Posterior Tooth Preparation for All-Ceramic Restorations
Understanding material-specific requirements is essential to success
Awab Abdulmajeed, DDS, MS
The combination of computer-aided design/computer-aided manufacturing (CAD/CAM) technologies and modern dental ceramics has revolutionized indirect restorative dentistry. With the availability of high-quality digital workflows, the design and fabrication of definitive restorations has become a common clinical practice. The delivery of a properly fitted, well-contoured, and structurally strong ceramic restoration is highly dependent on proper material selection and excellent tooth preparation. Furthermore, the tooth preparation requirements themselves are dependent on material selection.1 Therefore, it is imperative that clinicians thoroughly understand the properties of dental ceramics and their preparation requirements. The two primary categories of modern ceramics available are glass-ceramics (eg, lithium disilicates,) and oxide ceramics (eg, zirconia). Due to the monolithic nature of these materials, they offer sufficient mechanical properties and acceptable esthetics and can be predictably machined.2
Material-Specific Preparation
After a material has been selected for an indicated clinical procedure, its specific needs will affect the tooth preparation that follows.
Lithium Disilicate
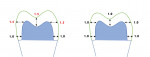
When preparing a tooth for a glass-ceramic restoration, it is very important to perform sufficient reduction. Glass-ceramic restorations require a significant occlusal and axial thickness in order to withstand functional forces and avoid bulk fracture.3 When using lithium disilicate, it is recommended to provide tooth reduction that allows for a minimum thickness of 1.5 mm on the occlusal and axial surfaces with a 1 mm of margin width; however, the minimum thickness can be reduced to 1 mm for all surfaces if these restorations are to be adhesively cemented using a resin cement (Figure 1).4
Zirconia
Zirconia (ie, zirconium dioxide) is widely used in its monolithic form as an all-ceramic restoration. The material is unique because it provides high strength and acceptable esthetics at a minimal thickness.5 Although monolithic zirconia restorations can be fabricated with surfaces as thin as 0.6 mm, the minimum thickness required can vary depending on the type of zirconia used. Zirconia is usually doped with yttria (ie, yttrium oxide), a component that stabilizes it at room temperature. The mol% yttria content has a direct effect on the mechanical and optical properties of zirconia. Increasing the mol% yttria content results in a more translucent zirconia, but this occurs at the expense of strength because it makes the material weaker. Therefore, it is crucial to know what specific type of zirconia is to be used because that will affect the tooth reduction requirements. There are many zirconia types provided by different manufacturers. The greater the mol% yttria content of zirconia, the greater the tooth reduction required to compensate for the loss of strength. Based on data provided by multiple studies, preparation requirements for the different types of zirconia can be recommended, including the following6-8:
• 3Y zirconia: 0.8 mm to 1.0 mm of occlusal and axial reduction
• 4Y zirconia: 1.0 mm to 1.2 mm of occlusal and axial reduction
• 5Y zirconia: 1.2 mm to 1.5 mm of occlusal and axial reduction
General Requirements for All-Ceramics
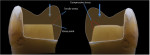
Regardless of the type of all-ceramic material to be used, there are certain general considerations for preparation design for these restorations that should be respected. Appropriate tooth reduction that follows the anatomy of the original tooth is required. This will ensure a uniform restoration while meeting the minimum thickness requirements for all surfaces. In addition, sharp internal line angles and edges as well as abrupt transitions should be avoided. All internal aspects of the tooth preparation should be rounded and smooth. This is necessary to prevent unfavorable tensile stresses from developing within the restoration, which are a common cause for ceramic failure. Rounded edges help to distribute the occlusal load more favorably and result in compressive stresses, which are well tolerated by modern ceramics (Figure 2).
The tooth preparation finish line is another element that requires detailed attention. The finish line should provide approximately 1 mm of space to permit sufficient material thickness at the crown margin area. If the restoration margins are thin, there is a greater chance that they may chip or fracture during the manufacturing process. The two recommended finish line configurations are rounded shoulder and heavy chamfer; however, whatever configuration is chosen, the finish line should be even, smooth, and continuous. If the finish line is rough, has significant irregularities, or has a J-shaped cavosurface margin, the crown will not have an optimal fit. This is due to the fact these are very small defects that cannot be machined by the milling tool during the fabrication process. Therefore, these areas will be overmilled, resulting in an increased marginal discrepancy. When properly designed and fabricated, contemporary all-ceramic restorations offer a clinically acceptable marginal fit.9
Clinical Significance
The success of a posterior indirect restoration depends on appropriate material selection and correspondingly appropriate tooth preparation. To ensure optimal outcomes, it is critical that clinicians understand the properties of the available all-ceramics and their material-specific reduction requirements. Modern materials and fabrication processes can provide a well-fitted ceramic restoration when the tooth preparation is of high quality.
About the Author
Awab Abdulmajeed, DDS, MS
International Dentist
Program Director
Assistant Professor
Department of General Practice School of Dentistry
Virginia Commonwealth University
Richmond, Virginia
References
1. Atlas A, Isleem W, Bergler M, et al. Factors affecting the marginal fit of CAD-CAM restorations and concepts to improve outcomes. Curr Oral Health Rep. 2019;6(4):277-283.
2. Sulaiman TA. Materials in digital dentistry-a review. J Esthet Restor Dent. 2020;32(2):171-181.
3. Rekow D, Zhang Y, Thompson V. Can material properties predict survival of all-ceramic posterior crowns? Compend Contin Educ Dent. 2007;28(7):362-368.
4. IPS e.max® CAD | IPS e.max ® Press: Adhesive 1 mm crown. Ivoclar Vivadent website. https://www.ivoclar.com/medias/IPS-emax-CAD-Press-Adhesive-1mm-Crown.pdf. Published November 14, 2016. Accessed June 16, 2022.
5. Leitão CIMB, Fernandes GVO, Azevedo LPP, et al. Clinical performance of monolithic CAD/CAM tooth-supported zirconia restorations: systematic review and meta-analysis. J Prosthodont Res. 2021;JPR_D_21_00081.
6. Abdulmajeed A, Sulaiman T, Abdulmajeed A, et al. Fracture load of different zirconia types: a mastication simulation study. J Prosthodont. 2020;29(9):787-791.
7. Alraheam IA, Donovan T, Boushell L, et al. Fracture load of two thicknesses of different zirconia types after fatiguing and thermocycling. J Prosthet Dent. 2020;123(4):635-640.
8. Stawarczyk B, Frevert K, Ender A, et al. Comparison of four monolithic zirconia materials with conventional ones: contrast ratio, grain size, four-point flexural strength and two-body wear. J Mech Behav Biomed Mater. 2016;59:128-138.
9. Tsirogiannis P, Reissmann DR, Heydecke G. Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: a systematic review and meta-analysis. J Prosthet Dent. 2016;116(3):328-335.e2.