Periodontal Disease: Conservative Management
Neil R. Gottehrer, DDS
The consumer is becoming more aware of periodontal disease, with data now published suggesting that periodontal infections can influence certain systemic diseases such as cardiovascular disease. These medical studies1,2 have been featured in the media. As a result, the challenge for the dentist to provide conservative, nonsurgical management of this disease has been decreased with increased consumer knowledge of the disease and desire to maintain their health.
With estimates as high as 60 million people suffering from periodontal disease, there is a significant percentage of the adult population needing conservative care for this condition.3 In May 2000, Dr. David Satcher, MD, PhD, then the US Surgeon General, reported that periodontal disease was one of the most prevalent diseases in the United States, second only to heart disease.4 It has been documented to be the number one cause of tooth loss.5 Patients must realize that they cannot maintain a healthy periodontal condition and retain their teeth without regular periodontal care and proper oral hygiene.6
Treatment now must focus on etiology, potential sequelae, and longer-term ramifications of untreated disease. Objectives of conservative periodontal treatment should include altering or eliminating microbial etiology and the contributing factors for periodontal disease, halting disease progression and returning the dentition to a state of health and comfort,7 obtaining host healing, and achieving gains in clinical attachment levels. New approaches to treatment, such as the recent advances in the use of site-specific, local antibiotics8 and host modulation by enzyme suppression,9 have become available and can result in more patients accepting treatment with the potential for improved results from care.
Pathogenesis of Periodontal Disease
Gingivitis and periodontitis are plaque-related conditions initiated by the accumulation of biofilms, which are highly organized subgingival bacterial plaques, on the oral mucosa and tooth surfaces.10 Clinicians continue to use manual probing to evaluate pocket depth (Figure 1) and bleeding on probing as primary diagnostic indicators of disease activity, based on clinical studies done in the early 1990s. The study indicated that frequent bleeding on probing was a predictor of future clinical attachment loss.11
It has been suggested that an absence of bleeding on probing be used as a criterion for stability rather than using the presence of bleeding as a predictor of disease activity.12 Histologic evidence of an absence of an inflammatory cell infiltrate at sites where bleeding on probing is eliminated further supports the use of bleeding status over time as part of the decision-making process for treatment.13
Manual Mechanical Therapy
Once the decision has been made that disease is present, the removal of sub- and supragingival plaque and calculus is required to treat the disease. Although Kaldahl14 demonstrated that surgical debridement provided better access to calculus removal than conservative techniques nonsurgically, especially in molar furcation and deep pockets, newer approaches can offer patients alternative therapies, especially when periodontitis is in the early stages. Chronic adult inflammatory periodontal disease can be both site-specific and episodic, either active or refractory. At any given time, there can be healthy sites that display evidence of previous disease that are no longer active, sites at which tissue destruction is actively occurring, and sites that are experiencing repair. Therefore, the typical patient presents with sites requiring different levels of care. Some areas require active treatment while others can be successfully managed with a single preventive maintenance visit. Other areas may require more involved treatment, necessitating extended care with multiple visits. The major challenge for the dentist and hygienist is to provide the appropriate care for all of these areas.
At times it is a challenge to clearly view the root surfaces that require treatment. This is easier to accomplish with optical magnification using clinical loupes. Used often for endodontic and restorative treatment, the lenses make it easier to view the root surfaces being instrumented, and can be used by both the dentist and hygienist. The lenses supplement tactile sensation and can further improve clinical outcomes.
Hinrichs et al15 found that the effect of periodontal therapy is directly related to the ability of treatment to lower the levels and prevalence of the pathologic bacteria. They indicated that treatment of chronic periodontal disease using hand instrumentation for subgingival scaling is likely to result in a modest change in the bacterial composition.
Ultrasonic Mechanical Therapy
While complete removal of subgingival calculus is unlikely, and it is not necessary to remove cementum, Smart16 found that considerable root detoxification and gingival healing results from using multiple light strokes with either sonic or ultrasonic scaling. It was found by Thornton and Garnick,17 in comparing ultrasonic and hand instrumentation, in the removal of subgingival plaque, that treatment outcomes were superior with ultrasonic instrumentation, such as the Dentsply Cavitron® (DENTSPLY, York, PA).
The most recently developed power-driven scalers, the piezo-ultrasonics, such as the Hu-Friedy Symmetry IQ™ (HuFriedy, Chicago, IL; Figure 2), produce a lateral or two-dimensional tip movement that has been described by many clinicians as the most ergonomic. The device requires less water, and, therefore, less aerosol spray is created. Piezo-ultrasonics produce no magnetic field; therefore, they can be used with patients who have a pacemaker and may be sensitive to a magnetic field.18
Lindhe and Nyman19 found that to sustain the positive effects of periodontal treatment, scaling and root planing must be performed periodically during the maintenance phase of therapy. They found that effective supragingival control of microbial plaque is absolutely critical if the dentist and hygienist are to achieve long-term control of inflammatory periodontal disease.
While most patients are able to remove supragingival plaque with routine oral hygiene procedures using manual brushes, floss, and other aids, the development of the “power” toothbrush has made this procedure much easier for many patients, particularly those with special needs. A 6-week study of one power toothbrush, compared with a manual brush, focused on special needs and geriatric patients. Plaque reduction was found to be 38% with the power brush, and 6% with the manual brush.20 Because most patients have difficulty maintaining a plaque-free, healthy mouth over extended periods of time, use of these power toothbrushes can help to improve and maintain periodontal health.
The use of antibacterial toothpastes, eg, Colgate Total® (Colgate, New York, NY) and Crest® Pro-Health™ (Procter & Gamble, Cincinnati, OH), has been documented to show significant reduction in bacterial accumulation on the tooth for up to 12 hours.21 Therefore, these pastes should be used at least two times per day with power brushing. Since Cobb demonstrated that power water irrigators cleansed deep between the teeth and below the gingival margin to remove the bacteria associated with periodontal disease,22 the irrigator should be used immediately following the power brush to obtain optimal bacterial reduction. Use of an antibacterial mouthrinse, eg, Listerine® (McNeil-PPC, Inc., Skillman, NJ) or Crest® Pro-Health™, as the final stage of personal oral hygiene, can destroy the remaining exposed oral bacteria on contact, completing the temporary removal of the dental plaque.23
To increase the number of patients who proceed with treatment, education must focus on etiology, potential sequelae, and long-term ramifications of untreated disease. To have patients accept periodontal care, there must be a desire for this treatment, and that is created by education. Also, recognizing the anxieties and phobias of many patients, we must be able to assure the patient that care can be accomplished with minimal discomfort. With recent advances in the use of site-specific, local antibiotics (eg, Arestin®, Warminster, PA; and Atridox®, Ft. Collins, CO), and host modulation by enzyme suppression (eg, subantimicrobial dosage doxycycline), there may be adjunctive conservative approaches to treatment to compliment traditional phase I therapy. The latest nonsurgical conservative techniques can result in more patients accepting treatment.
Host Modulation
A possibly valuable adjunct to nonsurgical conservative periodontal therapy is the use of oral, subantimicrobial dosages of doxycycline.24 The medication is available in 20 mg doses, to be taken twice daily. This dosage has no antibiotic action. In the development of periodontal disease, the bacterial challenge induces a host response releasing proinflammatory cytokines, which cause certain cells of the periodontium to secrete enzymes known as matrix metalloproteinases (MMPs). These enzymes, called collagenases, degrade collagen, which is the major structural protein of the periodontium. When the disease is active, the MMP levels increase, contributing to periodontal disease.25 The data suggests a statistically significant decrease in pocket depth of less than 0.5 mm. It is also clinically significant because, while the average decrease in pocket depth is only 0.5 mm, it is higher for pockets that approach 7 mm. These areas of greater depth are of concern as the teeth may be at risk for extraction, without this additional benefit of treatment. There are also additional optional adjunctive modalities, ie, a short course of clinical dosage of antibiotic therapy, extra scaling, and combination with selective site local-delivery antibiotics that yield more significant pocket reduction.
Locally Administered Anti-Infectives
Locally administered anti-infectives (eg, Arestin and Atridox) have been shown to suppress or eradicate subgingival bacteria, improve attachment levels, and reduce pocket depths and bleeding on probing. The rationale for using these drugs is to deliver a very high concentration of the antibiotic/antimicrobial to affected sites without systemic administration.
Arestin is an encapsulated minocycline that is easy to administer. The microsphere delivery system appears as a powder that immediately adheres to the tissue, delivered through a cartridge attached to an anesthetic-type syringe. The microspheres slowly release the anti-infective agent to maintain an elevated concentration of drug in the crevicular fluid. The drug dissolves out of the microspheres, according to the product insert, which becomes fragmented and completely bioresorbed. The findings from a multicenter study indicate significant pocket depth reduction when used in conjunction with scaling and root planing, compared to scaling and root planing alone.26
There are possible limitations in this technique for all products. These can include lack of access to the site, usually because of an extremely narrow opening, that prevents introduction of the material and possible difficulty in placement.
Management Decisions
Dentists and hygienists can now successfully manage periodontal disease nonsurgically, with simpler and more effective hygiene aids, the use of site-specific anti-infectives, and systemic enzyme suppression with subantimicrobial-dose doxycycline. Pocket depth may now be reduced predictably with conservative procedures such as scaling and root planing. This protocol, which allows for effective conservative, nonsurgical therapy, can now be used for almost every patient.
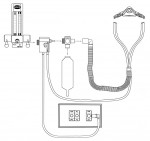
Treatment can now be accomplished with minimal discomfort. New nitrous oxide analgesia systems can reduce anxiety. They should have a failsafe flowmeter, double-mask scavengers with scavenger breathing coaxial tubing and automatic vacuum switches to assume that when gas flows the vacuum is on (Figure 3). This reduces risk and can ensure safety for the patient and staff.
Topical anesthetics are recommended for every patient. Even if the patient does not express an apprehension or fear about treatment, use of the topical assures the clinician that the patient will be comfortable. This is very important because success in treatment requires routine follow-up care. The patient will return for the necessary follow-up and periodontal maintenance treatment if they know that the treatment can be painless.
Oraqix®, a thermogel from DENTSPLY Pharmaceutical (York, PA) containing 2.5% lidocaine and 2.5% prilocaine, produces tissue analgesia so that instrumentation can be painless. It is placed into the pocket painlessly, using a blunt cannula (Figure 4). It is attached to an applicator. The gel is contained in a disposable syringe that is easily inserted into the applicator handle.
Another popular form of analgesic is the new Cetacaine® Topical Anesthetic Liquid Kit, manufactured by Cetylite Industries (Pennsauken, NJ). Cetacaine’s triple-active formula (benzocaine 14%, butamben 2%, tetracaine hydrochloride 2%) is ideal for scaling and root planing, providing patients with effective, non-injectable anesthesia that can be used in a full-mouth application. The bottle has a unique dispenser cap for Luer-lock syringes that allows the clinician to use only what they need. It has an onset of 30 seconds and duration typically lasts 30 to 60 minutes.
Because pain anxiety can deter a patient from accepting treatment, it is valuable to have these treatment aids available to assist in the delivery of care. Even with experience in these technologies, the general dentist may not prefer to manage these more difficult patients. It is advisable to refer these more challenging patients to a periodontist.
Considering all of these advances in technology, we no longer have to watch periodontal disease progress and wait until surgical intervention alone is required to regain health. Now, we can anticipate a stable long-term periodontal condition. With conservative management, using the described technology, patients who want to be healthy will accept treatment recommendations and have the necessary care completed.
References
1. Beck JD, Ek P, Helsa G. Periodontal disease and coronary heart disease: a reappraisal of the exposure. Circulation. 2005;112:19-24.
2. Tonetti MS, D’Aluto F, Nibal L, et al. Treatment of periodontitis and endothelial function. N Engl J Med. 2007;356:911-920.
3. Albander JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in United States, 1988-94. J Periodontol. 1999;70: 13-29.
4. US Department of Health & Human Services. Oral health in America: a report of the Surgeon General (executive summary). Rockville, Md. National Institute of Dental and Craniofacial Research, National Institute of Health; 2000. Available at: www.nidr.nih.gov/AboutNIDCR/SurgeonGeneral/ExecutiveSummary.htm.
5. Williams RC. Periodontal disease. N Engl J Med. 1990;322: 373-382.
6. Wilson TG Jr. Compliance and its role in periodontal therapy. Periodontology. 2000 1996;12:16-23.
7. American Academy of Periodontology. Ad hoc committee on the parameters of care: phase 1 therapy. J Periodontol. 2000: 71(Suppl): 856.
8. Williams RC, Paquette DW, Offenbacher S, et al. Treatment of periodontitis by local administration of minocycline microspheres: a controlled trial. J Periodontol. 2001;72: 1535-1544.
9. Caton JG, Ciancio JG, Blieden TM, et al. Treatment with subantimicrobial dose doxycycline improves the efficacy of scaling and root planning in patients with adult periodontitis. J Periodontol. 2000;71: 531-532.
10. Page P, Offenbacher S, Schroeder H, et al. Advances in the pathogenesis of periodontitis: summary of developments, clinical implications, and future directions. Periodontol 2000. 1997;14: 216-248.
11. Claffey N, Egelberg J. Indications of probing attachment loss following initial periodontal treatment in advanced periodontitis patients. J Clin Periodontol. 1995;22:690-696.
12. Lahig NP, Joss A, Orsanic T, et al. Bleeding on probing: a predictor for the progression of periodontal disease? J Clin Periodontol. 1986;13:590-596.
13. Varrotegham R, Hutchens LH, Garrett S, et al. Bleeding on probing and probing depths as indicators of the response to plaque control and root debridement. J Clin Periodontol. 1987;14:226-230.
14. Kardahl WB, Daluard KL, Patel KD, et al. Long-term evaluation of periodontal therapy: response to 4 therapeutic modalities. J Periodontol. 1986;57:93-102.
15. Hinrichs J, Wofff L, Philstrom B, et al. Effects of scaling and root planning on subgingival microbial proportions standardized in terms of their naturally occurring distribution. J Periodontol. 1985:56:187-194.
16. Smart GJ, Willson M, Davies E, et al. The assessment of ultrasonic root surface debridement by determination of residual endo-toxin ends. J Clin Periodontol. 1990: 17:174-178.
17. Thornton S, Garnick J. Comparison of ultrasonic to hand instruments in the removal of subgingival plaque. J Periodontol. 1982; 53:35-37.
18. Gottehrer N, Reynolds B. Power scalers: the new boom in contemporary periodontics. Dent Today. 1997;16:98-105.
19. Linde J, Nyman S. Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol. 1984;11: 504-514.
20. Chin M, Martin M, Day J. Efficacy of the Sonicare toothbrush for plaque removal in geriatric and special-needs populations. J Dent Hyg. 1996;70: 237-238.
21. Panagakos FS, Volpe AR, Petrone ME, et al. Advanced oral antibacterial/anti-inflammatory technology: a comprehensive review of the clinical benefits of a triclosan copolymer/fluoride dentrifice. J Clin Dent. 2005; 16(suppl):S1-S9.
22. Cobb CM, Rodgers RL, Killoy WJ. Ultrastructure examination of human periodontal pockets following the use of an oral irrigation device in vivo. J Periodontol. 1998; 59:155-163.
23. Thomas JG, Nakasiski LA. Managing the complexity of a dynamic biofilm. J Am Dent Assoc. 2006;137(suppl):10S-15S.
24. Caton J, Cianco SB, Bleden TM, et al. Treatment with subantimicrobial dose doxycycline improves the efficacy of scaling and root planning in patients with adult periodontitis. J Periodontol. 2000;73:521-532.
25. Page R, Korman K. The pathogenesis of human periodontitis: an introduction. Periodontol 2000. 1997;14:9-11.
26. Goodsen JM, Gunsolley JC, Grossi SG, et al. Minocycline HCl microspheres reduce red-complex bacteria in periodontal disease therapy. J Periodontol. 2007;78:1568-1579.
About the Author
Neil R. Gottehrer, DDS
President
Institute of Advanced Oral/Physical Health
Havertown, Pennsylvania