Zirconia Crowns for Primary Molars
Two preparation alternatives
Theodore P. Croll, DDS | Kevin J. Donly, DDS, MS
During the past decade, the use of prefabricated zirconia crowns for restoration of carious, fractured, and malformed primary molars has become popular among dentists who treat children. These crowns are also quite popular with parents who are not enthusiastic about their children showing off the metallic appearance of stainless steel crowns. Even though stainless steel crowns on primary molars are not located in the anterior "esthetic zone" of a smile, they are still prominent enough to be seen when a child's mouth is open, especially mandibular primary first molars.
The purpose of full coronal restoration of a primary molar is to reestablish coronal form and function of the original anatomic crown that has been lost to caries, caries debridement, and tooth preparation. Going back more than 50 years, this challenge has been met by pediatric dentists using various sizes of preformed stainless steel crowns, which, after appropriate pulp protection, are custom-adapted and luted to properly prepared teeth by contouring, crimping, finishing, and polishing.1-7
Unlike stainless steel crown forms, the axial surfaces and marginal regions of prefabricated zirconia crowns cannot be manipulated to adapt them to a tooth preparation. The length can be reduced on prefabricated zirconia crowns, but their design inherently mandates that the tooth preparation be adapted to the crown, not the crown to the appropriately prepared tooth. Regardless of the challenges that dentists face adapting zirconia crowns to carefully prepared primary molars, the technique has proven to be successful.8
This article presents two cases involving restoration of mandibular primary first molars, each using a different preparation design. The first design closely follows the crown manufacturer's suggestions, and the second features a shoulder preparation with vertical retentive grooves to better engage the luting cement.
Case Report No. 1
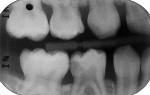
A boy aged 4 years and 11 months presented to the office with a large, deeply penetrating caries lesion on his mandibular right primary first molar (Figure 1). A bitewing radiograph suggested pulp exposure, but there were no clinical or radiographic signs or symptoms of pulp degeneration (Figure 2). The bitewing radiograph was also later used as a guide for crown size selection.
After local anesthetic injections were administered, a rubber dam was placed. Expect-ing that a pulpotomy would be indicated, the carious dentin was debrided while bur cutting a traditional Class II preparation, but care was taken not to penetrate into the pulp space (Figure 3). Next, a light-polymerized, resin-modified calcium silicate liner (TheraCal LC®, BISCO, Inc.) was injected and spread into the preparation and exposed to a curing light beam for 10 seconds (Figure 4).9,10 An incipient caries lesion and decalcified enamel on the mesial surface of the adjacent second molar were trimmed, and fluoride varnish was applied. After a matrix strip was placed and secured with a wooden wedge (Figure 4), a bioactive composite (ACTIVA™ BioACTIVE-RESTOR-ATIVE™, Pulpdent) was blended and injected into the preparation, overfilling the margins, and light hardened (Figure 5).11 Alternatively, a resin-modified glass-ionomer cement would have been acceptable for this step. The purpose of this "internal restoration" was to facilitate a full coronal preparation design and guarantee that the dentin was completely sealed during seating of the final prefabricated zirconia crown (NuSmile® ZR zirconia crown system, NuSmile). The molar was then prepared by reducing the occlusal aspect and axial surfaces by about 1.5 mm to 2 mm, miniaturizing the crown form so that the selected zirconia crown would acceptably replace the tooth structure that was lost to the caries infection and tooth preparation (Figure 6). The preparation margins were cut to a featheredge so that the unadaptable zirconia crown margins would overlap the termination of the axial preparation, peripherally.
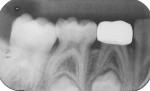
A pink ceramic "try-in" crown from the manufacturer was placed over the prepared tooth for trial sizing and to assess the need for refinement of the preparation. In this case, the buccal surface required slightly more reduction for the crown to be fully seated (Figure 7). Following the additional preparation, luting cement (BioCem Universal BioActive Cement®, NuSmile) was blended and placed within the selected tooth-colored crown form, and it was then pressed into place with finger pressure. A curing light was applied to the occlusal aspect for 10 seconds and then to the buccal and lingual aspects for 10 seconds each (Figure 8). This cement undergoes chemical polymerization in addition to light polymerization; therefore, complete hardening is assured. After light curing, the excess marginal cement was removed with a Hollenback carver (Figure 9). In addition, careful explorer probing and knotted dental tape are useful to remove interproximal increments of cement. At 46 months after placement, the zirconia crown demonstrated excellent occlusion and esthetics (Figure 10 and Figure 11). The 46-month postoperative radiograph revealed a distal margin that was slightly overhanging, but it proved to be of no consequence to the patient (Figure 12).
Case Report No. 2
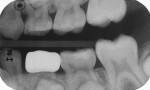
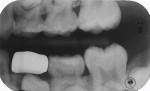
A 7-year-old girl presented with a fractured disto-occlusal, resin-modified glass-ionomer restoration on her primary mandibular left first molar that had been placed 30 months prior. The damage had permitted new caries to infect the distal third of the tooth (Figure 13). After local anesthesia was achieved and a rubber dam was placed, the carious tooth structure was debrided with a large round bur at slow speed, and the exposed dentin was covered with the resin-modified calcium silicate liner (Figure 14). Occlusal reduction was achieved in the same manner as in the previous case (Figure 15), and the axial reduction was cut to a shoulder preparation with the idea that the zirconia crown edge would seat onto the prepared margin (Figure 16). Two vertical grooves were included on the buccal aspect of the preparation to add to the surface area to improve luting cement adhesion. After the pink try-in crown established the proper size, the selected zirconia crown was filled with the luting cement and seated with finger pressure (Figure 17). The zirconia crown was observed 26 months after cementation (Figure 18 and Figure 19). At 33 months, the presence of advanced distal root resorption and eruption of the underlying premolar necessitated extraction of the crowned tooth (Figure 20 and Figure 21).
Discussion
Selecting a suitably sized prefabricated zirconia crown for a mandibular primary molar after tooth preparation can be a challenge. Generally, from the occlusal view, primary maxillary first molars are more rounded, and mandibular ones are more rhomboidal. In some children, the mandibular molars are more rounded in such a way that the manufactured crown forms can be difficult to adapt to the prepared tooth. One potential solution to this problem is to use a contralateral opposite-arch maxillary crown form to achieve an acceptable fit.12 Although the two preparation methods presented in this article have not been compared in a clinical study, both have demonstrated success in practice.
About the Author
Theodore P. Croll, DDS
Cavity Busters
Doylestown, Pennsylvania
Adjunct Professor
Pediatric Dentistry
University of Texas Health Science Center
San Antonio, Texas
Clinical Professor
Pediatric Dentistry
Case Western Reserve School of Dental Medicine
Cleveland, Ohio
Kevin J. Donly, DDS, MS
Diplomate
American Board of Pediatric Dentistry
Professor and Chair
Department of Developmental Dentistry
The University of Texas Health Science Center at San Antonio
School of Dental Medicine
San Antonio, Texas
References
1. Castaldi CR. Operative dentistry. In: Goldman HM, Forrest SP, Byrd DL, McDonald, RE, eds. Current Therapy in Dentistry, vol 2. St. Louis, MO: C.V. Mosby Company; 1966:621-655.
2. Mink JR, Bennett IC. The stainless steel crown. ASDC J Dent Child. 1968;35(3):186-196.
3. Full CA, Walker JD, Pinkham JR. Stainless steel crowns for deciduous molars. J Am Dent Assoc. 1974;89(2):360-364.
4. Myers DR. The restoration of primary molars with stainless steel crown. ASDC J Dent Child. 1976;43(6):406-409.
5. Croll TP, Riesenberger RE. Primary molar stainless steel crown restoration. Quintessence Int. 1986;17(4):
221-226.
6. Croll TP. Preformed posterior stainless steel crowns: an update. Compend Contin Educ Dent. 1999;20(2):89-92, 94-96, 98-100 passim; quiz 106.
7. Seale NS. The use of stainless steel crowns. Pediatr Dent. 2002;24(5):501-505.
8. Donly KJ, Sasa I, Contreras CI, et al. Prospective randomized clinical trial of primary molar crowns: 24-month results. Pediatr Dent. 2018;40(4):253-258.
9. Gandolfi MG, Siboni F, Taddei P, et al. Apatite-forming ability of TheraCal pulp- capping material. J Dent Res. 2011;90(Spec Iss A):abstract number 2,520.
10. Gandolfi MG, Siboni F, Prati C. Chemical-physical properties of TheraCal, a novel light-curable MTA-like material for pulp capping. Int Endod J. 2012;45(6):571-579.
11. Croll TP, Lawson NC. ACTIVA™ BioACTIVE-RESTORATIVE™ material in children and teens. Inside Dentistry. 2018;14(2)(suppl):1-8.
12. Croll TP, Donly KJ. Contralateral/opposite-arch zirconia crown restoration of two mandibular primary first molars. Inside Dentistry. 2015;11(3):78-81.