Immediate Replacement of a Fractured Implant and Adjacent Tooth
Success for secondary implant placement requires proper diagnostics and technique
Immediate implant placement—the extraction of a tooth/root and placement of an endosseous implant in the same surgical session—is a time-tested modality. The removal of a previously osseointegrated implant and immediate re-implantation is not well documented, however.
Several generations of root-formed implants have come and gone, though the utility of earlier implant versions persists for many years. When these implants fail due to fracture, removal is often required. If replacement of these implants with newer, improved versions of implants is desired, the surgeon must make a critical decision: can the implant be placed at the time of implant removal or should a staged approach be selected?
The virtues of one procedure include shorter number of surgical procedures, decreased morbidity, and faster overall treatment time. This can only be performed with the aid of 3-dimensional radiography (computed tomography or cone-beam computed tomography [CBCT] scan) to confirm that a prosthetically favorable fixture placement can be done and primary stability is anticipated at the time of fractured implant removal.
Other factors that must be considered include the absence or presence of active infection, the health of the soft tissues at the surgical site, and the medical stability of the patient. In addition, the removal of the fractured implant must be as minimally traumatic as possible, preserving the maximum amount of neighboring bone and avoiding mechanical and thermal trauma, which may compromise the wound healing and osseointegration potential for secondary implant placement.
Bone augmentation to reconstruct and preserve 3-dimensional ridge dimensions, critical for long-term success, is common. This can be managed similarly to those steps necessary for immediate implant placement after tooth extraction. If these criteria are satisfied, immediate re-implantation can be considered.
The following case report demonstrates how a fractured implant and adjacent fractured tooth were removed and replaced with two root-formed implants in one surgical procedure.
Case Presentation
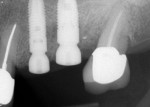
A 74-year-old female patient presented to the periodontal office complaining of pain in her maxillary left posterior sextant. Tooth No. 13 was hypersensitive to percussion and demonstrated a grade 2 mobility. The crown on the implant in the No. 14 position was mobile and associated with 8-mm probing depths with bleeding on probing and suppuration (Figure 1).
It was determined that tooth No. 13 was fractured and required removal. The implant in the No. 14 location was fractured in its coronal aspect, resulting in rotation of the abutment and crown. The treatment plan, which was to be performed in one procedure, was to extract tooth No. 13 and remove the non-salvageable implant No. 14, followed by two dental implants to restore function. However, the patient was informed that the invasiveness involved in removing the implant could require a staged approach instead.
Treatment
Following administration of local anesthesia (Septocaine® with epinephrine 1:100,000, Septodont, www.septodontusa.com), access through the occlusal surface of the implant-retained crown was achieved to remove the cemented crown and abutment together (Figure 2).
Sulcular incisions, including a mesiobuccal vertical-releasing incision, were performed from teeth Nos. 12 to 15. A full-thickness flap was elevated and the hopeless implant was visualized (Figure 3).
A 6.0-mm-diameter trephine was utilized under copious irrigation to remove the fractured implant, and tooth No. 13 was carefully extracted. Following debridement with ultrasonic and manual instrumentation, both sites were conditioned with a doxycyline slurry for approximately 3 minutes. After thorough irrigation with sterile saline, standard placement of a 4.0-mm x 13.0-mm implant (Astra Tech Implant System™, DENTSPLY Implants, www.dentsplyimplants.com) was performed in the No. 13 location. A combination of drills and an osteotome procedure (bone-added osteotome sinus floor elevation, or BAOSFE) was used to place a 5.0-mm x 11.0-mm implant in the site of tooth No 14, where the fractured implant was removed (Figure 4). The crestal sinus lift was obturated with freeze-dried cortical bone allograft (FDBA, LifeNet Health®, www.accesslifenethealth.org) along with the horizontal voids between the walls of the extraction socket of No. 13 and the osteotomy of No. 14. This was done to compensate for the predictable ridge resorption that occurs following extraction.1 The majority of these negative changes occur during the first year after extraction.2 Cardaropoli and colleagues3 showed that combining a particulate bone graft and collagen membrane can limit these changes around immediate implants.
A dermal allograft (PerioDerm® Acellular Dermis, DENTSPLY Implants) was trimmed via a soft-tissue punch and adapted around the two healing abutments and over the buccal and palatal cortical plates (Figure 5). Recently, Parma-Benfenati and colleagues4 demonstrated the use of a dermal allograft as a barrier over a space-maintaining device around dental implants. Linkevicius and colleagues5 showed that thickening peri-implant soft tissues with a dermal allograft preserves crestal bone more favorably compared to implants with naturally occurring thin mucosa; their study was based on the hypothesis that thicker soft tissue facilitates formation of biologic width without sacrificing crestal bone to compensate for the vertical dimensions of the soft-tissue peri-implant attachment.
The flaps were adapted around the healing abutments and sutured with a monofilament suture (CV5, Gore-Tex®, www.goremedical.com). The mesiobuccal vertical incision was closed with a 5-0 resorbable suture (Vicryl Rapide™, Ethicon, www.ethicon.com). A postoperative radiograph demonstrates the situation immediately after surgery (Figure 6). A transmucosal healing approach was selected because both implants achieved a high level of initial stability. Cordaro and colleagues6 demonstrated that when this mode of healing is performed, no difference exists regarding bone loss and probing depths compared to implants placed in a submerged fashion when bone grafting is performed simultaneous to implant placement. At 6 weeks, the site appeared clinically and radiographically to be healing without complications (Figure 7).
Definitive restorative treatment consisting of two separate screw-retained crowns was initiated approximately 10 weeks following surgery. More than 18 months after delivery of the restorations, soft tissues appeared free of inflammation and function was completely restored (Figure 8).
Discussion
The patient described in this case report was rehabilitated in one surgical appointment. The fractured implant and adjacent tooth both required removal. The treatment plan for implant replacement of both dental units often involves multiple procedures. While the prospect of immediate implant placement is a well-established treatment modality, the immediate replacement of a root-form implant is, fortunately, a less common occurrence. When implants fracture, inflammation and bone loss are frequently present, which often precludes the possibility of an immediate re-implantation. The coronal, supra-crestal location of the fracture in this situation, as well as the expedient treatment after the fracture, prevented an acute inflammatory reaction in the hard and soft tissues.
The preoperative CBCT scan revealed the presence of healthy bone palatal and apical to the hopeless fixture. It was anticipated that with careful implant removal, an immediate replacement could be attempted. Additional augmentation was done to prevent anticipated ridge-remodeling post implant removal and extraction.8,9 Botticelli and colleagues10 demonstrated the significant negative changes that occur following immediate implant placement.
In this case, an osteotome procedure was performed to elevate the maxillary sinus, with bone augmentation to facilitate implant placement with primary stability. Immediate placement of tooth No. 13 was done simultaneous with replacement of No. 14 implant, and one surgical site was managed with the identical regenerative therapy.
If implant positioning had been compromised based on post-implant removal and extraction-site anatomy, a staged approach would have been proposed prior to surgery. Because prosthetically favorable implant placement was anticipated and performed, immediate placement was done in this case. Because of the nature of the implant removal surgery and need to adapt the dermal barrier beyond the borders of the defect margins, a mucoperiosteal flap was elevated to achieve augmentation and soft-tissue adaptation. The question of ridge-dimension preservation with a “closed” technique has been questioned in the literature.11 Whether this would have affected the esthetic outcome in a posterior site was not as critical as achieving visual access for the efficacy of the procedure.
Conclusion
It was determined that with proper diagnostic information, such as CBCT, radiographs, occlusal analysis, and technique, implant removal and immediate replacement could and was successfully performed in this case.
About the authors
Barry P. Levin, DMD
Diplomate, American Board of Periodontology
Clinical Associate Professor
Department of Periodontology, University of Pennsylvania
Philadelphia, Pennsylvania
Private Practice Limited to Periodontology and Dental Implant Surgery
Elkins Park, Pennsylvania
Michael Weiss, DDS
Board of Directors
Delaware Valley Academy of Osseointegration
Ethics and Affiliate Committees
American Academy of Cosmetic Dentistry
Private Practice in General and Cosmetic Dentistry
Jenkintown, Pennsylvania
References
1. Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: a prospective clinical study. Int J Oral Maxillofac Implants. 2003;18(2):189-199.
2. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-323.
3. Cardaropoli D, Gaveglio L, Gherlone E, Cardaropoli G. Soft tissue contour changes at immediate implant: a randomized controlled clinical study. Int J Periodontics Restorative Dent. 2014;34(5):631-637.
4. Parma-Benfenati S, Roncati M, Galletti P, Tinti C. Resorbable dome device and guided bone regeneration: an alternative bony defect treatment around implants. A case series. Int J Periodontics Restorative Dent. 2014;34(6):749-755.
5. Linkevicius T, Puisys A, Linkeviciene L, et al. Crestal bone stability around implants with horizontally matching connection after soft tissue thickening: A prospective clinical trial. [published online ahead of print September 17 2013]. Clin Implant Dent Relat Res. 2013. doi: 10.1111/cid.12155. Accessed January 28, 2015.
6. Cordaro L, Torsello F, Chen S, et al. Implant-supported single tooth restoration in the aesthetic zone: transmucosal and submerged healing provide similar outcome when simultaneous bone augmentation is needed. Clin Oral Implants Res. 2013;24(10):1130-1136.
7. Chen ST, Beagle J, Jensen SS, et al. Consensus statements and recommended clinical procedures regarding surgical techniques. Int J Oral Maxillofac Implants. 2009;24(suppl):S272-S278.
8. Roe P, Kan JY, Rungcharassaeng K, et al. Horizontal and vertical dimensional changes of peri-implant facial bone following immediate placement and provisionalization of maxillary anterior single implants: a 1-year cone beam computed tomography study. Int J Oral Maxillofac Implants. 2012;27(2):393-400.
9. Kan JY, Rungcharassaeng K, Lozada JL, Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2- to 8-year follow-up. Int J Oral Maxillofac Implants. 2011;26(1):179-187.
10. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31(10):820-828.
11. Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: An experimental study in the dog. Clin Oral Implants Res. 2009;20(6):545-549.