Primary Incisor and Canine Restoration in a Child with Amelogenesis Imperfecta
Material advances bring new options to the treatment of enamel malformations
For decades, bonded resin “strip crowns,”1-3 open-faced resin-filled “window” stainless steel crowns,4,5 and resin-veneered stainless steel crowns6-8 have been the chief means of restoring severely carious, fractured, or malformed primary anterior teeth. All of these methods have been quite successful, but they are not without disadvantages. Resin strip crowns sometimes fracture and segments may detach, no matter what brand of resin-based composite is used. Likewise, some resin coatings of resin-veneered stainless steel crowns chip away over time. “Resin window” stainless steel crowns are very successful, but they usually show a silver-colored periphery, which is objectionable to some parents.
A number of manufacturers have introduced preformed zirconia primary crowns, which have unprecedented physical strengths and ideal appearance, in an array of sizes. This brief report documents treatment of a child with amelogenesis imperfecta whose carious and malformed maxillary primary central incisors were restored with resin-veneered stainless steel crowns. Two years later, after market introduction of zirconia primary anterior crowns, the lateral incisors and canine teeth were restored with the new ceramic crown forms.
Case Presentation
A 30-month-old girl was brought to the office by her mother in January 2010. The mother’s chief complaint was the color of the child’s teeth. The child was cooperative for examination on her mother’s lap. Intraoral examination revealed a full primary dentition with amelogenesis imperfecta (Figure 1 and Figure 2). There was generalized enamel hypoplasia, and the enamel that was present was thin at best. In some areas of both anterior and posterior teeth, no enamel was present over the dentin. Sharp-pointed cusp tips on the four primary canines were trimmed smooth with aluminum oxide disks and large round diamond burs at slow speed.
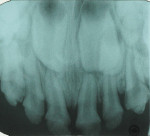
The child had large lingual caries lesions on the maxillary central incisors (Figure 3) and beginning caries lesions on the four maxillary primary molars. Small occlusal caries lesions were also diagnosed on the mandibular primary second molars. A maxillary occlusal radiograph showed no pulpal, radicular, or osseous alterations of the incisors (Figure 4). After the use of nitrous oxide/oxygen inhalation and local anesthetic was explained to the mother, the patient was scheduled for two appointments for resin-veneered stainless steel crown restoration of the maxillary central incisors, stainless steel crown restoration of the four maxillary primary molars, and occlusal resin-modified glass-ionomer repair of the mandibular primary second molars.9 The parents were supplied with a 5000-ppm sodium fluoride dentifrice and advised on its daily use; they were specifically instructed on wiping away excess to minimize swallowing of the material.
During the first visit, the child was anxious about treatment, but very cooperative. A 20% flow of nitrous oxide with 80% oxygen by mask inhalation was used. Earphones playing children’s music were placed for attention diversion. With routine local-infiltration anesthetic injections (articaine 4% with 1/200,000 parts epinephrine), the “nano-ionomer” (Ketac™ Nano Light-Curing Glass Ionomer Restorative, 3M ESPE, www.3mespe.com) was used to restore the carious occlusal surfaces of the mandibular primary second molars. The maxillary central incisors were then restored as follows.
Rubber dam was not used, but a 4x4 cotton gauze protected the throat and airway throughout treatment (removed only for photographs). Carious substance was first cut away using a medium-sized round bur at slow speed. In this case, marginal bleeding was not problematic. Sometimes such bleeding needs to be controlled by cotton swab dabbing with hydrogen peroxide or by placement of retraction cord in the usual manner. Papillary injections with local anesthetic solution containing a vasoconstrictor can also be helpful. A thin coating of resin-modified glass-ionomer base/liner (Vitrebond Plus, 3M ESPE) was placed and light-cured in the deep regions of dentin exposure on the lingual surfaces. The two incisors were then prepared for reception of the resin-veneered stainless steel crown forms. Preparation was designed to “miniaturize” the teeth with a feather-edge margin so the crown forms could replace what was lost to the malformation, removal of carious tooth structure, and tooth preparation (Figure 5).6,8 Tooth reduction usually removes the enamel layer and about one-third of the dentin thickness. The manufacturer of NuSmile crowns suggests 1.5 to 2 mm of incisal reduction, and the same amount of axial reduction (about 20% of crown height and thickness). Of course, additional dentin needs to be prepared for complete debridement of the carious dentin, and to allow for complete seating of the selected crown. NuSmile® resin-veneered crowns (NuSmile Pediatric Crowns, www.nusmilecrowns.com) were chosen for treatment. Crown size was selected by trial and error.
The lingual crown margins were trimmed slightly for proper length and then slightly crimped for better adaptation. To avoid detaching or fracturing the resin facing, the labial margins were not treated in any way. Resin-modified glass-ionomer cement (RelyX™, 3M ESPE) was blended and injected into the crown forms, with care taken to avoid air entrapment. The crowns were seated with digital pressure, and excess luting cement was cleared with a cotton swab (Figure 6).
At a second appointment, the four maxillary primary molars were restored with stainless steel crowns,10 also using nitrous oxide/oxygen inhalation, music with earphones, and articaine local anesthesia.
Two years later, the left primary lateral incisor had developed lingual caries. In the interim, commercial preformed anterior zirconia crown forms had become available. A zirconia crown (NuSmile® ZR, NuSmile Pediatric Crowns) was used to restore the left lateral incisor. That crown was also cemented with the resin-modified glass-ionomer luting cement (Figure 7).
For esthetic and prevention reasons, the parents were given the option of having the right lateral incisor and the maxillary primary canine teeth also restored with zirconia crowns for no additional fee. They gratefully accepted that offer. During a 30-minute visit, the right lateral incisor was restored as follows.
Nitrous oxide/oxygen inhalation at a 20% flow and music diversion with earphones was used again. Crown selection was facilitated by NuSmile’s pink try-in crowns (Figure 8). The advantage of the try-in crowns is that contaminants (blood, saliva, and phosphate groups from the phosphoric acid) coat the inner surface of the zirconia and are not easily removed by usual cleaning procedures. Such contaminants can interfere with the cement bond to the internal crown surface and affect cement retention. The try-in crowns facilitate crown size selection and can be autoclaved for additional use, and their pink color is easily identifiable. With articaine local anesthetic infiltration and a 4x4 inch gauze positioned palatally, the right lateral incisor was prepared in the same manner used for the central incisors, with the exception of increased axial preparation depth, to make room for the thicker porcelain crown form (Figure 9 and Figure 10). One aims for a passive fit, but not so loose as to result in large marginal “overhang.” Fit of the crown was assured using the try-in crown (Figure 11), and the actual crown form was luted into place using Ceramir® C&B Cement (Doxa Dental AB, www.ceramir.se) (Figure 12 through Figure 14).
At a subsequent appointment, the canine teeth were restored using the same management for patient comfort and safety. Crown size was determined with a canine try-in crown (Figure 15). Preparation included feather-edge subgingival margins, good incisal clearance in all mandibular excursions, and generous axial preparation to make room for the bulk of the preformed zirconia crown (Figure 16). Vertical grooves were cut to increase the surface area of luting cement contact for enhanced retention (Figure 17). The properly fitted crowns were luted into place using Ceramir C&B Cement (Figure 18) in the same manner as in the lateral incisor crown procedure.
The patient was photographed, and a maxillary occlusal radiograph recorded when the patient was 6 years old (Figure 19 through Figure 21).
Discussion
There are nearly 100 different hereditary causes of enamel malformations. Most enamel anomalies are associated with syndromes, whereas others affect the enamel with no systemic influences.11 This latter group is traditionally referred to as amelogenesis imperfecta. These conditions are characterized by either a deficiency in the amount of enamel (enamel hypoplasia) or by enamel that is hypomineralized.12 Hypomineralized enamel is typically discolored; it is either an opaque white or yellow-brown to orange color.13 The genetic causes of these enamel malformations are known for many, but not all, of the different types of amelogenesis imperfectas. Currently there are 10 genes known to cause enamel defects referred to as amelogenesis imperfecta.14 Understanding the type of amelogenesis imperfecta a patient has can help determine the types of treatments most likely to be successful. Patients with severely hypomineralized enamel often have extreme dental sensitivity and require full-coverage crowns. If the enamel is pitted or thin but well mineralized, treatment approaches using adhesively bonded materials, such as resin-based composite or resin-modified glass-ionomer cement, may be successful.
Ceramir C&B, originally called XeraCem, is a calcium aluminate-glass ionomer luting cement intended for permanent cementation of crowns and fixed partial dentures, gold inlays and onlays, prefabricated metal and cast dowel and cores, and high-strength all-zirconia or all-alumina crowns.15,16 The cement is a water-based composition comprising calcium aluminate and glass-ionomer components and has been demonstrated to be bioactive.15,17 Pre-clinical laboratory and biocompatibility testing and periodic recalls up to 3 years have shown that Ceramir C&B thus far has performed quite favorably as a luting agent for permanent cementation of permanent restorations.18,19 Although the resin-modified glass-ionomer luting cement RelyX Luting Plus has served dentists exceedingly well over many years and has become the standard for many cementation requirements in general, Ceramir C&B appears to be an excellent alternative for use as a bioactive luting agent for zirconia crowns on primary teeth.
When the central incisors were treated, zirconia crowns were just becoming available. However, treatment for this child typifies how anterior resin-bonded veneered stainless steel crowns as well as zirconia crowns can successfully restore carious or malformed primary anterior teeth. In addition, treatment of this child using nitrous oxide/oxygen inhalation and auditory diversion with earphones and music demonstrates how a preschooler can be treated safely and comfortably in a routine clinical dentistry setting without the need for parenteral sedative medications or general anesthesia.
Disclosure
Dr. Croll and Dr. Wright have no financial interest in any product or company named in this article. Kornberg School of Dentistry (Temple University, Philadelphia, Pennsylvania) has received prior funding from Doxa Dental AB for Dr. Jefferies’ research about Ceramir C&B, one of the luting cements mentioned in this article.
References
1. Doyle WA. A new preparation for primary incisor jackets. Pediatr Dent. 1979;1(1):38-40.
2. Webber DL, Epstein NB, Wong JW, Tsamtsouris A. A method of restoring primary anterior teeth with the aid of a celluloid crown form and composite resins. Pediatr Dent. 1979;1(4):244-246.
3. Croll TP. Restorative dentistry for preschool children. Dent Clin North Am. 1995;39(4):737-770.
4. Helpin ML. The open-face steel crown restoration in children. ASDC J Dent Child. 1983;50(1):34-38.
5. Croll TP. Primary canine full coronal restoration: new considerations. Quintessence Int. 1985;16(2):143-147.
6. Croll TP, Helpin ML. Preformed resin-veneered stainless steel crowns for restoration of primary incisors. Quintessence Int. 1996;27(5):309-313.
7. Waggoner WF, Cohen H. Failure strength of four veneered primary stainless steel crowns. Pediatr Dent. 1995;17(1):36-40.
8. Croll TP. Primary incisor restoration using resin-veneered stainless steel crowns. ASDC J Dent Child. 1998;65(2):89-95.
9. Killian CM, Croll TP. Nano-ionomer tooth repair in pediatric dentistry. Pediatr Dent. 2010;32(7):530-535.
10. Croll TP. Preformed posterior stainless steel crowns: an update. Compend Contin Educ Dent. 1999;20(2):89-106.
11. Pindborg JJ. Aetiology of developmental enamel defects not related to fluorosis. Int Dent J. 1982;32(2):123-134.
12. Suckling GW. Developmental defects of enamel—historical and present-day perspectives of their pathogenesis. Adv Dent Res. 1989;3(2):87-94.
13. Jälevik B, Norén JG. Enamel hypomineralization of permanent first molars: a morphological study and survey of possible aetiological factors. Int J Paediatr Dent. 2000;10(4):278-289.
14. Wright JT. Developmental defects of the teeth. University of North Carolina at Chapel Hill website. www.dentistry.unc.edu/research/defects/pages/ai.htm. Accessed May 29, 2014.
15. Doxa Dental AB. 510(k) Summary, XeraCemTM, K081405, August 21, 2008.
16. Doxa Dental AB. 510(k) Summary, Ceramir® Crown &Bridge, K100510, March 25, 2010.
17. Lööf J, Svahn F, Jarmar T, et al. A comparative study of the bioactivity of three materials for dental applications. Dent Mater. 2008;24(5):653-659.
18. Jefferies SR, Pameijer CH, Appleby DC, et al. A bioactive dental luting cement—its retentive properties and 3-year clinical findings. Compend Contin Educ Dent. 2013;34 (Spec No 1):2-9.
19. Jefferies S. Bioactive and biomimetic restorative materials: a comprehensive review. Part II. J Esthet Restor Dent. 2014;26(1):27-39.
About the Authors
Theodore P. Croll, DDS
Private Practice
Doylestown, Pennsylvania
Affiliate Professor
Department of Pediatric Dentistry UW School of Dentistry
Seattle, Washington
Adjunct Professor
Department of Pediatric Dentistry UT Health Science Center
San Antonio, Texas
Steven R. Jefferies, MS, DDS, PhD
Professor
Department of Restorative Dentistry
Director of Clinical Research and Biomaterials Research Laboratory
Temple University Kornberg School of Dentistry
Philadelphia, Pennsylvania
J. Timothy Wright, MS, DDS
Bawden Distinguished Professor and Director of Strategic Initiatives
Department of Pediatric Dentistry
School of Dentistry
University of North Carolina
Chapel Hill, North Carolina