Using Existing Dentures for Wash Impression and Occlusal Registration Records
David R. Avery, AAS, CDT
Approximately 57% of individuals over 65 years of age wear complete dentures.1 In 2000, the US Census Bureau reported that by the year 2010 more than 39 million people will be over 65 years of age.2 This demographic increase, combined with an increase in average educational levels and a strong sense of self, creates the potential for an unserviceable demand for high-quality complete denture treatment from the dental profession. With all indications pointing to a significant pending shortage of clinical and laboratory professionals needed to meet the increased demand, dentists and technicians who prepare for the provision of esthetically pleasing, functional complete dentures will be in great demand.
The author’s experience as a technician for 34 years has led to the conclusion that the technique described is an efficient and predictable method for the initial processes of final impressions and occlusal registrations. The works of Drs. John Frush, Earl Pounds, Walter “Jack” Turbyfill, and Joseph Massad influenced the author’s adaptation of this technique, which has been upgraded through the years, leading to simplified, successful results.
Technique
The technique consists of two steps. In the first step, the existing anterior tooth position is evaluated using phonetic exercises. In the second step, a functional impression is generated.
Evaluate the Existing Anterior Tooth Position Through Phonetic Exercises
Proper contour and normal physiologic movement of the muscles enhances an esthetic denture, whereas improper support can detract from it severely. Positioning the anterior teeth using the mandibular movements of speech is a hallmark of the Pound technique, a method which has proven successful over decades.3
- The pronunciation of the letter “M” places the upper lip at rest at completion, illustrating the amount of display of the central incisors. Men should display 1 mm to 2 mm; women 3 mm to 4 mm.
- The use of the letters “F” and “V” illustrate the appropriate relationship of the incisal edges with the vermillion border. Ideally, the maxillary incisors brush lightly against the border during the formation of these letters.
- The use of the letter “S” aids in the determination of appropriate vertical dimension through evaluation of the “speaking space.” Both men and wo-men should display 1 mm of clearance between the upper and lower incisors during the formation of this letter.
If a significant adjustment in the vertical dimension of occlusion (VDO) is required, the denture(s) can be adjusted to establish the appropriate VDO and incisal edge position on a trial basis. The clinician can articulate the denture before the impression procedure, equilibrate through occlusal reduction, or roughen the incisal and occlu-sal surfaces and add provisional material.
If adjustments in tooth position are desired in the new appliances, the clinician should record the desired changes with a study cast and on the prescription. For the best communication with the technician, also record digital images.
Functional Impression
There are numerous techniques for the capture of final impressions in the edentulous arch to be considered.4,5 In theauthor’s experience, the most accurate is the functional impression. A functional impression is created by applying a functional impression material to the fitting surface of an existing denture. This impression technique creates an impression under functional stresses.6 One functional impression material, Hydro-Cast® (Sultan Healthcare, Englewood, NJ), was developed by Dr. Earl Pounds and Mr. Clark Smith in the 1950s, and remains one of the best kept secrets in dentistry. The described technique using this material can be used when the patient’s existing dentures fit reasonably well. If any borders are overextended, they can be adjusted and polished. If any borders are short, they can be corrected by the addition of Triad® VLC (DENTSPLY Trubyte, York, PA).
1. Prepare the denture base by removing any extreme undercuts as would be performed for a reline impression. This preparation allows the denture to be removed from the master cast without damage to the cast or denture. Also, apply petroleum jelly to the teeth to facilitate easier removal of the tacky Hydro-Cast material at completion.
2. The material consists of a powder (fine-milled alginate) and liquid (ethanol) that are mixed at a ratio of 3:1. Mix the ingredients only enough to incorporate the components (Figure 1a and Figure 1b).
3. Allow the mixture to sit covered for a few minutes, until it reaches a manageable honey-like consistency. Then, load the material into the denture base. Border-mold the impression as normal during setting. The initial set takes 3 to 5 minutes (Figure 2).
4. On removal of the denture from the mouth, any premature pressure areas should be evident from the acrylic base bleed through. Adjust any premature contact areas with an acrylic carbide bur, mix and add new material, and reseat. Excess external material can be removed with a heated carving instrument.
5. After a satisfactory initial result, dismiss the patient with instructions to return in 4 to 5 days for evaluation of the functional result. The material does not reach a complete set until this period, thus the functional impression is accomplished. This technique also provides for tissue conditioning. Tissue conditioning occurs when a soft material applied to the fitting surface of a denture allows for more equal distribution of load and a return of the mucosal tissue to its normal position.6 Hydro-Cast is such a soft material. Tissue conditioning may need to be repeated over several visits to allow abused soft tissue to reach a satisfactory condition (Figure 3a). Therefore, Steps 1 through 5 may need to be repeated over multiple office visits.
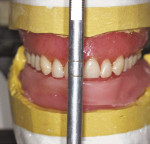
6. On completion of the tissue conditioning and the final impression, take a bite registration, preferably with a vinyl or other static material. Then, pour the master casts and articulate the dentures (Figure 3b).
7. In cases where upper and lower complete dentures are to be fabricated, additional steps are needed to ensure proper positioning of the maxillary anterior teeth on the new denture.
8. On articulation of the dentures, remove only the lower denture from the master cast.
9. Place a roll of silicone lab putty or baseplate wax on the lower cast and close the articulator, capturing the upper denture teeth in the roll (Figure 4a). In the case of a single maxillary denture, a silicone putty matrix can be accomplished by adapting the putty to the facial surfaces of the mandibular anterior teeth and the maxillary denture teeth (Figure 4b).
10. Capture an alginate duplicate of the existing upper denture for the development of a study cast for the technician’s use (Figure 5a).
11. The technician can place the incisal edges of the new anterior teeth in exactly the same position as the existing denture. If any adjustments in position are desired, the technician has a very specific starting point for reference and measurement (Figure 5b).
The billing codes for each conditioning appointment are: D5850 (maxillary conditioning) and D5851 (mandibular conditioning).
Conclusion
The steps described are accomplished best by scheduling the patient at the beginning of the day, pouring the master casts, trimming, articulating, and retrieving the dentures through the course of the day with the patient returning at the end of the day to retrieve the dentures. While this method creates accurate final impressions and occlusal registrations, it does require a little more time and effort from the clinician and staff. This investment of time is returned when the patient returns for a predictable wax try-in, typically requiring little to no adjustment. Also, the costs of the custom tray, occlusion rim, and associated chair time are added benefits to the clinician and staff. This streamlined procedure is repeatable and predictable, and provides the patient with a better chance for a successful outcome.
Disclosure
The author has received honoraria from and is a current consultant for DENTSPLY International.
References
1. Ivanhoe JR, Cibirka RM, Parr GR. Treating the modern complete denture patient: a review of the literature. J Prosthet Dent. 2002;88(6): 631-635.
2. Easterlin R. Growth and composition of the American population in the twentieth century. In: Haines MR, Steckel RH, eds. A Population History of North America. New York, NY: Cambridge University Press; 2000.
3. Turbyfill WF. Regaining pleasure and success with complete denture services. Int J Prosthodont. 1989;2(5):474-482.
4. Kois JC, Fan PP. Complete denture impressioning technique. Compend Contin Educ Dent. 1997;18(7):699-708.
5. Massad J, Davis WJ, Lobel W, et al. Improving the stability of maxillary dentures: the use of polyvinyl siloxane impression materials for edentulous impressions. Dent Today. 2005;24(2):118-123.
6. Wilson HJ, Tomlin HR, Osborne J. Tissue conditioners and functional impression materials. Br Dent J. 1966;121:9-16.
About the Author
David R. Avery, AAS, CDT
Director of Training and Education
Drake Precision Dental Laboratory
Charlotte, North Carolina