Fully Digital Same-Day Restorative Dentistry
In-office design and milling can provide laboratory-quality crowns for busy patients
John C. Flucke, DDS
The desire for practical solutions to fabricate laboratory-quality restorations in the office has been around for nearly as long as modern dentistry itself. The potential benefits of in-office fabrication include greater efficiency and patient convenience as well as significantly lower overhead costs,1 and quality control improves as the doctor establishes and monitors standards for each step of the process. In addition, eliminating the transportation time to and from the laboratory (or just from the laboratory in cases involving digital impressions), can help to prevent unexpected delays in performing the restorative procedures, which are inefficient for the practice and aggravating for patients. Furthermore, the long-term cost savings resulting from the reduction in laboratory fees and office overhead for straightforward procedures more than justifies the initial capital outlay for the necessary equipment and materials.
Early Solutions
In the analog days of dentistry, before the influx of digital solutions that started in the late 1980s, the only way for practices to facilitate the in-office fabrication of restorations was to create an actual dental laboratory in the practice. This posed several problems, the greatest of which was the required square footage because most dental offices were not architecturally designed with the concept of including an in-office laboratory facility. The investment in building or expanding into additional office space and acquiring the necessary laboratory equipment to achieve an end result of reducing the delivery date by a few days was not financially attractive for most private practices. Accordingly, most offices continued to rely on off-premises independent dental laboratories to fabricate their prostheses.
In the late 1980s and early 1990s, the reality of increasingly cost-effective and powerful computer technology brought with it the promise of moving the profession of dentistry toward the goal of an all-digital workflow that offered clinical predictability and economic efficiency. Digital imaging could be used to replace physical impressions, and CAD/CAM processes could be used to create in-office restorations based upon a digital design.2 Unfortunately, the technology of this time period was not advanced enough for dentists to predictably create restorations that could rival those made by human hands.3 Although analog fabrication methods, such as the lost wax technique, were not very efficient, from the standpoint of clinical acceptability, they were predictable and accurate.
A significant drawback of these initial systems was that much of the CAD portion of the process still had to be completed in the mind of the operator. On the screen, users were shown points on a 2D graph that indicated the margin, height of contour, etc. This 2D rendering of what was essentially a 3D problem meant that the user had to conceive a 3D solution in his or her mind and then extrapolate it into points on the 2D graph. Because some users were unable to accurately think and visualize in three dimensions, the results were often less than ideal.
Another drawback to these initial systems was the issue of compatibility. In the early days of CAD/CAM, both acquisition and fabrication units were designed, developed, and manufactured by the same company. This had the benefit of ensuring that the different components worked well together because the hardware and software were tightly integrated. However, it also limited competition and the innovation that competition encourages, which increased initial purchase costs as well as back-end maintenance and service fees because the high cost of switching between these closed systems essentially made the owners captive to their chosen manufacturers.
Contemporary Same-Day Dentistry
Due to ongoing development and exponential increases in computing power, it is now possible to render both digital impressions and prosthetic designs in 3D. This 3D rendering allows the user to visualize the actual digital scan on the screen, rotate it, and manipulate it in a variety of ways. It also allows prostheses to be designed on the digital impression, which provides users with the feeling that they are working in a real-world scenario while they are using the digital tools.4 Furthermore, the development of open systems that enable plug-and-play compatibility between intraoral scanners, design software applications, and chairside mills has become the new standard, and this has increased innovation and flexibility while driving down the cost of ownership.
Technology for the in-office fabrication of restorations has made tremendous strides, and today's systems have largely overcome the limitations of their predecessors. Users of current in-office design applications and milling machines have found that these state-of-the-art solutions produce restorations with fit and function that is on par with traditional fabrication methods as well as offer significant efficiencies and cost benefits—all while enabling the dental team to provide laboratory—quality restorations in record time.5
Case Report
A 61-year-old male patient presented to the practice for an emergency appointment with the chief complaint that he had "a broken tooth on the lower left." He had a history of hypertension and clenching/bruxism and used both a continuous positive airway pressure (CPAP) machine and a mandibular advancement device to combat his obstructive sleep apnea. A patient in the practice for many years, his dental history included multiple tooth fractures that resulted from the presence of large preexisting amalgam restorations combined with the effects of his clenching/bruxism habit. In addition, the patient had a very busy professional schedule, which made it difficult for him to find free time for dental appointments.
Evaluation and Treatment Planning
A clinical examination of the patient's lower left quadrant revealed a large fracture of his mandibular left first molar (ie, tooth No. 19). Many years prior, when the patient first presented to the practice for a new patient exam, it was noted that this molar had been previously treated with a large occlusal amalgam restoration. During the patient's time in the practice, this existing restoration began to fail, exhibiting recurrent caries at the margins. As a result, the existing restoration was removed, and the tooth was treated with a large indirectly fabricated occlusal inlay that was bonded into place approximately 15 years ago.
Although this reinforcement of the natural tooth structure with a bonded restoration produced a result that was successful for 15 years, the inlay encompassed approximately 80% of the intercuspal distance between the distobuccal cusp and the distolingual cusp and approximately 90% of the intercuspal distance between the mesiobuccal cusp and the mesiolingual cusp. In addition, the original amalgam preparation had a depth of approximately 5 mm to 6 mm from the cavosurface margin to the pulpal floor. When the indirectly bonded inlay was placed, it was hoped the bond strength would help to reinforce and strengthen the unsupported lingual cusps. However, the loss of the interocclusal supporting tooth structure and the weakened and unsupported lingual cusps were allowing cuspal flexure to occur, and over time, this had resulted in fracture lines as the tooth flexed under occlusal loading.
During the patient's current examination, it was noted that the fracture involved the loss of the distolingual cusp, starting at the lingual groove, and progressed from the distolingual cusp across the distal marginal ridge, resulting in partial loss of the distobuccal cusp. Due to the amount of natural tooth structure lost to fracture, the decision was made to restore the tooth with a full coverage crown.
On the day of the emergency examination and evaluation, the staff acquired multiple photographs (Figure 1 through Figure 3) as well as an intraoral scan (iTero Element® 5D Plus, Align Technology) to allow the doctor to study the case preoperatively and treatment plan accordingly. The patient was not experiencing any pain and there was no prospect of it developing, so he was scheduled for his next appointment and dismissed without receiving an interim restoration.
Same-Day Restorative Appointment Scheduling
When scheduling a case for which the restoration will be fabricated in-office, the patient can be given the choice of never leaving the office or returning for final cementation later that same day. Although some patients choose to wait, many patients choose to return later in the day. When asked, patients generally indicate that their lives are so busy that they would prefer to accomplish tasks during the downtime as opposed to waiting in the office. Those cases are generally scheduled to begin in the morning and then cemented as the last procedure of the day. This allows the final restoration to be fabricated during the lunch hour to keep to the same-day schedule and makes fabrication of a temporary restoration unnecessary.
For the patient in this case, his busy schedule made the prospect of same-day dentistry very appealing. On the appointment day, the patient was available from 9:00 AM to 10:00 AM in the morning and also had a 30-minute slot available in the afternoon. The plan was to perform the preparation in the morning at 9:00 AM and then deliver the final prosthesis at 4:00 PM. The patient was extremely pleased and excited about the prospect of being able to complete the entire procedure from beginning to end in a single day. To accomplish this task, the primary digital technologies that would be utilized were an intraoral scanner, design software, and a chairside mill.
Material Selection
Taking into consideration the patient's history of clenching and bruxism, the material chosen for the restoration was a nano-ceramic hybrid CAD/CAM block (Grandio® blocs, VOCO). This material is a nano-ceramic hybrid resin that is 86% filled. Because of its high filler content, the material's modulus of elasticity and function under thermocycling are very similar to that of natural tooth structure. It also wears in a way that is very similar to enamel, which was beneficial in this particular case because the patient had known clenching and bruxing issues.
The primary benefit of using this material for an in-office same-day procedure is that the CAD/CAM blocks do not require firing in a porcelain oven. This is a tremendous time saver for this type of procedure. Once the milling process is complete and the material is polished with a porcelain polishing system, its finish has the appearance and feel of a material that was fired and glazed.
Preparation and Scanning
The patient presented for the appointment, and profound anesthesia was quickly achieved using 18 mg lidocaine with 0.009 mg epinephrine delivered with a PDL syringe (Paroject®, Septodont) and a 30-gauge ultra-short needle (Septoject®, Septodont). The tooth was then prepared with a chamfer margin to provide adequate material thickness and to aid in the detection of the margin with an intraoral scanner.
After the initial reduction was completed, a buildup material (PermaFlo™ DC, Ultradent) was placed using a total-etch technique with a 40% phosphoric acid etchant (Velvet Etch™, Vista Apex) and a universal adhesive (RE-GEN™, Vista Apex). All of the curing was accomplished with a handheld laser light curing unit (Monet® Laser Curing Light, CAO Group). Once the buildup material was placed and cured, it was shaped to establish resistance and retention form, and the margins were finalized (Figure 4 and Figure 5). A visual check of the interocclusal distance was performed to ensure that adequate occlusal reduction had been provided. Because the impression was to be captured digitally, the digital scan would indicate any insufficiency requiring further reduction.
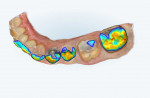
Following preparation, the margins were troughed using a diode laser (Picasso+®, AMD Lasers) with a 400-μm diameter tip that was set to deliver 0.5 W of power in the continuous wave mode. This was done to enable better visualization of the margins by the digital impression scanner. After laser troughing, the margins and preparation were digitally scanned, and the resulting "iRecord" file was visually inspected for integrity on the screen. Next, the occlusal surface was checked for proper reduction using the occlusal clearance tool included in the intraoral scanner's software. The occlusal clearance tool is applied after both arches are scanned and the teeth are imaged in maximum intercuspation. This tool determines the distance between the occlusal surface of the prepared tooth and the occlusal surface of the opposing dentition (Figure 6 through Figure 8) and lays out a color map indicating the proximity of the different areas of the surfaces (Figure 9). If inadequate reduction is noted, the preparation can be further reduced, and that area of the scan can be quickly and easily re-imaged to confirm that adequate reduction has been achieved and that the prosthesis will have adequate bulk to resist fracture during long-term occlusal loading.
Design and Fabrication
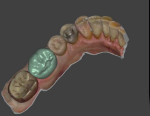
In this case, the preparation, margins, and occlusal reduction were all deemed clinically acceptable, so the scan was saved as a stereolithography (STL) file and uploaded to the manufacturer's cloud site directly from the acquisition unit. Next, the file was downloaded to the design computer, and the design software (DentalCAD, exocad) was used to create the prosthesis in a series of steps that started with the margins and ended with a completed crown (Figure 10 and Figure 11). Once past a brief learning curve, users can digitally design a prosthesis in approximately 10 minutes. The completed prosthetic design was then saved and opened in the chairside mill's software application (VPanel for DWX, Roland DGA). This software takes the digital design and translates it into a format that can be used by the mill to create the physical restoration. It also monitors the milling process and tracks bur life as well as indicates when routine maintenance is required.
The CAD/CAM block was placed into the mill (DGSHAPE DWX-42W, Roland DGA) and secured in place, and the restoration was milled into its final shape in approximately 20 minutes. This 4-axis mill features a 6-station automatic tool changer that allows it to switch tools during milling so that the most advantageous bur is used during every step of the fabrication process. The device is connected to the office's network via a wired Ethernet or Wi-Fi connection for transfer of the design file. In addition, it is connected to the office's compressed air system and requires a pressure of 0.3 MPa or higher.
Upon completion of the milling, the finished crown was removed from the mill and separated from the remaining portion of the block by hand with a coarse cylinder diamond bur. The polishing was then accomplished with a universal polishing system (Jiffy™ Universal Ceramic Adjusters and Polishers, Ultradent). Because the material used for the prosthesis did not require glazing and firing in an oven, the final polishing was completed in 5 minutes. As this case demonstrates, skilled providers using these methods to provide same-day crowns can anticipate only needing approximately 30 minutes to complete the design, fabrication, and polish.
Final Restoration
The patient returned for delivery of the crown at the appointed time. The restoration was tried in, and no adjustments were deemed necessary. The intaglio surface of the restoration was then treated with a silane coupling agent (Ceramic Bond, VOCO) for 60 seconds and then dried for 5 seconds with oil-free air. Next, the preparation was total etched for 10 seconds using a 40% phosphoric acid gel (Velvet Etch™, Vista Apex) and then rinsed for 5 seconds with water and dried briefly with a gentle stream of oil-free air. The dentin was left moist but with no puddling of water. After etching, the preparation was scrubbed with a dentin bonding agent (Futurabond® U, VOCO) and a gentle stream of oil-free air was applied for 5 seconds to evaporate the solvent.
To lute the crown into place, it was filled with a dual-cure luting agent (Bifix® QM, VOCO) and placed onto the preparation. Microbrushes were used to clean the excess extruded cement from the margins, and dental floss (Oral-B® Glide Floss, Procter & Gamble) was used to clean the interproximal surfaces. Once all of the visible extruded material was removed, the cement was set using the handheld laser light curing unit. The margins were then reevaluated to ensure that all of the excess cement was completely removed, and the patient was dismissed (Figure 12 and Figure 13). The restoration has had an uneventful history since placement.
Conclusion
During the last 5 years, the technology enabling fully digital same-day procedures has evolved at an even more accelerated pace. These state-of-the-art solutions for fabricating in-office restorations have achieved levels of accuracy, predictability, and esthetics that rival laboratory-produced restorations. Presently, the hardware and software meet critical thresholds regarding ease-of-use, reliability, compatibility, and cost that make the provision of same-day restorations accessible and even practical for private practices and their teams. With the currently available digital tools, the vision of delivering high-quality same-day restorations to patients while achieving excellent clinical outcomes is finally a reality.
About the Author
John C. Flucke, DDS
Chief Dental Editor and Technology Editor
Dental Products Report
Private Practice
Lee's Summit, Missouri
References
1. McLaren EA. CAD/CAM dental technology: a perspective on its evolution and status. Compend Contin Educ Dent. 2011;32(4):74-75.
2. Seelbach P, Brueckel C, Wöstmann B. Accuracy of digital and conventional impression techniques and worklfow. Clin Oral Investig. 2013;17(7):1759-1764.
3. Miyazaki T, Hotta Y, Kunii J, et al. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J. 2009;28(1):44-56.
4. Blatz MB. Chairside digital dentistry: a review of current technologies. Compend Contin Educ Dent. 2021;42(10):602-605.
5. Blatz MB, Conejo J. The current state of chairside digital dentistry and materials. Dent Clin North Am. 2019;63(2):175-197.