Self-Adhesive Resin Cements for Luting Zirconia- and Metal-Based Crowns
More predictable results with fewer materials and steps
In recent years, material selection for crown and bridge has increasingly moved from metal-based to zirconia-based restorations. Zirconia made it possible to create posterior restorations that were stronger and more durable than previously available all-ceramic restorations. Additionally, unlike leucite-based ceramics, lithium disilicate ceramics, and alumina-based ceramics, which require that the restoration be bonded to the tooth, zirconia restorations can be bonded or cemented.
Because metal-based restorations are still being used, a luting material that can be used with both metal-based and ceramic restorations minimizes the number of cements required in the practice. Self-adhesive resin cements fulfill this need, providing strong bonds to dentin and a variety of materials used for crowns.1
Additionally, when restoring endodontically-treated teeth that will require placement of a post, use of self-adhesive resin cement simplifies the process of post cementation. With the technique commonly used with dentin adhesives and resin cements in the past, there was a risk of adhesive pooling in the apical of the post space, preventing complete seating of the post as well as complete curing. With the introduction of self-adhesive resin cements, the use of an adhesive in the post space is eliminated, as are potential issues associated with its use in this treatment.
Case Presentation
A 35-year-old male patient presented for an initial examination and prophylaxis. The patient indicated that the crown placed on tooth No. 31 approximately 2 years prior had needed repeated re-cementation. He also reported pain in the upper right posterior quadrant. Radiographs were taken, and decay was noted on the mesial of tooth No. 2 and deep decay on the distal of tooth No. 3, which also demonstrated an apical lesion on the palatal and distal buccal roots. This tooth tested with elevated response to cold, percussion, and electric pulp testing. Tooth No. 31 had previous endodontic treatment and had a bonded core present. Examination noted short preparation walls with the margin coronal to the gingival margin and a tapered preparation, leading to poor retention and frequent crown debonding, which explains the need for reluting.
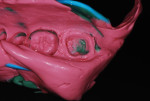
Treatment recommendations included placement of a composite restoration on the mesial of tooth No. 2, endodontic treatment on tooth No. 3 (Figure 1) followed by placement of a post/core, and restoration with a full-coverage crown and re-preparation of tooth No. 31 for a new crown (Figure 2).
Clinical Phase 1
Anesthesia was infiltrated, a rubber dam was placed, and access was achieved to uncover the pulp chamber. The canal orifices were identified and explored to estimated working length with a #20 hand file. An apex locator was used to set and confirm the working length. The canals were instrumented to working length using EndoSequence rotary nickel-titanium files (Brasseler USA, https://brasselerusa.com) with a final size of 35 and 0.04 taper in all three canals. Canals were alternately irrigated with 5% sodium hypocholorite and 17% EDTA liquid as rotary files were switched.
Canals were dried with paper points, and a Resilon cone matching the file size was trial fitted in each canal to working length. RealSeal SE (Sybron Dental Specialties Inc., www.sybronendo.com) was dispensed from the automix syringe onto a pad, and the cones were coated in sealer and introduced into each canal to working length. Excess Resilon cone was cut off using a Thermique™ Thermal Condenser (Parkell, Inc., www.parkell.com), and a radiograph was taken to verify apical obturation.
A post drill was used in a slow-speed handpiece to create post space in all three canals to a depth of 12 mm from the coronal surface, ensuring that the apical extent of the post would be a minimum of 3 mm apical to the osseous crest and would retain at least 5 mm of apical obturation material to make sure the canals remained sealed over time. Tapered posts (GC Fiber Post, GC America Inc, www.gcamerica.com) with a diameter of 1.4 mm were trial fitted to ensure they would seat to the depth of the prepared post holes. GC Ceramic Primer (GC America) was applied to the posts, allowed to sit for 2 minutes, and then air-dried. Gradia® Core self-etching bond (GC America) was mixed and applied to the posts; after 30 seconds, this was air-dried then light-cured for 10 seconds to provide a highly bondable surface between the fiber post and luting resin and core material. Bonding adhesive was not placed into the post preparations.
G-CEM LinkAce™ (GC America), a self-adhesive resin luting cement with high bond strength to dentin, metal, and ceramics, was injected into the post preparations, and the posts were inserted to depth and light-cured to set the coronal aspect, stabilizing the posts. The portion of the luting cement that the light was unable to reach would self-cure after 4 minutes. Additional Gradia Core self-etching bond was brushed onto the exposed dentin of the coronal and left for 30 seconds. A light stream of air was applied to evaporate the remaining solvent in the adhesive for 10 seconds and then light-cured for 10 seconds. Gradia Core was dispensed to backfill the tooth to create a core around the coronal aspects of the fiber posts. The core was light cured and then allowed to complete self-cure mode for 3 minutes. The rubber dam was removed, the coronal aspect was adjusted for occlusion, and the patient was dismissed.
At the next appointment, local anesthetic was administered and a preliminary impression of both arches was taken using EXA’lence™ heavy body VPES (vinyl polyether silicone) impression material (GC America) in a full-arch tray. Chemically, VPES impression materials are a blend of a polyether and a vinyl polysiloxane (VPS) material. This provides the hydrophilic (wetting) properties of a polyether along with the higher tear strength of VPS that allows it to perform well in thin segments such as in the sulcus.2-4 Better hydrophilicity means more precise flow subgingivally with fewer voids and bubbles. Additionally, the better tear strength subgingivally provides more accurate replication of the subgingival anatomy, including the preparation margin.4
Crown preparation was performed on tooth No. 3, placing the margins at approximately 0.5 mm apical to the gingival margin (Figure 3). Access to the mesial of tooth No. 2 allowed for caries removal while preserving the mesial marginal ridge of the tooth. G-ænial™ Bond (GC America) was applied to the cavity prep and allowed to sit for 10 seconds. It was air-thinned for 5 seconds and then light-cured for 10 seconds. As the area to be restored was in a very low wear area, it was decided to use a flowable resin. G-ænial™ Universal flo Flowable composite (GC America) was dispensed into the preparation, and a brush tip was used to smooth the uncured composite, which was then light cured for 20 seconds. Tooth No. 31 was re-prepared, lowering the margins approximately 1 mm subgingivally and paralleling the axial/proximal walls to increase retention for the new crown (Figure 4).
One at a time, the previously taken preliminary impressions of the maxillary (Figure 5) and mandibular (Figure 6) arches were each filled with EXA’lence extra light body VPES impression material and reinserted intraorally. After 4 minutes, the trays were removed. The two-stage impression technique allows the preliminary impression material to gently force the lighter body wash material into the sulcus, capturing the margins without the need for a retraction cord. This works exceptionally well when a full-arch tray is used, as the tray resists any deformation of the previously set impression material. Use of this technique with dual-arch trays can lead to deformation of the impression due to the lower resistance of the tray,5 and the author does not recommend it. Exabite™ II NDS VPS bite registration creme (GC America) was injected onto the occlusal surfaces of the lower arch, and the patient was asked to occlude with light pressure. Upon setting, the occlusal record and the impressions of each arch were sent to the lab.
The materials selected for the crowns included a zirconia-based all-ceramic crown on the maxillary molar and a porcelain-fused-to-metal (PFM) restoration for the mandibular molar. As the patient reported a history of clenching, it was decided that the second molar would be better served by the PFM, as esthetics was less critical than with the first molar and the material at the distal needed higher strength in a thinner thickness. Thicker material was needed on the distal marginal ridge of No. 31, with a monolithic zirconia crown versus a PFM to limit the potential for chipping in this area.
Provisional restorations were prepared using Revotek LC™ (GC America) and seated. Using the Chairside Shade Guide System (LSK121, https://lsk121.com), the shades of the natural, unrestored teeth were compared with various shade tabs in the guide, and it was decided with the patient’s input that tab MY13 matched the best. A lab prescription requesting a zirconia-based crown with overlaying ceramic for the maxillary molar and PFM for the mandibular molar was filled out, and the case was shipped to LSK121 Lab.
Laboratory Phase
The impressions were poured in stone, creating dies for fabrication of the crowns. Because the two crowns to be fabricated would be of different materials, the process would vary based on the coping that was to be employed for each crown. To ensure matching esthetics with the two different copings, it was decided to use GC Initial™ porcelain (GC America) because of its deep chroma, high fluorescence, opalescence and/or high transparency. All the shades across the entire system have been carefully harmonized, whatever the type of coping created or the process used for fabrication.
Clinical Phase 2
The Revotek LC provisional restorations were removed and the preparation was cleaned. The two crowns were tried in and marginal fit was assessed. Occlusion was checked and a minor high spot was adjusted in the mesial buccal cusp tip of tooth No. 31. A CeraGlaze cup (Axis | Sybron Endo, www.axisdental.com) restored the glaze lost at the place of adjustment. GC Metalprimer II (GC America) was applied to the interior of the PFM crown to improve bonding of the resin cement to be used. It was then allowed to sit for 2 minutes and air-dried. Both crowns were loaded with G-CEM LinkAce and inserted intraorally. The patient verified that the crowns were fully seated and the occlusion felt comfortable. Then a cotton roll was inserted, and the patient was asked to occlude for 4 minutes while the self-adhesive resin cement completed its self-cure mode.
Upon setting, any excess cement at the crowns’ margins was removed with a hand instrument (Figure 7 and Figure 8). Occlusion was verified and the patient was dismissed.
Conclusion
Self-adhesive resin cements have simplified restorative dentistry, allowing more predictable, consistent results with fewer materials and steps. This relates to cementation of posts when restoring endodontically-treated teeth as well as luting crowns of various materials. High bond strengths are important when luting full-coverage crowns and partial coverage onlays; occlusal loading has the potential to dislodge the restoration from the tooth preparation. This becomes more important when the preparation is short and cannot rely solely on mechanical retention.
Posts luted within a canal placed when restoring endodontically-treated teeth do not require high bond strengths; the post has a narrow diameter with a long length, making dislodgement difficult (as long as restorative ferrule is achieved with the crown). Failure observed with fiber posts can relate to which cement was used. Resin-cemented fiber posts have greater pullout strength than glass ionomer cements, which relates to the cement’s adherence to the fiber post.6 The literature has demonstrated better bond strength for resin luting materials versus glass ionomers and resin-modified glass ionomers with fewer failures.7 This can be clinically relevant when crowns are to be placed on preparations that minimize the axial wall height (short prep) regardless of the material used to fabricate the crown.
Disclosure
Dr. Kurtzman received an honorarium from GC America for preparation of this article.
Acknowledgement
Laboratory work performed by LSK121 Oral Prosthetics, Naperville, Illinois.
References
1. Sterzenbach G, Karajouli G, Naumann M, et al. Fiber post placement with core build-up materials or resin cements-an evaluation of different adhesive approaches. Acta Odontol Scand. 2012;70(5):368-376.
2. Fukushima S, Tsunooka M, Kamohara H, Sakuma T. Dimensional stability of new elastomeric impression material [abstract]. IADR. 2009. Abstract 3291.
3. The Ratings [membership required]. Reality Publishing Company website. www.realityesthetics.com.
4. Nathanson D, Takahama Y, Lherault R, Attar M. Tear strength of new elastomeric impression materials [abstract]. https://iadr.confex.com/iadr/ced09/webprogram/Paper123666.html. Accessed October 20, 2014.
5. Carrotte PV, Johnson A, Winstanley RB. The influence of the impression tray on the accuracy of impressions for crown and bridge work—an investigation and review. Br Dent J. 1998;185(11-12):580-585.
6. Pereira JR, da Rosa RA, do Valle AL, et al. The influence of different cements on the pull-out bond strength of fiber posts. J Prosthet Dent. 2014;112(1):59-63.
7. Turker SB, Ozcan M, Mandali G, et al. Bond strength and stability of 3 luting systems on a zirconia-dentin complex. Gen Dent. 2013;61(7):e10-e13.
Gregori M. Kurtzman, DDS, MAGD, DICOI
Private Practice
Silver Spring, Maryland
For more information, contact:
GC America
800-323-7063
www.gcamerica.com