Treatment Planning for Periapical Cemental Dysplasia
A carefully planned case takes an unexpected turn
Patient treatment planning represents a fusion of science, emotion, economics, and reality. Linear thinking and flow charts are a necessary prelude to the complexity all practitioners face while offering solutions to complex stomatognathic problem sets. The case study presented here concerns a patient with a cemento-osseous dysplasia who was experiencing occlusal disease. The carefully planned and accepted treatment was made more complex by the patient’s decision to change her course of treatment due to finances and her husband’s poor health. To accommodate this change, the decision tree had to be altered to optimize the patient’s treatment outcome at a critical point in her care.
Occlusal Disease
The cascade of events stemming from tooth loss is cumulative and can be catastrophic. Partial or full edentulation leads to patterns of osseous resorptive behavior. Intervention by dentists to create cost-effective interim treatments often includes removable partial dentures. Care must be taken in such cases, because factors such as fulcrum force and decay of abutment teeth can cause subsequent additional loss of teeth and bone over time. Attempts to monitor occlusion and maintain denture base stability through rebase and relines are often “too little too late.”
This leads to a domino effect, where missing teeth beget more missing teeth. For many, the inevitable endpoint will be dentures. The role of the dentist in performing denture dentistry cannot be overemphasized. Many practitioners offer “high-end,” “gorgeous” dentures, but the fees charged for these services may be better spent in efforts to improve retention, support, and esthetics prior to resigning a patient’s fate to complete dentures.
Cemento-Osseous Dysplasias
Osseous dysplasias are a group of disorders known to originate in the periodontal ligament tissues. These conditions are most prevalent in middle-aged African American women, but they have been seen in Asians and Caucasians as well.1-3 These lesions are the most common fibro-osseous lesions seen in everyday practice. They may represent a reactive or dysplastic process, but their etiology is unknown.
This group can be subdivided into three groups—periapical, focal, and florid—based upon radiographic appearance and location. Periapical cemento-osseous dysplasia (PCOD)—often referred to as cementoma—surrounds the apical area of the roots and is often bilateral. Focal cemento-osseous dysplasia (single lesion) and florid osseous dysplasia are limited to the jaws.
The lesions of PCOD are asymmetric and may be found in two or more quadrants in tooth or former tooth positions. These lesions have bony trabeculae and calcifications embedded in a fibroblastic matrix. PCOD is most prevalent in African American women.3
There are three different periods during which the lesions of PCOD may appear in radiographically differing presentations. The first is the osteolytic period, where areas of circular and elliptical resorptive lesions are seen. In the second, the cementoblastic phase, small calcifications appear within the lesions, which often look like a mixture of radiolucent and radiopaque lesions. The last phase, maturation, shows large calcifications, and some lesions can become very large without widening the cortex of the mandible.4
The diagnosis of PCOD requires biopsy, but the risk of infection or fracture negates the efficacy of surgical removal or biopsy unless the lesions are exposed and symptomatic. The greatest danger with PCOD is the possibility of developing osteomyelitis with extensive denture or partial denture wear.
These lesions can often look like a periapical lesion or granuloma on a tooth requiring endodontic therapy, but if pulp testing is performed, these teeth will be found to be vital.5
The concerns in treating a patient with PCOD include bone quality and the prognosis of dental implants for patients with this condition versus the risk of potential osteomyelitis from prolonged denture use. The bone quality of PCOD changes from vascular normal bone into avascular mixed cementum-ossifying lesions.6
Case Presentation
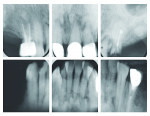
A female African American patient was diagnosed with PCOD based on the information in her radiographs. Associated teeth were tested and found vital and the patient presented with ill-fitting partials and root tips. Her chief complaint was pain while chewing and discomfort from the partials. Radiographically, the mixed lesions were seen in all four quadrants of her jaws, and were associated with the teeth that were present and those that were previously extracted (Figure 1).
The patient’s clinical presentation of edentulism and the subsequent use of partial dentures resulted in severe bone atrophy posteriorly (Figure 2 through Figure 5). The patient’s indecision regarding her future dental care led to broken crowns that were cemented daily with the partials until the pain led to a decision for definitive treatment.
The approach for treatment followed the principle “first, do no harm.” That meant that since the vascularity of the implant sites was compromised, the implants would be placed in edentulous areas and the areas of root tips to ascertain the viability of implant treatment to resolve the patient’s problems. In the event of complications, the treatment would be discontinued and dentures or precision attachment partials would be discussed.
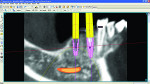
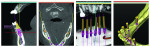
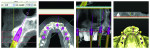
A cone-beam computed tomography (CBCT) scan was conducted and reformatted by 3D Diagnostics (www.3ddx.com) so that the implants’ placement could be planned with SimPlant® (Materialise Dental, www.materialisedental.com). The treatment modality selected was constructed so that the treatment would begin with three maxillary implants with a fixed bridge for the upper left quadrant and two implants in the No. 20 and No. 21 sites, which would be joined to future mandibular implants to fabricate a hybrid prosthesis or mandibular fixed implant bridge. The proper consent was received and the implants were placed during the first surgery.
Treatment Planning
The stages to planning this case were as follows.
Stage 1—Implants for the maxillary left bridge and two implants placed lower left to ascertain viability and integration.
Stage 2—Completion of the maxillary bridge.
Stage 3—Edentulation of the remaining mandibular teeth with additional implant placement in remaining anterior symphyseal bone between the mental foramina and right posterior molar area.
Alternatively, maintenance of mandibular teeth with placement of posterior mandibular implants only if patient decided to retain mandibular incisors.
Stage 4—Completion of the mandibular hybrid (cement-retained mandibular denture). This had the possibility of becoming a fixed bridge if the patient decided on the additional expense.
Stage 5—Maxillary edentulation with fixed bridgework to complete the full-mouth occlusal implant rehabilitation.
The reformatting done by 3DDX allowed virtual placement of the implants and measurements from the existing teeth and roots to be used for pilot osteotomy placement. The loss of tooth No. 10 after initial treatment planning led to a decision to place implant No. 11 at a mesial angle so that the antero-posterior distance of the bridge could be optimized.
The implant planning for the initial implant placement was viewed in the SimPlant planner (Figure 6 though Figure 10) and MIS’s SEVEN® implants (www.mis-implants.com) were chosen for placement due to their cost effectiveness; sand-blasted and acid-etched surface, which increased the surface area; sterile single final drill; and implant stability at placement. The placement of five additional implants post-edentulation and mandibular ridge leveling can be seen in the SimPlant full window view. The SimPlant treatment plan was designed to address the edge to edge anterior bite. This would be done by performing an osteoplasty of the mandibular anterior and placing the implants in a more uprighted position with respect to the existing mandibular dentition. Placement of implants inferiorly and lingually would allow for a modification from a splayed Class III to a Class I occlusal relationship. The removal of the anterior teeth combined with osteoplasty and implant placement in a more inferior position would allow for maintaining her existing vertical dimension of occlusion. The patient agreed to the cost and number of implants, but she was given the option to leave the remaining lower teeth and place smaller-diameter implants in the posterior regions, so a treatment variation was created for this scenario as well. She wasn’t certain whether she could approve full mandibular edentulation until she evaluated the initial procedure’s success. Lastly, the maxillary full-arch treatment was planned to facilitate phase 2 treatment and provide her with an upgrade path.7
The First Surgery
After following sterile protocol and administering anesthesia, the remaining root tips were removed with Physics Forceps™ (Golden Dental Solutions, www.physicsforceps.com) which create a fulcrum to aid in delivering the tooth atraumatically. These forceps are used with gentle forces applied by fingertips to facilitate the “pop” found when the tooth releases from the periodontal ligament within the socket (Figure 11). The root can then be delivered with a traditional forceps (Figure 12). By placing the bumper against the remaining alveolus, the sharp beak of the forceps can engage the remaining tooth structure and a gentle, steady pressure in an occlusal direction will help release the root while keeping the buccal plate intact.
Osteotomies were initiated and measured from tooth No. 10 distally prior to its extraction (Figure 13). MIS implants have a unique semi-conical geometry and display excellent condensing properties during placement.
The MIS SEVEN implant comes with a sterile, final, single-use placement drill, which exactly matches the shape of the implant selected in pre-treatment planning. The panorex of the post-treatment implant placement reveals placement of the “experimental implants” (Figure 14).
Treatment Planning Twist
The patient’s husband was admitted to the hospital with a serious medical emergency and the patient was concerned that the agreed upon treatment would be too expensive, given her upcoming hospital bills. So with the implants already placed, a compromise treatment plan had to be found. The problem was compounded by the realization that the occlusal vertical dimension increase, which was planned to create the adequate inter-occlusal distance for implant rehabilitation, would no longer be available.
The patient understood the limitations and an upper fixed bridge and removable partial denture (RPD) as well as an implant-retained lower partial denture (LPD) would be fabricated. The implants were uncovered and the stock abutments supplied with the implants were placed. Then the snap caps were placed upon the abutments so a closed tray impression could be made for construction of the bridge (Figure 15). The soft tissue contours, which were evident upon removal of the healing abutments, demonstrated good keratinized gingiva (Figure 16).
The MIS abutment selection kit was sent to the laboratory (Rapa Dental Ceramics) so technicians could select stock abutments that would require minimal milling to avoid incurring the cost of fabricating custom abutments. The laboratory ordered and milled the stock abutments and returned them on a seating jig made of primopattern resin (primotec USA, www.primotecusa.com) for intraoral delivery (Figure 17).
The seated abutments were verified radiographically and torqued to 30 NCm prior to cementing the maxillary bridge (Figure 18). The bridge was fabricated with guide planes, rest seats, and milled undercuts for the eventual upper partial denture, which would replace the maxillary right quadrant teeth until implants could be done in the maxilla at the next phase of treatment (Figure 19).
Working with Limited Vertical Dimension
Zest Locators (ZEST Anchors, www.zestanchors.com) were chosen for placement on implants 21 and 22 to retain the lower partial denture (Figure 20). The proper locator heights were selected by measuring from the top of the tissue to the platform of the implant after suitable healing. This number would normally be adequate, but due to the limited interocclusal space, 1 mm was subtracted to keep the locator head as close to the tissue as possible (Figure 21). The laboratory was instructed to place the male of the locator into the frame of the denture, and a tooth-colored acrylic was used as a facing for the teeth so that a minimal dimension of acrylic could be used, but it was still supported by the metal framework of the partial for strength (Figure 22).
The modification of the bridge to accept a removable partial denture was performed, as the maxillary implant rehabilitation would be postponed indefinitely. The upper partial, which was designed with a plate design, had rests, clasps, undercuts for clasps, and a bilateral balanced occlusion to decrease occlusal overload to the implant bridge and mandibular implants. Use of the bridge to retain the partial would further provide stability, support, retention, and cross-arch stabilization for the maxillary prosthesis (Figure 23).
The patient was extremely happy with the treatment results (Figure 24 and Figure 25). She was able to concentrate on her husband’s recovery without financial or emotional stress. The good will involved in helping the patient improve her condition sequentially based upon her emotional, personal, and financial readiness truly exemplifies the concept of “upgradeable dentistry” as described by the author.7
Conclusion
This case study demonstrates the flexibility and fluidity of dynamic treatment planning. Often treatment plans must be modified either due to dental change or unanticipated events. This treatment was undertaken to eliminate pain. The finances were agreed upon and the ability to make sure that implants would osseointegrate was the predicating factor to the final treatment decisions.
The patient was made aware that the best bone for implants in the mandible would be where the existing, mal-posed teeth were. The reality that two implants placed in sockets did in fact integrate was verification that mandibular edentulation with implant placement could be predictable. The factor that was not predictable was the illness of the patient’s husband and the financial burden she was experiencing.
The ability to work with the patient to overcome these obstacles, while still presenting her with a substantial improvement in her occlusion, led to a satisfactory outcome. The “upgradeable path” to her restorations is already planned, and when she is ready to proceed, she can anticipate a predictable plan to further improve her oral care. If she is satisfied with the outcome achieved, then the initial goals of occlusal and functional improvement have already been satisfied.
Disclosure
The author received minor honoraria from MIS, Golden Forceps, and 3DDX.
Acknowledgements
The author would like to thank Leszek Rapa, MDT, for his laboratory expertise at Rapa Dental Ceramics in Palm Harbor, Florida.
References
1. Gonçalves M, Píspico R, Alves Fde A, et al. Clinical, radiographic, biochemical and histological findings of florid cemento-osseous dysplasia and report of a case. Braz Dent J. 2005;16(3):247-250.
2. Loh FC, Yeo JF. Florid osseous dysplasia in Orientals. Oral Surg Oral Med Oral Pathol. 1989;68(6):748-753.
3. Pindborg JJ, Kramer IRH. Histological typing of odontogenic tumours, jaws cysts and allied lesions. 1st ed. Geneva: World Health Organization; 1971.
4. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial pathology. Philadelphia, PA: W.B. Saunders Company; 1995:464-465.
5. Smith S, Patel K, Hoskinson AE. Periapical cemental dysplasia: a case of misdiagnosis. Br Dent J. 1998;185(3):122-123.
6. Bencharit S, Schardt-Sacco D, Zuniga JR, Minsley GE. Surgical and prosthodontic rehabilitation for a patient with aggressive florid cemento-osseous dysplasia: a clinical report. J Prothet Dent. 2003;90(3):220-224.
7. Winter R. Upgradeable dentistry: Part 1. Dentistry Today: 2009;28:82-87.
About the Author
Richard Winter, DDS, MAGD
Private Practice
Milwaukee, Wisconsin
Fellow, ADI, ICOD
Mastership, AGD
Diplomate, International Congress of Oral Implantologists