Treating Wear From Bruxism in Autistic Patients
Crown-lengthening surgery offers conservative alternative to extraction and implant placement
Ahmad Soolari, DMD, MS | William E. Kelson, DDS
Autism is a developmental disorder with manifestations that include severe deficits in communication, and children with autism commonly engage in bruxism (ie, teeth grinding) during sleep.1 This habit can affect occlusion, mastication, speech, appearance, self-esteem, and quality of life. In the United States, an estimated 2.8% of children aged 3 to 17 years are diagnosed with autism. Some receive no treatment at all, whereas others are treated either with medication or behavioral therapy.2 The most frequent oral findings among autistic patients are bruxism, self-inflicted oral lesions, and malocclusions, and behavioral therapy is not expected to resolve bruxism.3
Because autism spectrum disorder inhibits communication and social interaction skills, the process of providing dental hygiene treatment and services to these patients is complex. Treating malocclusion, bruxism, pain, and severely worn-down dentition in patients with autism can be challenging, particularly because they have difficulty complying with the at-home care parts of the process.
Case Report
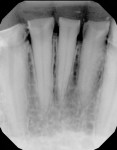
A 36-year-old male patient was referred for specialty care to coordinate a combined periodontal-prosthodontic treatment. The patient had a medical diagnosis of autism that required 24-hour home supervision as well as a history of incomplete restorative dentistry, bruxism, regurgitation, acid erosion, over-retained stainless steel crowns, enamel dysplasia, occlusal disharmony, teeth without clinical crowns, and major esthetic compromise. His condition resulted from a lack of an organized approach to oral care and rehabilitation. The patient's chief complaints were pain, tooth sensitivity, and difficulty eating. In addition, he had a history of excessive grinding and clenching of the teeth. Clinical and radiographic evaluations were performed, which revealed a severely worn-down dentition (Figure 1). In order to facilitate the necessary prosthodontic treatment that the patient required to regain dental function and improve his speech and esthetics, surgical crown lengthening was recommended. Following crown lengthening, the patient would be restored with dental crowns for teeth Nos. 19 through 30. This treatment plan was accepted by the patient and his caregivers.
Clinical Treatment
The treatment plan was coordinated with the referring dentist, who prepared the teeth and placed a temporary prosthesis prior to the crown-lengthening surgery (Figure 2). Because the patient's cognitive abilities and motor skills were developed enough to facilitate his cooperation during dental treatment, local anesthesia in the dental chair was sufficient to perform the crown-lengthening surgery. The patient and his parents were provided with education and motivated to perform an acceptable level of oral hygiene at home as well as advised to adhere to three rotational recall appointments between the offices of the periodontist and the primary care dentist.
Prior to the surgery, the patient was prescribed 500 mg of amoxicillin to be taken 3 times a day for 1 week and 600 mg of ibuprofen to be taken as needed. At the surgical appointment, the temporary prosthesis was removed from the mandibular teeth (Figure 3). Using a No. 12 blade (No. 12 Carbon Steel Sterile Surgical Blade, Benco Dental), envelope incisions were made from the distal aspect of tooth No. 18 to the distal aspect of tooth No. 31 to enable access to the root and bone via a full-thickness raised flap. Once the flap was elevated, osseous reduction was performed 360° around the teeth (Figure 4 through Figure 6). The flap was closed with 4.0 silk sutures, and then a periodontal dressing (COE-PAK™ AUTOMIX, GC America) was placed. The patient's healing progression following the surgical procedure was within normal limits.
The purpose of the crown-lengthening surgery was to increase the surface area of the crown preparations because minimal clinical crown was present. Four weeks after the surgery, the general dentist completed the crown preparations and took an impression, and the crowns for teeth Nos. 19 through 30 were delivered 2 weeks later (ie, 6 weeks after crown lengthening). The crowns were fabricated with an occlusal design that facilitated intercuspation, which limits lateral movement and reduces the potential for bruxing. At the 3-month recall appointment, the patient's parents stated that he was no longer grinding his teeth and was able to chew solid food properly. Photographs and radiographs taken 1 year after treatment demonstrate that all of the treated teeth are fully functional with no mobility, no widened periodontal ligament, no endodontic treatment, and no bleeding on probing (Figure 7 through Figure 12).
For this patient, crown-lengthening surgery produced a stable dental condition within 1 year with a concomitant decrease in clenching and grinding, which may possibly be attributed to a reduction in sensitivity following placement of the final crowns. Long-term care included increasing the frequency and efficiency of oral hygiene measures with the help of the patient's caregivers, application of a fluoride gel or rinse, intake of healthy noncariogenic foods, and frequent recall appointments. In addition, future treatment was discussed, which would focus on the upper jaw with similar management.
Discussion
Many individuals who have disabilities-physical or developmental-typically do not have the financial resources to obtain medical and dental care, and this can lead to progressively adverse effects. Ultimately, financial constraints become a deciding factor when considering possible treatment modalities. For the patient in this case report, the treatment options included saving teeth with minimal to no clinical crowns or extracting them and delivering a removable or fixed prosthesis. The fixed option would require the placement of dental implants following tooth extraction, and the incidence of implant-related complications is on the rise.
Most dental treatments for children with autism, who often have nutritional problems, are tooth extractions, and the rate of utilization of dental services for this group is low.4 The oral health status of children with autism can be negatively affected by factors such as eating problems, clenching and grinding behaviors, sleep disorders, and speech impediments; therefore, caregivers should be informed and encouraged to provide the dental care that patients with autism require.4
For the patient in this case report, clinical observation revealed severely worn-down dentition, loss of vertical dimension, and traumatic occlusion. Currently, the first treatment option that is usually recommended in the dental community for such a case is to remove the affected teeth and replace them with dental implants. However, in this case, crown-lengthening surgery offered a good therapeutic prognosis, especially considering that implant therapy was not a treatment of choice for this patient because of his grinding habit, the longevity of implants in patients with severely worn-down dentition does not surpass that of compromised but successfully treated natural teeth,5 and biologic and prosthetic complications commonly develop over time.6 Lang and colleagues estimated that up to 50% of implant cases develop complications within 10 years of insertion.7 With this patient's age of 36 and an expected life-span of 70 to 80 years, maintenance of the natural teeth was the best plan, and implants can still be considered when he is older should his natural teeth fail. Preservation of the natural dentition is typically preferred by patients and is economically justifiable.8 Because this patient required assistance with basic activities of daily living, it was assumed that his risk of developing complications from dental implants would have been higher,9 and that the cost of maintenance would be correspondingly higher than that of his natural teeth.10
Surgical crown lengthening must include the consideration of factors such as biologic width, attached gingiva, furcations, restorative needs (eg, ferrule), and the loss of bone support around adjacent teeth. In this case, the purpose of crown-lengthening surgery was to provide proper resistance and retention form for the restorations while avoiding biologic width invasion, which can feel like a splinter. This requires 3 mm of space between the margin of the restoration and the bone.
Prior to crown-lengthening surgery, it is highly recommended to break contact points, prepare the teeth, and place well-fitted provisional restorations that can be easily removed. Delivery of restorations following crown-lengthening surgery is rapid and simple because crown-lengthening surgery enables easier impressions, less stress for the primary care dentist, and more predictable results. The patient in this case report was happy with the outcome, and the restorative dentist was pleased with the efficiency of the work. The patient wanted restoration of his lost dentition and to be disease-free while the restorative specialist wanted to deliver a long-term restoration in a healthy environment. The provision of crown-lengthening surgery enabled the restoration of teeth that would otherwise have needed to be extracted, and the outcome of the team approach was restored function, stability, and an esthetic appearance.
When developing a treatment plan, dental professionals are taught to address the patient's chief complaint, but autistic dental patients may not be able to effectively communicate, which can complicate their oral healthcare. A personalized, preventive, and predictable treatment plan should be formulated. This requires the cooperation of parents or caregivers and a thorough understanding by the dentist and dental assistant of the individual patient's needs. When dealing with autistic patients, emotional skills are more useful than intellectual and clinical skills,11 and patients will vary in their behaviors and reactions to the dentist's commands. A dental appointment is a significant event for most patients but is especially stressful for the guardian of an autistic patient. Dental professionals should make the visit simpler and easier for everyone by reviewing the patient's medical, dental, and psychological history and preferences in advance. Parents of autistic children want to ensure that their child will receive personalized, attentive, and predictable care to minimize the number of future visits.
Proper preparation by the dental practice is essential. The practice should contact the patient's treating physician, educators, mental health counselor, and general dentist prior to the appointment to get to know the patient and his or her caregivers. Assign a specific staff member to extend a warm and welcoming phone call to the family, set up a short appointment, and fill out all of the necessary paperwork in advance in order to avoid an extended wait. Having to sit in the waiting room while administrative matters are handled can frustrate attention-deficient autistic patients. Not having to wait creates trust in the dental staff, and this trust is a currency for delivering successful treatment outcomes. The goal is to develop a long-term relationship in an office setting that minimizes anxiety so that you can provide quality dental care.
Other modifications to improve the treatment experience for autistic patients include minimizing distractions (eg, no staff members should enter the treatment room if they are not directly involved in the care of the patient) and limiting the noise to soothing, rhythmic music. In addition, ceiling lights may be turned off, the patient may be supplied with dark protective goggles with side shields to minimize peripheral vision, and the surgical area may be covered with a periodontal dressing to prevent the patient's access to the sutures and to increase comfort. Parents or caregivers should be educated about the procedure that will be performed and given both oral and written instructions for home care. A follow-up phone call should be made to ensure that the patient is not experiencing any pain, swelling, or discharge. Overall, the dental treatment and management of patients with autism requires a family-centered approach that addresses the concerns and preferences of caregivers in tandem with the needs and behaviors of patients.12 Oral home care for autistic patients should be tailored to suit their abilities and may include the use of an electric toothbrush, topical fluoride applied with a toothbrush, and due to their reduced ability to perform self-care, more frequent prophy appointments to aid in maintaining the restorations and prevent recurrent decay.
Concluding Remarks
For the patient in this case report, crown-lengthening surgery yielded a favorable long-term prognosis, allowing him to retain his natural dentition and avoid unnecessary extractions and the insertion of dental implants. Dentists should be tolerant with autistic patients and plan ahead for the factors involved in their visit and treatment in order to produce favorable results that benefit all parties involved.
The results of this case demonstrate that teeth with minimal clinical crowns can be retained with the aid of appropriate periodontal surgery. Crown-lengthening surgery increases the amount of coronal tooth structure available to retain restorations, preserving patients' natural dentition with good occlusal harmony. The treatment did not eliminate all of the etiological factors of bruxism, but it did alter the magnitude and direction of the condition by changing the occlusal scheme, which resulted in the elimination of pain as well as improved chewing efficiency, sleep patterns, speech, appearance, and psychological well-being.
About the Authors
Ahmad Soolari, DMD, MS
Diplomate
American Board of Periodontology
William E. Kelson, DDS
Private Practice
Silver Spring, Maryland
Member
Robert T. Freeman Dental Society
Private Practice
Gaithersburg, Potomac, and Silver Spring, Maryland
References
1. Muthu MS, Prathibha KM. Management of a child with autism and severe bruxism: a case report. J Indian Soc Pedod Prev Dent. 2008;26(2):82-84.
2. Xu G, Strathearn L, Liu B, et al. Prevalence and treatment patterns of autism spectrum disorder in the United States, 2016. JAMA Pediatr. 2019;173(2):153-159.
3. Orellana LM, Silvestre FJ, Martínez-Sanchis S, et al. Oral manifestations in a group of adults with autism spectrum disorder. Med Oral Patol Oral Cir Bucal. 2012;17(3):e415-e419.
4. Onol S, Kirzioğlu Z. Evaluation of oral health status and influential factors in children with autism. Niger J Clin Pract. 2018;21(4):429-435.
5. Holm-Pedersen P, Lang NP, Müller F. What are the longevities of teeth and oral implants? Clin Oral Implants Res. 2007;18(Suppl 3):15-19.
6. Derks J, Schaller D, Håkansson J, et al. Effectiveness of implant therapy analyzed in a Swedish population: prevalence of peri-implantitis. J Dent Res. 2016;95(1):43-49.
7. Lang NP, Berglundh T, Heitz-Mayfield LJ, et al. Consensus statements and recommended clinical procedures regarding implant survival and complications. Int J Oral Maxillofac Implants. 2004;19(Suppl):150-154.
8. Donos N, Laurell L, Mardas N. Hierarchical decisions on teeth vs. implants in the periodontitis-susceptible patient: the modern dilemma. Periodontol 2000. 2012;59(1):89-110.
9. Lindhe J, Meyle J, Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the sixth European workshop on periodontology. J Clin Periodontol. 2008;35(8 Suppl):282-285.
10. Fardal Ø, Grytten J. A comparison of teeth and implants during maintenance therapy in terms of the number of disease-free years and costs -- an in vivo internal control study. J Clin Periodontol. 2013;40(6):645-651.
11. Chandrashekhar S, Bommangoudar JS. Management of autistic patients in dental office: a clinical update. Int J Clin Pediatr Dent. 2018;11(3):219-227.
12. Gandhi RP, Klein U. Autism spectrum disorders: an update on oral health management. J Evid Based Dent Pract. 2014;14(Suppl):115-126.