A Perspective on Digital Radiography
Converting to digital technology holds many benefits for treatment planning, acceptance, and completion.
Digital technology has been a well-received advancement in dental imaging; however, it would be incorrect and unsafe to classify it as a declaration of a new "standard of care." According to a 2007 survey conducted by the American Dental Association, of the approximately 173,000 dentists in the United States, 36.5% used digital imaging for bitewing and periapical radiography, and 20.3% used it for panoramic studies.1 These statistics are up from 7 years ago, when only about 11.5% of practicing dentists had stopped using film; at that time a random survey among a sample of 1,709 general dentists in private practice were using digital technology for all of their intraoral imaging.2
Many of those who have aggressively jumped into the digital world have also embraced other digital technology. Second-year dental students could almost be expected to pick up the technology in a few outings, while many older dentists who graduated in the 1960s and 1970s are slower to adapt and change. Some of the drawbacks to embracing change are fear of that change, the cost of that change, and the learning curve for that change.
A parallel could be drawn with the same trepidation most people experienced when it came time to go from an old pegboard system to their first computer and software management system. Once the switch is made, no one tends to look back.
Initially, the cost factor can be significant. Optimally, each operatory should have its own dedicated computer. Dragging around a laptop becomes bothersome and unacceptable. Sensors can be centrally stored and those can be shared by different operators. The investment in higher-quality monitors will become cost effective by being able to offer a more effective case presentation. Each room with an x-ray will cost from $12,000 to $15,000 for a wired system, and $20,000 to $23,000 for a wireless system.
With all the new advances, the learning curve is actually no longer as steep as it once was; learning CAD/CAM, for example, has become much easier with the newest generation of user-friendly computer-assisted restoration systems. If auxiliaries are good at taking high-quality images with film, they will quickly learn how to position the digital sensors and be able to produce equally as good digital images. Most manufacturers include in-depth tutorials with the software to help show how to best place and effectuate a quality image. Well-trained associates of these manufacturers will come to the office and spend as much time as necessary to help doctors and their staff through the transition.
Types of Digital Radiography Approaches
Digital technology is possible with three different approaches. The first, direct scanning of an existing x-ray, will be only as good as the quality of the scanner and, of course, the original film. The second approach uses photo-stimulable phosphor plates (PSP) for indirect digital imaging. These plates are often as thin or thinner than a traditional film packet. It is questionable how long these images are usable. The time it would take from exposure to being loaded into the computer could be anywhere from 90 seconds to 4 minutes, depending upon the equipment. Very often there are scratches on the plates, which creates an unacceptable image.
The third and last approach employs digital sensors. All sensors are close to the size of traditional films: size 0 is 31 mm x 22 mm; size 1 is 37 mm x 24 mm; and size 2 is 48 mm x 30 mm. Thickness often dictates ease of use. Hopefully, new technology will make sensors more comfortable; however, the thinnest sensor is still more than 4 mm thick, (4.2 mm), and the others are slightly less than 5 mm thick. Some manufacturers have rounded the corners and others have provided "pillows" that make the unyielding plastic more comfortable. However, the reality is that these sensors do not bend as film does, which often creates distorted images at the corners. Many patients do not tolerate film packets, and most likely these same patients will have some difficulty with the sensors. While cone beam and external imaging is on the rise, it is still far too expensive for many dentists.
PSP plates have been around since 1981, and are the basis of nearly all hospital digital radiography systems. Although theoretically the plates can be used indefinitely, in practice the plates need to be replaced approximately every 3 months or after 50 exposures.3
Adopting Digital Technology
Mastering the software tools takes a little time; however, the end result is well worth it. If one wishes to translate critical diagnostic findings into comprehensive treatment plans, one could expect a higher percentage of case acceptance if digital radiography is used. The full-monitor projection allows the dentist to "show and tell" with greater ease and understanding. The dentist can establish a frame of reference, such as normal biologic width on one tooth and the changes that take place with periodontal disease on a second tooth that alter normal relationships. Just as everyone who uses intraoral photographic imaging knows how powerful that tool has become, a similar reaction takes place when patients can view an enlarged and enhanced image.
Similarly, electronic filing systems offer dentists an avenue to advance their practice with new technology. Dentists can now take, and share with other dentists, exquisite before-and-after reports that provide an excellent record of treatment. One of the benefits of having computerized files in the operatory is the easy access to the patient's treatment progress, without flipping through a cumbersome paper chart and looking at dates on old radiographs.
One of the easiest and best ways to get a taste of how a technology works is to have a manufacturer representative fully demonstrate a system in the office for all staff who would be using it, and then leave the system in the office for a week or two as a trial run. This will allow a dental practice to see how the system works on a daily basis, how easily the team can adapt to the new system, whether the new system makes a significant difference in production, and, ultimately, make a more informed purchasing decision. At the very least, the dentist and all hygienists and dental assistants who would be using the new system should give it serious attention during the trial period. Demonstration units are generally set up with a laptop and many can even be easily taken from operatory to operatory. Many dentists have found that after trying a new digital system they can basically lock the door to their darkroom and rid the office of all the caustic fixing and developing chemicals, and never look back.
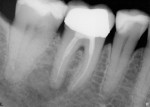
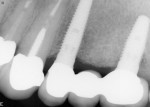
Just as many endodontists have embraced this technology, restorative dentists can predictably monitor their functional and esthetic outcomes of many procedures as well. For example, if doing crown preparations, before taking the impressions check the emergence profile and the intended path of insertion as it relates to good contacts (Figure 1, Figure 2 and Figure 3). Because radiation exposure is cumulative, using digital technology generates far less total exposure—up to 70% to 80% less—so the overall radiation risk is greatly diminished in return for the benefit of producing more predictable results.4 This will better predict the intended result before the laboratory or the in-office CAD/CAM system produces the restoration. When the restoration is tried in prior to cementation (Figure 4), the emergence profile can be observed, which will help predict how the biologic width of the periodontium will accept this new restoration. Decisions can be made to accurately determine the need for surgical elongation of certain teeth where subgingival involvement is an issue (Figure 5). Of course, this can also be done with traditional film radiography; however, few dentists want to spend the time necessary and, more importantly, subject the patient to excess radiation.
In 2004, Gordon Christensen, outlining the advantages of digital radiography relative to immediate observation of images, stated: "If this were the only positive aspect of digital radiography, I still would choose it over conventional radiography."4 However, instant imaging is far from the only benefit, as manufacturers and the research behind the technology report that 80% to 90% less radiation is necessary to produce a quality image, compared to using traditional E-type film.5
Improving Case Acceptance
Case presentation is the cornerstone of a current, technologically up-to-date practice. The most successful practitioners are those who can easily communicate with their patients. Presentation is preceded by a thorough examination, careful diagnosis, and the development of a comprehensive treatment plan that makes sound use of modern technology. Patients must take away from a consultation visit a clear picture of what their dentist has planned. In most instances, patients leave the office with a definitive treatment plan. This is not necessarily an electronic readout with codes and fees; however, a detailed letter of explanation could include images. In most cases this should include the fees and financial arrangements.
While the traditional 1.5-inch radiographs that many still use are instrumental for the dentist, they are not as useful for educating patients. The larger or full-screen images provided digitally can be highlighted with arrows pointing out areas of concern (Figure 6). This technology, along with clinical images, will serve for decision-making and legally documenting the issues that need attention.
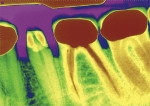
For chairside presentations, digital radiography has advanced and promoted more effective communication with the patient. Using a full-screen monitor, the presenting dentist can take full advantage of exquisite software with many options for color, positive images, revealing images, and complimenting the traditional negative image, which all afford the patient far more information that they can actually understand (Figure 7). The ability to point with a cursor, aligning the image beside a digital clinical image, often tells a more complete story.
Neff has covered visual technology for case presentation in depth.5 He closely correlates digital camera systems, computer imaging enhancements, with effective case presentations. Combining the clinical visual technology on the same screen with digital radiography presents the complete image. In the presentation of implant options, the operating dentist can show the patient where the fixture will be placed. This creates a template that ensures the dentist's ability to accurately place dental implants.
Communication
Since the advent of electronic communication, everyone has enjoyed the benefit of faster transfer of both general and sensitive information, which has profound practical and economic effects. Insurance claims are processed much faster, allowing patients to complete treatment faster, speeding up workflow for the dentist and his or her staff, and, ultimately, receiving payment for completed treatment.
Digital radiography is revolutionary in respect to communication between dentists and specialists, dental technicians, and insurance companies. Very often it is necessary for a patient to go from one office to a second within a short period of time, at times even within the same day. The receiving dentist will have all of the necessary information by the time the patient arrives, along with digital radiographs that were E-mailed by the referring dentist. The patient benefits from this technology with timely comprehensive care, especially in emergency situations.
Laboratories are often sent a radiograph depicting an emergence profile that is potentially causing a periodontal issue. A digital film will often say a lot more than a written paragraph of explanation. The outcome of esthetic dentistry relies on very accurate communication with a laboratory technician. The use of digital imaging and radiography has raised the bar for outcome.
Multiple-Discipline Benefits
Every discipline in dentistry can profit from using digital radiography. Clinicians placing dental implants will find they are placing them far more accurately, even if a 3-dimensional study was done before surgery. Periodontists making use of the enhancement tools are able to compare previous-year images to measure treatment progress. Endodontists can obturate and fill with more confidence and certainly with more speed. Restorative dental procedures are done with more confidence, and with deep restorations and crowns on implant abutments, excess cement can be detected in the sulcular tissues (such as shown in Figure 6). Laboratory and CAD/CAM restorations can be easily checked for fit and emergence profile. Oral surgeons and pathologists can be better prepared to make a diagnosis, and quickly check progress with implant placement and other surgical procedures (Figure 8). Pedodontists and orthodontists can more efficiently track a growing or shifting dentition.
Many practitioners of all dental disciplines who use this technology find that their patients have a better connection—and commitment—with the goals set forth in their treatment plan, which ultimately strengthens the doctor-patient relationship.
File Storage
It would be prudent to mention that if a dentist makes the investment in a digital radiography system, he or she should take steps away from a single-site file storage system. Any failure of the hard drive or destruction by fire or water damage would be disastrous. It is strongly suggested to have the largest available hard drives, to regularly back up those hard drives, and also ensure off-site data storage so that valuable radiographic records are not lost.
Conclusion
For the last 15 years, it has been the perception by many that dentistry is product-driven. It is now safe to say that there is definitive science that has made technology possible. Dentists who have not closely looked at digital radiography should do so. It will raise the level of the practice and make the dentistry more rewarding.
References
1. American Dental Association. 2006 Technology Survey. Available at: https:/www.ada.org/members/sections/professionalResources/06_tech.pdf.
2. Kantor ML. Dental digital radiography: More than a fad, less than a revolution. J Am Dent Assoc. 2005;136(10):1358-1362.
3. Bedard A, Davis TD, Angelopoulus C. Storage phosphor plates: How durable are they as a digital dental radiographic system? J Contemp Dent Pract. 2004;15(2):57-69.
4. Christensen GJ. Why switch to digital radiography? J Am Dent Assoc. 2004;135(10):1437-1439.
5. Neff AW. Using visual technology for case presentation. Inside Dentistry. 2010;6(3):78-80.
About the Author
Jeffrey A. Watson, DDS
Private Practice
Syracuse, NY