Nano-Ceramic Restorative Block
A new material is available for chairside CAD/CAM restorations.
By Dennis J. Fasbinder, DDS
Monolithic restorative materials can offer innovative restorative solutions for age-old dental problems. Chairside CAD/CAM systems are commonly associated with the use of adhesive ceramic materials to fabricate inlays, onlays, crowns, and veneers. A number of feldspathic porcelain (eg, Vita® Mark II, Vident, www.vident.com; CEREC® Bloc, Sirona Dental Systems, www.sirona.com), leucite-reinforced porcelain (IPS Empress® CAD, Ivoclar Vivadent, www.ivoclarvivadent.com), and lithium-disilicate (IPS e.max®, Ivoclar Vivadent) blocks are available for use with the CEREC® AC (Sirona) and E4D Dentist (D4D Technologies, www.e4d.com) systems.1 Several long-term clinical studies have documented the longevity, durability, and clinical success of these types of restorations.2 Composite resin (Paradigm™ MZ100, 3M ESPE, www.3mespe.com) blocks are also available for both chairside systems. Although the composite block has been available for over 10 years, it does not have the same clinical acceptance as the porcelain blocks. One of the primary reasons for the lack of clinical use of the composite block is the general perception dentists have of “composite” materials.
Composite Material Use
A composite material is generally defined as something composed of more than one distinct element or compound. While most materials in dentistry fit under this broad definition of a composite material, in dentistry, the term “composite” specifically refers to the tooth-colored restorative material composed of a resin matrix and various types of filler particles, which is used in a myriad of formulations for the direct restoration of teeth. Dentists are well aware that composites shrink in volume by 1.5% to 3% when they are cured. This polymerization shrinkage is purported to lead to enamel microfractures, margin gaps, microleakage, marginal staining, and recurrent caries, which can result in restoration failures. Considerable effort has been devoted to understanding this undesirable process and limiting its effects.3 The application of multiple, discrete layers of composite that are sequentially cured is the accepted clinical technique to control potential damage to the composite restoration or tooth structure due to the stress generated by polymerization shrinkage.
Creating well-contoured proximal surfaces and firm contacts with adjacent teeth can also be problematic in posterior composite restorations. A number of sectional matrix designs and clinical techniques have been advocated for use with composites to create the desired proximal contours and contacts.4 Composites also are thought to endure more general surface wear in larger occlusal posterior restorations. They are generally not considered to be the optimal material for developing and maintaining stable occlusal contacts over the long term and are often placed initially with the expectation that they will become core foundations for future indirect-metal or ceramic restorations.
Chairside CAD/CAM Restorations
Composite Materials
Chairside CAD/CAM restorations offer an alternative solution to the placement issues involved with the use of direct composite materials while still completing the restoration in a single appointment. A randomized clinical trial compared the clinical longevity of composite (Paradigm MZ100) inlays to porcelain (Vita Mark II) inlays.5 At the end of 10 years of clinical function, there was no significant difference in margin finish, surface finish, proximal contact, and anatomic form, which was found to remain essentially unchanged from baseline for both materials. Six porcelain inlays fractured over the course of the study; only one was a fracture of a composite inlay. Chairside CAD/CAM composite inlays performed as well as porcelain inlays, with significant advantages in shade match and inlay fracture over the 10 years of the study.
Nano-Ceramic Restorative Block
A recently developed nano-ceramic restorative material is a unique CAD/CAM block based on the integration of nanotechnology and ceramics. The material is said to offer the ease of handling of a composite material with a surface gloss and finish retention similar to a porcelain material. Lava Ultimate™ (3M ESPE) contains a blend of nano-particles agglomerated to clusters and individual bonded nano-particles embedded in a highly cross-linked polymer matrix. It is a combination of aggregated zirconia/silica clusters (composed of 20-µm silica and 4-µm to 11-µm zirconia particles), non-agglomerated/non-aggregated 20-µm silica, and non-agglomerated/non-aggregated 4-µm to 11-µm zirconia with an approximately 80% ceramic load.
The fracture resistance of a material is a function of fracture toughness and flexural strength. With a reported flexural strength of 200 MPa, the nano-ceramic block has a higher initial strength than feldspathic and leucite-reinforced porcelain blocks, as well as veneering porcelains for porcelain-fused-to-metal crowns. The improved strength allows for a somewhat more conservative tooth reduction in the cavity preparation. The manufacturer recommends an axial reduction of 1 mm and a cuspal reduction of 1.5 mm, with both dimensions being about 0.5 mm less than that conventionally recommended for porcelain restorations. The fracture toughness of the nano-ceramic material is statistically greater than feldspathic materials and direct composites, while being less brittle than feldspathic glass-ceramics and, therefore, less prone to cracking during try-in and function. A laboratory study reported that adhesively bonded Paradigm MZ100 molar crowns were more crack-resistant than adhesively bonded Vita Mark II porcelain crowns.6
The inclusion of nano-particles in the Lava Ultimate block offers the potential for easy adjustment and creation of a high-gloss surface finish similar to porcelain. A reported advantage of the nano-ceramic material is its ability to retain a high-gloss surface finish over time, which is a limitation of composite blocks. In vitro studies by the manufacturer indicate that Lava Ultimate has a resistance to toothbrush abrasion and retention of the initial glossy surface finish similar to glass ceramics. However, only long-term clinical evaluation will confirm this desirable property of the material. Lava Ultimate restorative will be available in eight popular shades in both low- and high-translucency forms for both CEREC AC and E4D chairside CAD/CAM systems. In addition, the manufacturer will offer a 10-year warranty for replacement of the restorative material should it fail clinically.
Case Report
A patient presented with a long-standing direct composite restoration with significant wear at the facial and occlusal areas (Figure 1 and Figure 2). After discussing treatment options, risks, and benefits, the patient elected to have a chairside CAD/CAM onlay delivered in a single appointment.
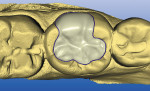
After local anesthesia was administered, the cavity was prepared for the nano-ceramic onlay, which was more conservative than for CAD/CAM ceramic onlays, with 1.5-mm reduction over the cusps and 1-mm axial reduction to ensure adequate restorative material to resist fracture. The proximal contacts of the tooth were maintained intact, as the marginal ridge areas were well supported by dentin and the proximal surfaces were free of caries (Figure 3).
Digital scans of the preparation quadrant and opposing teeth were made with the CEREC AC system, and the virtual models were aligned with a buccal scan. The preparation details were easily visualized on the virtual model in the design software (Figure 4). The restoration proposal was calculated based on the unique anatomy of the adjacent teeth, refined with the CEREC 3D V3.84 software program (Sirona) and transmitted to the milling chamber (Figure 5). A Lava Ultimate I14 block (shade A2 LT) was inserted into the milling chamber, and the onlay was milled from the prefabricated block of nano-ceramic (Figure 6). Upon recovery of the milled restoration from the milling chamber, the restoration was tried in and adjusted for optimum internal adaptation and marginal fit to the cavity preparation.
The restoration was efficiently polished with a low-speed, single-grit, abrasive polisher (40-µm aluminum oxide-impregnated silicon) followed by polishing with a Robinson bristle brush with a 5-µm diamond polishing paste. The onlay was made ready for delivery by air-abrading the intaglio surface of the restoration. (It is not recommended to etch the intaglio bonding surface with hydrofluoric acid.) A selective etch concept with a dual-cure resin cement was used to adhesively cement the restoration. Following visible-light curing, the margins were finished and polished with a 15-µm microfine-diamond, low-speed, single-grit abrasive polisher (40-µm aluminum oxide-impregnated silicon), followed by polishing with a latch-head brush with impregnated abrasive silicon-carbide particles and a 5-µm diamond polishing paste (Figure 7 and Figure 8).
Conclusion
This clinical case illustrates the high-gloss finish that can easily be achieved with the nano-ceramic material with a very efficient finishing and polishing sequence without the need for firing the restoration in a porcelain furnace. The clinical use of the nano-ceramic material will ultimately be determined by long-term clinical research. Previous studies of chairside CAD/CAM composite restorations have documented the durability and fracture resistance of the material as well as its wear resistance compared to feldspathic porcelain.5 The degree to which the new nano-ceramic material duplicates these features with a more conservative tooth reduction and improved retention of the surface finish and gloss will ultimately determine the expanded use of the material. The nano-ceramic CAD/CAM block Lava Ultimate will surely challenge the thoughtful provider to reconsider the misperception that this is “just another block.”
References
1. Fasbinder, DJ. Restorative materials for chairside CAD/CAM restorations. Compend Cont Educ Dent. 2010;31(9):2-17.
2. Fasbinder DJ. Clinical performance of chairside CAD/CAM restorations. J Am Dent Assoc. 2006;137(Suppl):22S-31S.
3. Tantbirojn D, Pfeifer CS, Braga RR, Versluis A. Do low-shrink composites reduce polymerization shrinkage effects? J Dent Res. 2011;90(5):596-601.
4. Saber MH, El-Badrawy W, Loomans BA, et al. Creating tight proximal contacts for MOD resin composite restorations. Oper Dent. 2011;36(3):304-310.
5. Fasbinder DJ, Dennison JB, Heys D. Clinical Evaluation of CAD/CAM-Generated Composite Inlays: Ten-Year Report [abstract]. International Association of Dental Research. 2011;Abstract #379.
6. Kassem AS, Atta O, El-Mowafy O. Combined effects of thermocycling and load-cycling on microleakage of computer-aided design/computer-assisted manufacture molar crowns. Int J Prosthodont. 2011;24(4):376-378.
About the Author
Dennis J. Fasbinder, DDS
Clinical Professor
University of Michigan School of Dentistry
Ann Arbor, Michigan