Oral Disease: The Battle for Balance
Employing a whole-patient approach to the lifelong struggle of caries management
My teeth have always been soft.” That’s a statement that you have probably heard many times in your dental practice. Do these patients really have soft teeth? No, of course not. But patients have learned this response and thought process because it is how we in the dental profession have explained the unchecked ravages of tooth decay. This was one of the “easy” ways to explain to them why they, and we, could not help control the disease process. Today, dental research has given us a better understanding of the carious process and what mechanisms we should consider in its management.
Demineralization and Remineralization
First, the oral cavity is a biologic soup and our teeth “live” in this dynamic environment (Figure 1). The dentition and the oral bacteria are entwined in a cyclic reaction of demineralization and remineralization.1 With each food or drink item that passes through the mouth, the oral pH becomes acidic and the tooth structure demineralizes (Figure 2 and Figure 3). If not for saliva and its special properties, the teeth would simply dissolve away under a constant acidic attack. We also know that the enamel is a “semipermeable membrane”2 with a constant flow of fluids outward from the pulp chamber, which can also help protect the tooth structure. As the oral bacteria on the surface of the enamel surface continually reduce the pH of the outer surface of the enamel with the constant infusion of hydrogen ions, there is a resulting leaching out of calcium and phosphate ions from this structure, creating demineralization of the tooth structure. It is also understood that in the ideal mouth the indigenous microflora protect the host from exogenous pathogens by stimulating vigorous immune response and providing colonization resistance in a mutualistic symbiosis.3
Yet, most of the patients who we treat do not have “ideal” mouths. They present to us in conditions that are often significantly less than that. They present with disease (Figure 4 and Figure 5). It is the author’s opinion that it is our professional responsibility to help move our patients from a state of constant disease potential to a state of health. This requires much more than telling our patients that they must brush and floss more or better. The physical removal of the bacteria-laden plaque is of course important, but most of our patients are not fully “trained” on how to really do this well. Perhaps this is because we assume that they intrinsically know how. But the reality is that most of our patients do not fully understand how to remove this biofilm. They often rely on over-the-counter chemical agents and quick fixes that they find on the shelves of their supermarkets and pharmacies that promise to solve their dental issues but are often only superficial remedies.
It is incumbent upon us, the oral health care providers, to teach our patients how to effectively remove the biofilm that accumulates after each meal. When patients are instructed how to individually and properly manage their home care needs, major breakthroughs happen and improvement of the patient’s oral health occurs.
Understanding Caries Factors
Dental caries is the result of the activity of mutans streptococci (MS) and Lactobacillus.4 These microorganisms and others activate and contribute to the localized chemical dissolution of the dental structure. This term is used to describe the results, signs, and symptoms caused by the metabolic events taking place in the biofilms (dental plaque) that cover the affected areas in the oral cavity.5 This explains why one area of the mouth can have aggressive disease with not much activity in another area. Additionally, we must remember that caries has been defined as infectious and transmissible,6 resulting from the passing of the MS bacteria present in the oral cavity. This transmission can be vertical (parent to child) or horizontal (anyone to anyone). The dental sciences have been attempting to explain the caries model to the profession, and these models have evolved and changed over the years as our understanding of caries factors has grown.
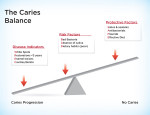
Perhaps the most important model that has been developed is the Featherstone Caries Etiology model (2007).7 This model (Figure 6) illustrates that disease control is dependent on a delicate balance between the protective commensals of the oral cavity and the risk factors present in the patient. This teeter-totter model simply explains that if there is an imbalance in the system that enables risk factors to outweigh protective factors, disease is the final outcome. If these risk factors are long term, then the caries process can and will run rampant and eventually destroy the dentition (Figure 7 and Figure 8). A Caries Sequence Model (Figure 9) has been adapted by Brian Nový, DDS, assistant professor of Restorative Dentistry at Loma Linda University. In this model, Nový states that low intraoral pH is the main ingredient in the overall sequence, confirming the adage, “If you don’t address the pH problem, you cannot control the disease.”
We know that saliva plays a significant role in maintaining good oral health. Healthy saliva contains proline-rich proteins and glycoproteins, mucins, calcium, and phosphates, along with trace amounts of fluoride and other minerals. It buffers the acids from plaque and acidic conditions when stimulated because the stimulated saliva pH will increase to 7.8 from a resting pH of 6.75. This action helps the healthy oral cavity recover from acute acidic episodes and helps in the “demin-remin” cycle, which occurs when the pH drops below 5.5 during normal eating and drinking. At this level, small amounts of tooth structure will dissolve and become trapped in the biofilm on the tooth’s surface. As the pH recovers, the demineralized structure can remineralize using these dissolved minerals.
However, when there is an imbalance in the oral system, this process often will not occur and dissolution of tooth structure will ensue. This is often seen with root caries, which occurs at a higher pH (6.2 to 6.4) than enamel caries (5.5). Additionally, the root surface has only half as much mineral as enamel, and is thus less defensive.
Patients with “dry mouth” are especially susceptible to root caries. Dry mouth can be caused by physiology or medications. Medically-induced xerostomia disease is increasingly being identified as a significant problem for patients.8
Assessing the Factors
The challenge for the dental care provider is determining how to manage the caries disease process. Embracing Caries Management by Risk Assessment (CAMBRA) is an important step in the management process of the caries infection. First, identification of the disease indicators is imperative. The identification process includes understanding the socioeconomic status of the patient, identifying any development problems, observing the presence of white spot lesions, and noting the placement of restorations in the previous 3 years.
Next, the clinician must identify risk factors, such as an acidic oral environment and dry mouth. Knowledge of the type and quantity of bacteria, along with the presence of visible plaque, exposed roots, saliva reduction factors, inadequate saliva flow, frequent snacking habits, deep pits and fissures, and orthodontic appliances must also be considered in this assessment. Some of those indictors and risk factors have been discussed above. The clinician then needs to introduce caries protective factors.
Options for Preventive Care
There are many different treatment modalities that the dental care provider can call upon to help achieve balance in the oral cavity. Fluoride products and treatments are certainly one line of defense, but there are others that should be considered.
Chlorhexidine gluconate (0.12%) solution is a cationic detergent that contains positively charged ions that are attracted to the negatively charged cell walls of MS. This disrupts adhesion, cell membrane function, the uptake of glucose, the production of glucans, and bacterial metabolism. Patient compliance often becomes an issue, however, because of the staining of the patient’s teeth. Additionally, chlorhexidine cannot be combined with fluoride, and it does not have a significant effect on Lactobacillus.
Nutraceutical phenols, such as Herbal Lollipops (Dr. John’s® Candies, www.drjohns.com), contain a specific herbal formula extracted from licorice root that has been shown to selectively kill gram-positive cariogenic coaggregates, gram-negative periodontal coaggregates, and all oral yeasts.9 The nutraceutical phenol also slows biofilm formation, does not harm protective commensals, and has a consistent activity.
A sodium hypochlorite 0.2% oral rinse such as CariFree® (Oral BioTech, www.carifree.com) is bactericidal to all bacteria on contact. Used as part of the CariFree system, it allows dental care providers the ability to diagnose and treat the caries infection with minimally invasive procedures. The intent of this unique system is to assist in regulating oral pH in addition to strengthening the dentition through the combination of the sodium hypochlorite solution, xylitol, and fluoride in its various components. Limitations of the system include the possible side effect of a change in taste sensation, and the recommendation for use only in patients 6 years and older.10
Probiotic dental therapy is defined as the daily administration of certain live microorganisms in amounts adequate to confer a health benefit to the host.11 The ProBiora3® system of products (Oragenics, www.oragenics.com) replenishes the mouth’s healthy bacteria by crowding out harmful bacteria using a patented blend of three beneficial bacteria naturally present in healthy mouths.12 This blend of probiotics helps promote fresher breath and supports periodontal and dental health. There is an added beneficial side effect, which is the release of a low-level form of hydrogen peroxide as a normal by-product, which will whiten the patient’s teeth. EvoraPro® is available for professional dispensing to accelerate the repopulation of beneficial bacteria.
When sodium bicarbonate (baking soda) is used as an oral dentifrice, it is an effective mechanism to help prevent the resurgence of disease-causing bacteria. It has low abrasion to the tooth structure, is antibacterial, and helps create a large pH shift to neutralize even the most acidic oral environment. The taste challenge initially experienced by the patient is often overcome with time and use, and many patients report that they like how their teeth feel after using it.
Xylitol is a five-carbon alcohol sugar that cannot be metabolized into acid by cariogenic bacteria. Because it cannot be metabolized, it helps reduce the population of cariogenic bacteria. Its sweet taste can also increase saliva flow and help increase tooth remineralization. Chewing gums and hard candies containing xylitol used after each meal in children older than 5 years have been shown to be a very effective by the multidisciplinary expert panel convened by the American Dental Association (ADA) Council on Scientific Affairs. It is recommended that patients at high risk for caries use 6 to 10 g of xylitol per day. Additionally, when combined with sodium fluoride, it can provide improved anticaries benefits.13 Products such as Salese™ (Nuvora®, Inc., www.nuvorainc.com), an over-the-counter xylitol and baking soda lozenge, have been very helpful when used as directed to help prevent oral pH from falling to critical levels. XyliMelts® (OralHealth, www.oralhealth.com) are a recent addition to the prevention market. These are self-adhesive discs that release xylitol via a time-release mechanism. The disc is applied to the buccal mucosa and allowed to dissolve over time to help neutralize the pH of the oral cavity.
This same multidisciplinary ADA panel concluded that a mixture of chlorhexidine-thymol varnish should be used as a root caries preventive agent. Cervitec® Plus (Ivoclar Vivadent, www.ivoclarvivadent.com) is a 1% chlorhexidine and 1% thymol varnish that firmly adheres to tooth surfaces and creates a shield of long-lasting protection. White lesions should have Cervitec Plus applied followed by a fluoride varnish such as Embrace™ Varnish (Pulpdent Corporation, www.pulpdent.com) 1 to 2 weeks later. Embrace Varnish has a unique combination of xylitol, calcium, phosphate, and fluoride and can significantly help remineralize tooth surfaces.
MI Paste™ and MI Paste Plus™ (GC America Inc., www.gcamerica.com), which contain RECALDENT™, help to strengthen teeth by replenishing calcium and phosphates, the needed building blocks of tooth structure. These products help produce a salivalike environment that aids in maintaining normal acid levels in the oral cavity. It has also been shown to inhibit the attachment of MS and attract “good” bacteria, thus helping to change the biofilm in the mouth.
Conclusion
The effort to restore and maintain balance in the oral cavity is a lifelong struggle. This understanding is causing a paradigm shift in the overall thought process of the dental profession; moving dentists from a repair and restore modality, to one of identification, prevention, and maintenance. As clinicians become more aware of this process, we can learn to help our patients defend against oral imbalance. Our patients’ health and well being depend on it.
References
1. Featherstone JD. The caries balance: the basis for caries management by risk assessment . Oral Health Prev Dent. 2004;2(3):259-264.
2. Chow LC, Vogal GL. Enhancing remineralization . Oper Dent. 2001;26(suppl 6):S27-S38.
3. Ruby J, Barbeau J. The buccale puzzle: The symbiotic nature of endogenous infections of the oral cavity . Can J Infect Dis. 2002;13(1):34-41.
4. van Houte J. Role of micro-organisms in caries etiology . J Dent Res. 1994;73(3):672-681.
5. Fejerskov O, Kidd EAM . Dental Caries: The Disease and its Clinical Management. 2nd ed. Oxford, England: Blackwell Publishing; 2008.
6. Caulfield PW, Li Y, Dansanayke A. Dental caries: an infectious and transmissible disease . Compend Contin Educ Dent. 2005;26(5)(suppl 1):S10-S16.
7. Featherstone JD, Domejean-Orliaguet S, Jenson L, et al. Caries risk assessment in practice for age 6 through adult . CDA Journal. 2007;35(10):703-712.
8. Sreebny LM, Vissink A. Dry Mouth, the Malevolent Symptom. Hoboken, NJ: Wiley-Blackwell; 2010.
9. Peters MC, Tallman JA, Braun TM, Jacobson JJ. Clinical reduction of S. mutans in pre-school children using a novel liquorice root extract lollipop: a pilot study . Eur Archs Paediatr Dent. 2010;11(6):274-278.
10. Kutch VK, Bowers RJ. Balance. A Guide for Managing Dental Caries for Patients and Practitioners. Tamarac, FL: Llumina Press; 2012.
11. Socransky SS, Hafajee AD. The bacterial etiology of destructive periodontal disease: current concepts . J Periodontal. 1992;63(4 Suppl):322-331.
12. Hillman JD, McDonell E, Cramm T, et al. A spontaneous lactate dehydrogenase deficient mutant of Streptococcus rattus for use as a probiotic in the prevention of dental caries . J Applied Microbiol. 2009;107(5):1551-1558.
13. Sintes IL, Escalante C, Stewart B, et al. Enhanced anticaries efficacy of a 0.243% sodium fluoride/10% xylitol/ silica dentifrice: 3 year clinical results . Am J Dent. 1995;8(5):231-235.
John C. Comisi, DDS, MAGD
Private Practice
Ithaca, New York