an example of a well-planned esthetic treatment where unanticipated problems that could have been simply avoided resulted in two remakes. It also prolonged and postponed the expected outcome. The subjective nature of esthetic restorations and unexpected technique-related problems, such as open margins and occlusion, often necessitate a total or partial remake. In this clinical case, the shortcomings of orthodontic treatment were corrected restoratively, which is a common practice when an esthetic treatment involves both disciplines. The first set of veneers failed to meet the desired outcome for numerous esthetic and functional inadequacies. The second set of veneers showed an improvement over the first set, yet did not meet the desired esthetic outcomes based on the principles of form, function, anatomy, and color. In spite of the shortcomings, the patient expressed interest in the second set. It was a compromised outcome, but as one may say, beauty is in the eye of the beholder. Multiple debondings of restorations 4 weeks after placement is rarely observed or reported when the standard protocol for bonding ceramic veneers is properly followed.
The two important surface treatments of porcelain (etching and silanization) play a very important role in the composite-porcelain bond.6-8 An etched porcelain surface is hydrophilic with high surface energy. It has an affinity for contamination that is not easy to fully clean.9,10 The reactive surface of silane also may become nonreactive if the silanated porcelain is contaminated.11,12 Etching porcelain with 9.5% hydrofluoric acid gel for 1 to 2 minutes depending on the leucite content of porcelain will result in a maximum retentive surface.13 Silane is a wetting agent that provides a covalent bond.14,15 It is most effective when applied in monolayer. In the absence of etching porcelain, studies have shown that proper silanization of porcelain provides a strong porcelain-composite bond.16 The use of a two-part silane is strongly suggested by these and other authors.6,16,17 A one-part silane may undergo condensation if it is not used in the specified shelf-life.17,18 The method of application of silane is dictated by the types of solvent (acetone vs ethanol). Failure to remove the nonreactive surface caused by excess use of silane or inadequate cleaning before bonding may result in debonding of the veneer at the porcelain interface.6,14 Because of the technique sensitivity of etching and silanization of porcelain, these and other authors strongly recommend that both surface treatments be performed by dentists after try-in of porcelain and before bonding.5,6
It is impossible to visually differentiate between a sanded veneer, an adequately etched veneer, and an overly etched veneer13 if the latter is steam cleaned. The adverse effect of over-etching of porcelain on the porcelain-composite bond has been reported in the literature.13,19,20 Over-etching of porcelain results in formation of a salt (hexafluorosilicate) and crystalline residue, which covers the etched surface. These residues have been shown to interfere with bonding composite resin to etched ceramic.6,7 One study showed a 50% reduction in porcelain-composite bond when post-etching residues were not removed.21 Scrubbing the etched surface with a brush and phosphoric gel followed by ultrasonic cleaning for 4 to 5 minutes has been suggested as an effective method of cleaning the etched porcelain surface.7 Observation in this case study reports steam cleaning of the etched surface was very effective in removing residues. Special caution should be exercised when an etched porcelain veneer is subjected to steam cleaning because it may result in fracture of ultrathin veneers or accidental loss caused by the force of discharged steam.
Conclusion
Regardless of the nature of bonded substructure (enamel, dentin, or porcelain), proper surface treatment of porcelain and proper isolation is paramount to achieving a durable and lasting bond. In spite of broad inconsistencies among different manufacturers’ instructional materials for ceramists and dentists regarding proper surface treatment of bonded surfaces, there are well-conducted in vitro studies that can be used as guidelines and protocols for bonding etched ceramic restorations. Developing a joint dentist/ceramist protocol for proper surface treatment of porcelain before bonding is paramount. This includes sanding with 30-µm aluminum oxide at 20 psi to 30 psi, adequate etching with hydrofluoric acid gel based on the concentration of the etchant and the leucite content of porcelain, proper cleaning of the etched surface, and correct silanization.
References
1. Strassler HE, Weiner S. Seven- to ten-year clinical evaluation of etched porcelain veneers [abstract]. J Dent Res. 1995;74(Spec Iss): 176;1326.
2. Strassler HE, Weiner S. Long-term clinical evaluation of etched porcelain veneers [abstract]. J Dent Res. 1998;77(Spec Iss A):1017.
3. Friedman, MJ. A 15-year review of porcelain veneer failure—a clinician’s observations. Compend Contin Educ Dent. 1998;19(6): 625-638.
4. Nathanson D, Strassler HE. Clinical evaluation of etched porcelain veneers over a period of 18 and 42 months. J Esth Dent. 1989;1(1):21-28.
5. Barghi N, Overton JD. Preserving principals of successful porcelain veneers. Contemporary Esthetics. 2007;11(1): 48-51.
6. Alex G. Preparing porcelain surfaces for optimal bonding. Functional Esthetics and Restorative Dentistry. 2008;2(1):38-49.
7. Magne P, Cascione D. Influence of post-etching cleaning and connecting porcelain on the microtensile bond strength of composite resin to feldspathic porcelain. J Prosth Dent. 2006;96(5):354-361.
8. Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosth Dent. 2003;89(3):268-274.
9. Swift B, Walls AWG, McCabe JF. Porcelain veneers: the effects of contaminants and cleaning regimens on the bond strength of porcelain to composite. Brit Dent J. 1995; 179(6):203-208.
10. Aboush YE. Removing saliva contamination from porcelain veneers before bonding. Prosth Dent. 1998;80(6):649-653.
11. Soares CJ, Soares PV, Pereira JC, et al. Surface treatment protocols in the cementation process of ceramic and laboratory-processed composite restorations: a literature review. J Esthet Restor Dent. 2005;17(4): 224-235.
12. Suh BI. All-bond—fourth generation dentin bonding system. J Esth Dent. 1991;3(4): 139-147.
13. Barghi N, Fischer DE, Vatani L. Effects of porcelain leucite content, types of etchants, and etching time on porcelain-composite bond. J Esth Res Dent. 2006;18(1):474-53.
14. Rosen MR. From treating solution to filler surface and beyond—the life history of a silane coupling agent. J Coat Technol. 1978; 50(644): 70-82.
15. Anagnostopoulos T, Eliades G, Palaghias G. Composition, reactivity and surface interactions of three dental silane primers. Dent Mater. 1999;9(3):182-190.
16. Barghi N. To silanate or not to silanate: making a clinical decision. Compend Contin Educ Dent. 2000;21(8): 659-666.
17. Nguyen R, Barghi N. Duration of efficacy of a two-mix silane following activation [abstract]. J Dent Res. 2001;80(Spec Iss):529.
18. Daniels MW, Francis LF. Silane absorption behavior, microstructure, and properties of glycidoxypropyltrimethoxysilane-modified colloidal silica coatings. J Colloid Interface Sci. 1998;205:191-200.
19. Stangel I, Nathanson D, Hsu CS. Shear strength of the composite bond to etched porcelain. J Dent Res. 1987;66(9):1460-1465.
20. Blatz MD, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003;89(3):268-274.
21. Canay S, Hersek N, Ertan A. Effect of different acid treatments on a porcelain surface. J Oral Rehabil. 2001;28(1):95-101.
About the Authors
Nasser Barghi, DDS, MA
Professor, Department of Restorative Dentistry
University of Texas Health Science Center—San Antonio
San Antonio, Texas
Elaheh Mohebzad, DDS
Advanced Orthodontic Resident, Department of Orthodontics
University of Texas HealthScience Center—San Antonio
San Antonio, Texas
Rene C. Aguirre
Research Assistant, Department of Restorative Dentistry
University of Texas HealthScience Center—San Antonio
San Antonio, Texas