History-Centered Diagnosis
A thorough subjective examination enables differential diagnosis and guides the objective examination
Brooke Blicher, DMD | Rebekah Lucier Pryles, DMD
Diagnosing endodontic disease requires the careful compilation of subjective and objective data. The information obtained from patients during the subjective examination guides the gathering of objective data during the clinical and radiographic examinations. Modern endodontic diagnosis is both minimally invasive and accurate, particularly with the advent of three-dimensional radiography and replicable testing. Clinical and imaging modalities facilitate the differentiation of odontogenic symptoms from nonodontogenic facial pain.
Diagnosing From Afar
The COVID-19 pandemic upended the diagnostic abilities of many practitioners when mandated practice closures in the spring of 2020 limited their ability to collect clinical and radiographic data.1 Clinicians were implored to manage patients pharmacologically and limit in-person encounters to only those patients whose conditions were unresponsive to medications. Office visits were also predicated on the availability of appropriate personal protective equipment, including N95 respirators. Despite these limitations, clinicians maintained the ability to obtain historical data from patients. The adoption of telehealth facilitated this information gathering both during the industry-wide shutdown and afterward in situations involving patients prohibited from in-person office visits due to active quarantines secondary to illness, travel, or direct exposure to COVID-19.2
This adoption of telehealth highlighted the utility of the subjective examination in facilitating endodontic diagnosis and served as a useful reminder of its inherent value. For a time, dental healthcare providers were forced to utilize phone or video conferencing to triage emergencies, prescribe medications, and plan for both acute and long-term management. Although video conferencing and intraoral photographs taken on patients' smartphones could, in some cases, allow clear visualization of certain issues, such as extraoral swelling, the vast majority of telehealth encounters relied solely on verbal communication. Patients' reports of symptom development, progression, and current presentation were used to elucidate differential diagnoses, which could then be followed up with pharmacologic management or the delivery of definitive emergency care in the dental office.
Information obtained during these subjective exams offered an effective means to triage patients into appropriate pharmacologic management as well as follow-up care. Many endodontists in regions with mandated office closures that permitted exceptions for only the most severe dental emergencies used teledentistry encounters to manage patients in challenging situations, both infectious and inflammatory. Oftentimes, patients provided a history of known etiology. They reported issues such as broken teeth, deep caries, or otherwise diagnosed dental disease that had been delayed, and they relayed their symptoms of swelling and pain. Through an assessment of these reported symptoms, clinical judgment could be used to determine whether infectious or inflammatory pathoses were the likely source. Patients with suspected infections often reported swelling, which was, in many cases, visible via videoconferencing. For these patients, antibiotics were prescribed, and follow-up consultations were scheduled via telephone. Because antibiotics are expected to take effect within 48 hours,3 in-office management could be scheduled if relief was not felt beyond that time period.
Patients who presented with severe pain that was not obviously due to infection posed greater challenges. In some cases, these patients reported suffering for days with severe pain that was unresolved by over-the-counter analgesics. That fact alone was sufficient to raise suspicion of the presence of symptomatic irreversible pulpitis for which antibiotics would have no effect.4,5 For these patients, as long as no contraindications were identified from the medical history, evidence-based pharmacologic analgesia was recommended. If their pain was unresponsive, patients were scheduled for care.
To arrive at a differential diagnosis based solely on the subjective exam, it is critical for clinicians to understand all of its necessary components.
The Subjective Exam
The subjective exam (see Components of the Subjective Exam) should always commence with obtaining the patient's chief complaint in his or her own words.6 Patients can be prompted by open-ended questions such as, "What brings you in today?" The chief complaint communicates the patient's motivations for seeking care. For example, if a patient's chief complaint involves hypersensitivity to cold, the history of the present dental illness will center around when and how the cold sensitivity occurs. Asking questions about specific symptoms may be necessary if a patient fails to sufficiently elaborate. In this example involving cold hypersensitivity, the patient should also be asked if he or she experiences heat sensitivity or pain when biting. Beyond questioning thermal sensitivity that is suspicious of symptomatic irreversible pulpitis, whenever infection is suspected, patients should also be asked about the presence of swelling or any drainage that could be indicative of the presence of a sinus tract. The history of the present dental illness should include information about the onset, duration, localization, and intensity of symptoms as well as any alleviating or exacerbating factors. In addition to the history of the present illness, the subjective exam also involves acquiring a past dental history of the area in question.6
A timeline of symptoms, including their onset, duration, and continuity, should be established. Regarding pain, onset refers to the first time that symptoms were noticed. Patients should be specifically asked if the pain occurred at any point in the past, especially if symptoms are no longer present, because a history of pain is considered a risk factor for future endodontic involvement.7 Duration refers to the length of time that symptoms last when they occur. Have they been present for days, weeks, or months? If they occurred in the past, for how long? When symptoms occur, are they constant, intermittent, or episodic?
Localization refers to a patient's ability to identify a particular tooth as the source of symptoms. Patients should be questioned with respect to the locality of pain. Does it remain isolated to a single tooth or the dentition in a single arch? Does it move between dental arches? Does it affect non-dental structures? Although referred pain is common, patients may have perceptions regarding the general vicinity of symptoms. Orofacial pain due to pulpitis can be difficult to localize, whereas pain caused by infection affects the nociceptive fibers in the periodontal ligament specific to the tooth, making it easier to localize.7 Referred pain is more common among maxillary and mandibular posterior teeth, is less common in anterior teeth,7 and can radiate to extraoral areas of the face and head. Referred pain originating from the mandibular molars will commonly be experienced in the ipsilateral ear.7
To quantify the intensity of pain, patients are often asked to rate it on a scale of 0 to 10, in which 0 represents no pain and 10 represents the worst pain imaginable. In certain cases, patients will delineate feeling differing intensities at different times, indicating episodic waves of pain. Pain intensity is subjective, and pain is experienced differently by different members of the population; therefore, reports of severe pain should be treated as such.
Alleviating factors are any actions reported by the patient that relieve pain, which includes taking medications. In cases of degenerative pulpitis, the application of cold may offer relief, and patients will often report swishing cold ice water to provide a few minutes of solace. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen are classically the best analgesics for inflammatory pain, including that of endodontic origin.8 Conversely, exacerbating factors are those stimuli reported by the patient that produce pain, which can include cold, heat, and biting pressure. Geographic location may play a role in the types of exacerbating factors reported. For example, clinicians in northern New England communities have observed that patients will oftentimes report pain that is exacerbated by going outside during the winter months, whereas those who practice in the desert southwest have found that patients oftentimes report pain that is exacerbated by spicy foods.
Beyond collecting all of the information about the symptoms of the present dental illness, the subjective examination should garner a past dental history of the area in question.6 Both recent and older restorative, endodontic, or surgical treatments as well as a history of dental trauma in the area of concern can elicit potential etiologies for active endodontic disease.
Once the subjective examination is complete, the clinician should have the information necessary to permit the development of a differential diagnosis for the patient's symptoms. The objective examination can then be utilized to confirm the diagnosis so that appropriate treatment can be rendered. The following two cases illustrate how a thorough subjective examination helps to guide the objective examination in diagnosing endodontic disease.
Case Report 1
A 45-year-old female patient presented to her general dental practitioner with the chief complaint of being in the worst pain that she had ever experienced and not being able to find anything to relieve it. She reported that she had sought care with her primary care physician for acute, episodic facial pain 2 days prior to presenting for dental care. Suspecting trigeminal neuralgia based on the quality and intensity of the patient's pain, her physician prescribed carbamazepine and ordered a diagnostic magnetic resonance imaging (MRI) study to investigate a potential neurologic cause. However, because the MRI scan could not be immediately obtained, the patient's physician advised her to seek a dental consultation to rule out other potential etiologies. The patient's general dentist performed a limited oral examination and acquired a periapical radiograph (Figure 1) of the area around teeth Nos. 18 and 19, which demonstrated no obvious pathosis. In an abundance of caution, the patient was referred to the endodontics office for further investigation and to gain better visualization of the area through cone-beam computed tomography (CBCT) analysis.
The information acquired during the subjective examination conducted by the endodontist included a past dental history of crown placement on tooth No. 19. Although it was placed 2 years prior to the development of the current symptoms, the patient reported that it had demonstrated intermittent low-level cold sensitivity since that time. While characterizing the history of the present dental illness, the patient reported experiencing 4 days of episodic pain, during which intense waves of pain lasting about 10 minutes each occurred several times per day. She indicated that the pain was located on the left side of her face in the distribution of the mandibular branch of the trigeminal nerve. According to the patient, when the pain was at its worst, it was a 10 out of 10 in intensity; however, in between waves, it was approximately 3 to 4 out of 10. She reported that her history of pain was entirely spontaneous without any obvious source of exacerbation and noted that she experienced incomplete relief of her symptoms after taking 600 mg of ibuprofen and no change in her symptoms during the 48 hours since she began taking carbamazepine.
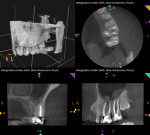
This patient's reported history of cold sensitivity, current symptoms (including their localization), and ability to achieve partial symptom alleviation with ibuprofen were suggestive of the development of a pulpal pathosis in the mandibular left quadrant; therefore, the objective examination was guided to explore this possibility. The clinical examination revealed intact restorations and normal periodontal findings. To replicate the patient's symptoms, pulp sensitivity tests and periodontal ligament tests were performed. Teeth Nos. 18, 19, and 20 were similarly tender to percussion, palpation, and biting. During cold testing, teeth Nos. 18, 20, and 21, exhibited normal responses; however, tooth No. 19 failed to exhibit a response. No clinical abnormalities were noted in the upper left quadrant. CBCT imaging was performed, which revealed widening in the apical region of the periodontal ligament of tooth No. 19 only (Figure 2).
Given the findings of the clinical and radiographic examinations, the diagnosis and suspected source of pain was pulpal necrosis with symptomatic apical periodontitis associated with tooth No. 19.5 The completion of root canal therapy for tooth No. 19 (Figure 3) resulted in resolution of the patient's symptoms, and her physician tapered her off of the carbamazepine without complication.
Case Report 2
During the mandated office closures of the COVID-19 pandemic, a 49-year-old male patient presented to the endodontist via telehealth for the assessment of severe pain affecting the left side of his face. His chief complaint was that his teeth were keeping him up all night. As a part of the history of the present dental illness, the patient reported experiencing unrelenting pain for a duration of 2 days that prevented him from sleeping. He indicated that the pain affected the left side of his face, jaw, and teeth without providing more specific localization and that it was at a constant intensity of 8 out of 10. In addition, he reported that taking a combination of 800 mg of ibuprofen and 1,000 mg of acetaminophen every 4 hours provided no relief; however, swishing ice-cold water around in his mouth offered a few minutes of pain reduction.
The patient's past dental history indicated that immediately prior to the mandated office closures, he underwent a dental examination that revealed a radiographic pathosis associated with previously endodontically treated tooth No. 14, severe periodontal involvement of teeth Nos. 16 and 17, and breakdown of the restorations on teeth Nos. 18 and 19. The recommended treatment, which included endodontic retreatment of tooth No. 14, extraction of teeth Nos. 16 and 17, and full-coverage restorations for teeth Nos. 18 and 19, had been delayed due to office closures. Presently, the patient denied experiencing any intraoral or extraoral swelling, loose teeth, bad tastes in the mouth, or particular areas of tenderness to pressing or chewing.
Although the patient remained very concerned about tooth No. 14 because he had been informed of the presence of an endodontic pathosis, his reported history was inconsistent with that of endodontic reinfection. The lack of any swelling or tenderness to pressure localized to this tooth suggested that the severe pain currently being experienced by the patient was originating from another source. Spontaneous, radiating pain of severe quality that can be relieved by ice water fits the diagnosis of a degenerating pulp rather than an acutely abscessed tooth. Therefore, antibiotics would have no expected effect.4
During nonpandemic times, antibiotic prescribing guidelines would have suggested the delivery of operative treatment and/or a delayed prescription of antibiotics to address a recurrent infection without swelling or signs of systemic spread.9 This patient hadn't slept in 2 days, and the prospect of a third sleepless night left him desperate for relief and raised concerns that he would need to seek care at an emergency room if pharmacologic agents continued to fail. Due to the presumed differential diagnosis and failure of pharmacologic agents to control pain, the patient's situation was considered an emergency, and he was scheduled for an immediate in-office assessment and treatment.
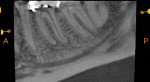
The information obtained from the subjective examination was used to guide the in-office objective examination. First, a comprehensive clinical examination was performed, which revealed well-adapted, full-coverage porcelain-fused-to-metal crowns on teeth Nos. 14 and 15, the partial eruption of teeth Nos. 16 and 17, and large amalgam buildups with stained margins on teeth Nos. 18 and 19. Gingival irritation was evident surrounding teeth Nos. 16 and 17. Next, sensitivity tests were performed. None of the teeth in the upper or lower left quadrants were sensitive to percussion, palpation, or biting; however, teeth Nos. 12, 13, 16, 17, 18, 20, and 21 responded normally to cold and electric pulp testing, whereas teeth Nos. 14, 15, and 19 were nonresponsive to both. CBCT imaging revealed evidence of a periapical pathosis on the mesiobuccal root of tooth No. 14, which was related to an untreated second mesiobuccal canal (Figure 4). In addition, maxillary sinus mucositis was present adjacent to tooth No. 14, and between teeth Nos. 15 and 16. Tooth No. 19 also demonstrated evidence of a developing apical pathosis (Figure 5).
The diagnosis for tooth No. 14 was previously treated with asymptomatic apical periodontitis. Tooth No. 19, however, was confirmed to have pulpal necrosis with asymptomatic apical periodontitis.5 These findings indicated that tooth No. 19 was the source of patient's pain given the recent nature of pulpal degeneration. Nonsurgical root canal therapy was performed on tooth No. 19, which resulted in resolution of the reported pain (Figure 6). Regarding tooth No. 14, plans were made to perform nonsurgical root canal retreatment following lifting of the COVID-19-related dental practice restrictions.
Conclusion
Mandated office closures during the COVID-19 pandemic highlighted the utility of the subjective examination in diagnosing endodontic pathoses. The chief complaint, the history of the present dental illness, and the past dental history provide the foundation for the clinical and radiographic examinations that serve to confirm or deny the differential diagnosis developed from the subjective information. Knowing which questions to ask and carefully listening to the patient's responses during the subjective exam are the first steps in providing relief for patients with acute endodontic disease.
About the Authors
Brooke Blicher, DMD
Assistant Clinical Professor
Department of Endodontics
Tufts University
School of Dental Medicine
Boston, Massachusetts
Clinical Instructor
Department of Restorative Dentistry and Biomaterials Science
Harvard University
School of Dental Medicine
Boston, Massachusetts
Upper Valley Endodontics
White River Junction, Vermont
Cofounder
Pulp Nonfiction Endodontics
Rebekah Lucier Pryles, DMD
Assistant Clinical Professor
Department of Endodontics
Tufts University
School of Dental Medicine
Boston, Massachusetts
Clinical Instructor
Department of Restorative Dentistry and Biomaterials Science
Harvard University
School of Dental Medicine
Boston, Massachusetts
Upper Valley Endodontics
White River Junction, Vermont
Cofounder
Pulp Nonfiction Endodontics
References
1. American Dental Association. ADA recommending dentists postpone elective procedures. ADA website. https://www.ada.org/about/press-releases/2020-archives/ada-calls-upon-dentists-to-postpone-elective-procedures. Published March 16, 2020. Accessed February 17, 2022.
2. Choi SE, Simon L, Basu S, Barrow JR. Changes in dental utilization patterns due to COVID-19 among insured patients in the US. J Am Dent Assoc. 2021. doi: 10.1016/j.adaj.2021.07.002.
3. Johnson M. Antibiotics and the treatment of dental infections. Endodontics: Colleagues for Excellence. Fall 2019.
4. Nagle D, Reader A, Beck M, Weaver J. Effect of systemic penicillin on pain in untreated irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(5):636-640.
5. Levin LG, Law AS, Holland GR, et al. Identify and define all diagnostic terms for pulpal health and disease states. J Endod. 2009;35(12):1645-1657.
6. Blicher B, Walton R, Torabinejad M. Chapter 4: Endodontic diagnosis and treatment planning. In: Torabinejad M, Fouad A, Shabahang S, eds. Endodontics: Principles and Practice. 6th ed. Elsevier; 2020:61-82.
7. Bender IB. Pulpal pain diagnosis-a review. J Endod. 2000;26(3):175-179.
8. Richards, D. The Oxford Pain Group League table of analgesic efficacy. Evid Based Dent 2004;5:22-23.
9. Lockhart PB, Tampi MP, Abt E, et al. Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling. J Am Dent Assoc. 2019;150(11)906-921.