Simplifying the Workflow for Direct Posterior Restorations
Composite system and high-intensity curing light increase efficiency and predictability
Jason Olitsky, DMD
One of the most frequently performed procedures in dental practices is the treatment of posterior carious lesions with light-cured, tooth-colored direct composite restorative materials.1 The goals of this conservative treatment approach are to preserve as much natural tooth structure as possible, remove the carious tissue, and seal the tooth to prevent recurrent decay. Tooth-colored filling materials provide an esthetic option for patients, but they have traditionally come at a cost regarding efficiency. Direct composite restorative protocols are often time-consuming and can involve a multitude of technique-sensitive steps that require proper isolation of the operative site.2-4 Incomplete photopolymerization of the incrementally placed composite layers is the most common source of error in direct restorative treatments; therefore, proper light curing is of critical importance to prevent postoperative sensitivity and marginal leakage as well as to achieve an optimal color match.5-7
Optimizing treatment time without sacrificing ideal material placement requires innovation in direct composite monomer technology, photoinitiators, and light-emitting diode (LED) curing technology. Thankfully, the almost constant innovation from dental manufacturers is now providing dentists with more efficient, simplified workflows that yield optimal and predictable results. When choosing a direct restorative system, clinicians should consider void-free systems that offer esthetic and long-lasting results and, most importantly, systems that can be employed efficiently with little to no postoperative sensitivity.
Case Report
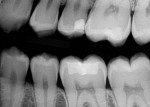
A 27-year-old female patient presented to the dental office for an occlusal surface restoration on her lower left first molar (ie, tooth No. 19). She had several posterior Class I and Class II restorations that had been placed by previous practitioners. During her initial examination, occlusal decay was detected in the tooth (Figure 1), and it was determined that in order to restore it in a conservative and minimally invasive manner, direct composite would be the modality of treatment.
The patient was anesthetized, and a rubber dam (Latex Black Dental Dam, Sanctuary) was placed to achieve isolation. First, a carbide bur was used to remove the occlusal carious material, followed by a diamond bur to even the cavosurface margins. Next, a round bur was used to excavate the deepest portion of the decay. In the final preparation step, a diamond bur was used to smooth and refine the angles of the preparation and also provide a slight bevel for the esthetic integration of the direct restorative.
Once the preparation design was comple-ted, the dentin and enamel were particle abraded (PrepStart™ Air Abrasion Unit, Zest Dental Solutions) with 40-µm aluminum oxide, which homogenizes the dentin and creates a microretentive surface for an ideal interface for dentin bonding. To restore the tooth, a light-curable flowable composite (Tetric® PowerFlow, Ivoclar Vivadent) and sculptable composite (Tetric® PowerFill, Ivoclar Vivadent) were selected.
After disinfecting the preparation with 2% chlorhexidine gluconate, a 37% phosphoric acid etching gel (Total Etch, Ivoclar Vivadent) was applied to the enamel for 15 seconds in a selective etching technique. Etching the enamel facilitates maximum bond strength when compared with etching dentin, and it better protects against and reduces the chances of hypersensitivity. After thoroughly rinsing off the phosphoric acid etching gel, the preparation was dried (A-dec Warm Air Tooth Dryer, Patterson Dental), and a universal adhesive (Adhese® Universal, Ivoclar Vivadent) was placed and scrubbed using an ergonomic pen-like applicator (Adhese Universal VivaPen®, Ivoclar Vivadent) (Figure 2). The dentin was gently air-dried, but one of the reasons for selecting this universal adhesive was that it is flexible in its dentin moisture tolerance. With the adhesive placed, the tooth was then light cured for 3 seconds (Figure 3) using a high-intensity LED curing light (BluePhase® 3s PowerCure™, Ivoclar Vivadent), which provides 3,000 mW/cm2 of light-curing power in its 3-second cure mode. It decreases curing times, minimizing the risk of error during curing. To further increase the predictability of the curing process, its Polyvision™ technology automatically detects any movement away from the occlusal surface during curing to alert the user to the possibility of an inadequate cure and automatically extends the curing time.
To restore the tooth, the flowable composite (Tetric® PowerFlow [shade IVA], Ivoclar Vivadent) was placed first to serve as a dentin replacement layer. This shade is one of only three shade choices in the system, which reduces the number of shades that are necessary to inventory, and because it matches the shade of most adult posterior teeth, the time required for ideal shade matching is reduced as well. The material exhibits a similar opacity to dentin, possesses a high radiopacity to be easily distinguishable on radiographs, and utilizes highly reactive light-initiator technology (Ivocerin®, Ivoclar Vivadent) to realize its 4-mm depth of cure. When first placed, the material is highly translucent, but after curing, it becomes more opaque (Figure 4 and Figure 5). This makes it an excellent dentin replacement material and opaquer for discolored floors of preparations. When placed at the correct thickness, the opacity prevents the finalized restorations from appearing gray.
After the flowable layer was placed and cured to idealize depth and opacity, a layer of the sculptable composite (Tetric® PowerFill [shade IVA], Ivoclar Vivadent) was placed in one 4-mm increment, sculpted using contouring instruments (OptraSculpt® NG, Ivoclar Vivadent), and then light cured for the manufacturer recommended 3 seconds (Figure 6).
After any necessary occlusal adjustments were made and the restoration was finished and polished with polishing cups and points (OptraPol®, Ivoclar Vivadent), a final clinical photograph (Figure 7) and radiograph (Figure 8) were taken, which demonstrate the restoration's monolithic, void-free qualities, sealed margins, and esthetic chameleon effect.
About the Author
Jason Olitsky, DMD
Accredited Member
American Academy of Cosmetic Dentistry
Private Practice
Ponte Vedra Beach, Florida
References
1. Bohaty BS, Ye Q, Misra A, et al. Posterior composite restoration update: focus on factors influencing form and function. Clin Cosmet Investig Dent. 2013;5:33-42.
2. Jadhav S, Hegde V, Aher G, Fajandar N. Influence of light curing units on failure of direct composite restorations. J Conserv Dent. 2011;14(3):225-227.
3. Rodrigues Junior SA, Pin LF, Machado G, et al. Influence of different restorative techniques on marginal seal of class II composite restorations. J Appl Oral Sci. 2010;18(1):37-43.
4. Giachetti L, Scaminaci Russo D, Bambi C, Grandini R. A review of polymerization shrinkage stress: current techniques for posterior direct resin restorations. J Contemp Dent Pract. 2006;7(4):79-88.
5. Souza-Junior EJ, de Souza-Régis MR, Alonso RC, et al. Effect of the curing method and composite volume on marginal and internal adaptation of composite restoratives. Oper Dent. 2011;36(2):231-238.
6. Van Ende A, De Munck J, Van Landuyt KL, et al. Bulk-filling of high C-factor posterior cavities: effect on adhesion to cavity-bottom dentin. Dent Mater. 2013;29(3):269-277.
7. Margeas RC. Bulk-fill materials: simplify restorations, reduce chairtime. Compend Contin Educ Dent. 2015;36(1):e1-e4.
For more information, contact:
Ivoclar Vivadent
ivoclarvivadent.us
800-533-6825