Facial Esthetics—The Framework
Using facial landmarks to dictate tooth position can enhance esthetics and conserve tooth structure.
By Michael Apa, DDS
In order to create individual smiles that compliment patients’ facial features and enhance their overall facial beauty, clinicians can adopt a technique that uses facial landmarks to dictate tooth position. This method not only can enhance the esthetics, it can also ultimately allow the practitioner to be more conservative in tooth reduction.
Where Symmetry Comes In
To understand this type of procedure, it helps to have a general understanding of the word “beauty,” which is defined as the phenomenon of the experience of pleasure through perception of balance and proportion of stimulus. In short, something is perceived as beautiful when some type of harmony or balance exists. During the last decade of cosmetic dentistry, “smile design” has focused mainly on modifying the position and restoring the teeth of patients seeking a better-looking smile.1 This approach became the foundation for laboratories and practitioners communicating in the design process. It also resulted in perfectly symmetrical smiles’ being duplicated for each individual patient. However, if carefully analyzed, it is apparent that patients’ faces are not symmetrical,2 and that delivering or creating complete symmetry in an asymmetrical environment creates a disharmony that can be easily visualized. Therefore, it is of utmost importance to analyze the facial features or “the frame” in which the smile is being created. Within this process, the objective is to design the smile creating symmetry with features and, in a sense, tying the features of the face together by balancing them with the smile.
The challenge for educators in this situation is teaching something that is abstract in a clinical, methodical way. It is important to understand that esthetic dentistry combines both an artistic component along with a comprehensive dental approach.
Finding the Frame
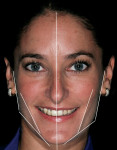
The first instinct of practicing clinicians is to see the smile. The first exercise in these types of cases is to back up and see the progression of development that has occurred. The idea is to find the frame within which the smile belongs, then focus on parameters of smile design, and finalize by looking at individual tooth form.3 The parameters guiding the facial analysis are the horizontal plane, vertical plane, the relation of thirds of the face, and the strong side versus the weak side (Figure 1). These elements provide the frontal framework of the smile. In essence, the clinician should be able to visualize the proper incisal plane that the gingival plane should be paralleled to, the axial inclinations, the position of the teeth in the lower third of the face, and the angulation of the buccal corridor. Upper lip support, lower lip relation, and the occlusal plane all influence sagittal reference, and two characteristics of the smile that are best visualized in the sagittal dimension are overjet and incisor angulation. Finally, the clinician should focus on the oblique plane, which provides reference to the smile arc and orientation of the palatal plane.4 Diagnostically, the practitioner should consider the three-dimensional position of the smile, then use a knowledge of smile design and tooth proportion to finish creating natural esthetics.
Reference Points
Clinicians should orient themselves with a vertical and horizontal plane of reference. Those who have painted, sculpted, or sketched are aware of the need for perspective in space. This is referred to as the “Facial T” (Figure 2). Attractiveness results from a general sense of parallelism and symmetry between structural facial features, because parallelism is the most harmonious relationship between two lines.5 The interpupillary line represents the horizontal perspective that guides evaluation of the incisal plane, gingival margins, and the position of the maxilla (Figure 3, Figure 4, Figure 5). It should be noted that the interpupillary line is not always the only reference that can be used, because there are situations in which patients may have an asymmetrical position of the eyes. In this case, a second reference, which is perpendicular to the facial midline, can be used.6 The vertical element is the facial midline bisecting the center of the face and extending through the bridge (nasion) of the nose and philtrum. This midline becomes reinforced by the direction and axis of the dental midline. If the dental midline cannot be coincident with the facial midline, it is best to anchor the smile by creating the midline vertical. Severe discrepancies may indicate orthodontic movement (up to 2 mm off the facial midline).7,8 The facial midline aids in evaluating the location and axis of the dental midline along with mediolateral discrepancies in tooth position.
Next, the clinician should consider the growth and development of the patient to determine how to treat the anterior esthetics. The upper third of the face is the area bordered by the base of the hairline—or beginning of wrinkling of the forehead—to the top of the brow. The top of the brow to the base of the nose is the middle third, and the base of the nose to the base of the chin is considered the lower third. This evaluation will reveal any abnormalities in anterior facial height (Figure 6). As ramus length varies, both anterior facial height and tooth display vary. Not only can this determine the need for periodontal surgery or orthodontic movement, it also defines the buccal parameters of the buccal corridor. A short ramus with normal posterior eruption results in an obtuse gonial angle, or the “long, narrow face.” The patient may develop either an anterior open bite, which would indicate a combination of orthodontics and or prosthetics, or excessive gingival display, which would indicate maxillofacial surgery or hard-tissue crown lengthening and prosthetics. Conversely, decreased anterior facial height is due to a long ramus, an acute gonial angle, and results in inadequate maxillary tooth display and a “square face.” This can be treated orthodontically or restoratively. Again, these are generalizations, and each case has its own set of parameters. What is important to remember is that people’s faces are not symmetrical from right to left. The gonial angles are influenced by the strength of the masseter muscle—the stronger the masseter muscle (strong side), the more acute the gonial angle. From a frontal view, this creates an angle that should parallel the canine, premolars, and molars—which comprise the buccal corridor. Starting from the condyle to the pogonion, the canine and buccal corridor should parallel this angle in order for the teeth to “frame” the face. If the incisal tips of the canines or premolars are hanging over the lower lip, it means the teeth have been built out too far buccally; conversely, if there is too much negative space, the smile has not been built out enough. An important point, however, is to understand what building the smile out does to a patient’s face: It essentially widens, or gives horizontal prospective to, the lower third of the face. Women who have lost sufficient cheek fat can have a “smile lift,” which, in essence, gives the illusion of fuller cheeks. Understanding what the buccal corridor does is very powerful in creating the desired look.
In determining the guidelines from a sagittal reference, there are three factors to consider: upper lip support, lower lip relation, and the occlusal plane. Upper lip support is determined by the gingival two thirds of the maxillary central incisors. This is important in understanding the necessary changes to be made to the upper lip, if any. Lip incompetence is caused when the centrals are tipped too far facially; conversely, when the teeth are retruded, the upper lip falls over the teeth and becomes thin at the vermillion border. The second thing to note is where the incisal third of the maxillary centrals will lie; they should be just short of the wet-dry border of the lower lip. Finally, the occlusal and incisal edges of the occlusal plane should coincide with the Camper’s plane, which extends from the inferior border of the ala of the nose to the superior border of the tragus of the ear.
Once clinicians have established a three-dimensional framework, they can begin applying these principles to determine how to restore the patient’s smile.
Case Presentation
Patient Evaluation
A 29-year-old woman who had had an implant placed previously in the No. 7 site discussed her desire for overall improvement in her smile. After analysis of her face, it was determined that it was fairly symmetrical (mesofacial).9 The left gonial angle was lower than the right, making the patient’s left side the “strong side,” and the right the “weak side” (Figure 7). Upon radiographic examination, a large Class III composite restoration was seen between the anterior teeth mesially and distally. Clinical examination revealed a resin-bonded fixed partial denture (FPD) over the implant in site No. 7, bonding on tooth No. 10, and mild wear on the canines.
Treatment Plan and Preparation
The treatment plan recommended to the patient was to restore teeth Nos. 4 through 6 and teeth Nos. 8 through 13 with porcelain laminate veneers and site No. 7 with an implant-supported porcelain-fused-to-metal (PFM) crown.
The clinicians located the midline by finding the patient’s facial midline and relating it to her dentition. Next, they identified the interpupillary plane and related the gingival and incisal planes to it (Figure 3, Figure 4, Figure 5). They continued to find all of the facial parameters noted above until the framework for the smile was found. Once this was achieved, they moved into performing the dental analysis. In this particular patient, the desirable “golden proportion” seemed to be significantly off in the anterior central and lateral incisors, while the canines and premolars seemed to need minimal adjustment.10,11 To address the soft-tissue heights, which were also quite irregular, the clinicians planned to achieve gingival harmony through manipulation with a diode laser (Figure 8 and Figure 9).12,13 To establish the implant contact point, they needed to measure to the crest of bone from the mesial and distal—4.5 mm to 5 mm from the crest of bone to the contact point is needed to re-establish papillary growth.14,15 Note that prior to beginning any case, this exact “mental” diagnosis is performed to determine tooth position. The authors then prefer to mark up the mouth to do a quick mock-up in flowable composite (LuxaFlow™, Zenith/DMG, www.dmg-america.com) to achieve final shape. This is done prior to anesthesia, and it provides the practitioner with an accurate idea of what can be achieved; it can also be used as a preparation guide for proper reduction (Figure 10 and Figure 11).16
The most important factor with a mock-up is to follow smile design as a guide, but be able to see where the facial planes play a role in tooth position. The first step is to get the central incisor position vertical and centered with the facial midline. By altering line angles in teeth, it is possible to change the axial inclination, altering both gingival zenith and axial inclination. Incisal length and facial-lingual position are evaluated to determine if adjustments are needed. The laterals, in this case, were used to offset the centrals to create natural embrasure. Tooth No. 7 was rotated in a mesial-lingual direction to create a natural embrasure as well as raise the contact point to a more apical position for papillary regeneration. Tooth No. 10 was set back slightly to the lingual, again, simply to create a natural esthetic appearance. The canines and premolars were mocked up to parallel the planes of the strong and weak sides. Once the clinicians were satisfied, an alginate impression, which would serve as a provisional stent, was taken.
The teeth were then prepared using the mock-up as a guide for reduction. The clinicians used a feldspathic ceramic, which can be feathered to approximately 0.2 mm. This demonstrates that bulk reduction for material is not always the important issue. It is rather an understanding of initial tooth position and desired tooth position, along with stump shade and desired shade, which dictates preparation. Some controversy may exist as to the minimum thickness of porcelain laminate veneers.17 Studies have shown that a minimum thickness of 0.2 mm is needed for each shade change.18 As always, initial arch form preparation was done first, followed by soft-tissue recontouring (Figure 12, Figure 13, Figure 14), and, finally, final margin placement.19 Once these steps were completed, the provisional material (bis-acryl) was placed into the alginate stent and allowed to partially set for 1 minute. It is important to note that a thin layer of glycerin must be placed on the teeth first to inhibit polymerization. The provisionals can be pulled from the mouth and evaluated for thickness of material to see if the proper amount of reduction has been accomplished. After verification, final impression, and an accurate bite registration, the preparation shade and facebow were taken. The provisionals were then trimmed and temporarily bonded in place using the “spot-etch technique” and flowable resin (Figure 15 and Figure 16).20
The patient is always brought back the following day to go over the provisionals to check the occlusion and esthetics. In this case, minor adjustments were made and records were then completed to relay to the laboratory. Final measurements of the central incisors were taken, as were a full digital set of photographs, alginate impressions of the temporaries, and a bite registration. The goal is to provide as much information to the ceramist as possible to make it easier to replicate the shape, contour, and detail of the temporaries in the ceramic. The authors have found that a proper set of provisionals can eliminate a lot of the guesswork in communication between patient, doctor, and ceramist. While the shape of the smile three-dimensionally is a major factor in creating natural smiles, it is also important to consider color and texture. Some may say that this is the job of the ceramist, but it is crucial to be able to guide the ceramist in relaying the correct color and texture. Understanding the medium being used and having a sense of the spatial arrangement of the face guides the proper positioning of the smile.
To complete this case, the restoration was then inserted and the tissue around the implant was given 2 months to heal properly before any adjustments were made. Minor occlusal adjustments and nightguard therapy were performed to ensure longevity of the restorations (Figure 17, Figure 18, Figure 19, Figure 20).
Conclusion
Following simple principles regarding the special arrangement of the face can guide the clinician in providing more natural smiles with less tooth reduction. The authors have found that offering this type of treatment requires that practitioners educate their patients in color and form. While patients may be initially resistant to “imperfect perfection,” when executed properly, it provides the ability to mimic nature. The end result is a proper reduction rather than over-reduction, and a smile that looks like the one the patient was born with.
Acknowledgments
Dr. Apa would like to thank Jason Kim, CDT, of Oral Design for the ceramic work in this case, and Albert Ambriz, DDS, for his research assistance on this article.
References
1. Calamia JR, Ciseros G, Levine JB, et al. Smile design and treatment planning with the help of a comprehensive esthetic evaluation form. Dent Clin of North Am. 2011;55(2):187-209.
2. Ferrario VF, Sforza C, Poggio CE, Tartaglia G. Distance from symmetry: a three-dimensional evaluation of facial asymmetry. J Oral Maxillofac Surg. 1994;52(11):1126-1132.
3. Winter R. Visualizing the natural dentition. J Esthet Dent. 1993;5(3):102-117.
4. Sarver DM, Ackerman MB. Dynamic smile visualization and quantification: Part 2. Smile analysis and treatment strategies. Am J Orthod Dentofacial Orthop. 2003;124(2):116-127.
5. Chiche GJ, Pinault A. Esthetics of Anterior Fixed Prosthodontics. 1st ed. Chicago, Illinois: Quintessence Publishing. Co.; 1994.
6. Morley J, Eurank J. Macroesthetic elements of smile design. J Am Dent Assoc. 2001;131(1):39-45.
7. Kiyak HA, Kokich VO Jr, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11(6):311-324.
8. Spear FM, Kokich VG, Matthews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137(2):160-169.
9. Jefferson Y. Skeletal types: Key to unraveling the mystery of facial beauty and its biologic significance. J Gen Orthod. 1996;7(2)7-25.
10. Levin EI. Dental esthetics and the golden proportion. J Prosthet Dent. 1978;40(3); 244-252.
11. Preston JD. The golden proportion revisited. J Esthet Dent. 1993;5(6):247-251.
12. Lee EA. Laser-assisted gingival tissue procedures in esthetic dentistry. Pract Proced Aesthet Dent. 2006;18(9):2-6.
13. Lee EA. Laser-assisted crown lengthening procedures in the esthetic zone: contemporary guidelines and techniques. Contemporary Esthetics and Restorative Practice. 2006;42-49.
14. Chu SJ, Tan JH, Tarnow DP, Stappert CF. Papilla proportions in the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2009;29(4):385-393.
15. Fletcher P, Magner AW, Tarnow DP. The effect of the distance from the contact point to the crest of bone one the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
16. Gurel G. predictable and precise tooth preparation techniques for PLVs in complex cases. Oral Health. 2007;15-26.
17. Radz GM. Minimum thickness anterior porcelain restorations. Dent Clin North Am. 2011;55(2):353-370.
18. McLaren EA. Porcelain veneer preparations: to prep or not to prep. Inside Dentistry. 2006;2(4):76-79.
19. Spear FM. Treatment planning materials, tooth reduction, and margin placement for anterior indirect esthetic restorations. Advanced Esthetic and Interdisciplinary Dentistry. 2005;1:4-14.
20. Alex G, Boksman L, Margeas RC. Provisionals: alternative methodologies. Dentaltown.com. 2006;October:52-59.
About the Author
Michael Apa, DDS
Private Practice
New York, New York