Resilon Update
Gregori M. Kurtzman, DDS
Traditionally, endodontic treatment requires instrumentation of the root canal to remove infectious debris, leaving clean canal walls. After the instrumentation and irrigation of debris from the canal is complete, the root canal is filled with gutta-percha inserted with an endodontic sealer. These sealers to be used with gutta-percha have included calcium hydroxides, zinc-oxide and eugenol cements, and glass ionomer cements. When Resilon™ (Pentron® Clinical Technologies, LLC, Wallingford, CT) was introduced 4 years ago, much concern was expressed for this obturation material, ranging from how would it geometrically fill canals compared to gutta-percha to whether it could provide a seal equal to zinc oxide/eugenol (ZOE) or AH-26 (epoxy resin root canal sealer). In the meantime, the literature has been filled with numerous peer-reviewed articles reporting on many aspects involving Resilon. This article addresses the concerns and discusses some of the literature that has been published on Resilon.
Resilon is a core obturation material alternative to gutta-percha and requires a sealer to complete obturation of the canal system. Several studies have used a methacrylate resin sealer, such as Epiphany™ (Pentron Clinical Technologies)—which is also sold as RealSeal, (SybronEndo, Orange, CA) as a sealer system with Resilon as the core obturation material. Another product falling into this category of methacrylate sealers is EndoRez (Ultradent, South Jordan, UT). Presently, alternatives to Resilon available on the market consist of resin-coated gutta-percha cones (EndoRez cones); Resilon is the only solid resin cone being offered at this time. Resilon is also available as a terminus on a fiber obturator that allows one to obturate the canal and place a fiber post simultaneously with a methacrylate sealer. This application is available as Innuendo (Heraeus Kulzer, Armonk, NY).
Leakage
Coronal leakage has been indicated as a major determinant of endodontic success or failure. When the coronal portion of the tooth is not sealed with a restorative material that resists microleakage, the tooth is at risk of bacterial infiltration and failure of the endodontic filling. Microleakage continues to be a main reason for the failure of root canal therapy, where the challenge has been to achieve an adequate seal between the internal tooth structure and the main obturation material.
Coronal leakage for even a minimal amount of time may quickly lead to apical migration of bacteria. Research has demonstrated that when exposed to artificial and natural saliva for as little as 2 days, a root canal filling will have leakage and bacterial contamination to the root apex.1 Studies using gutta-percha and various sealers indicate that gutta-percha will consistently allow bacterial leakage. But use of an adhesive sealer can significantly slow or stop coronal-apical bacterial migration.2
Gutta-percha has limitations in its resistance to coronal leakage, which have been overcome with the newer resin alternatives. Although sealers can form close adhesion to the root canal wall, none is able to bond to the gutta-percha core material. Upon setting, shrinkage of the sealer allows the sealer to pull away from the gutta-percha core, leaving a microgap through which bacteria may pass.3 In studies performed at the University of North Carolina, the gutta-percha test group demonstrated leakage in 80% of specimens regardless of the obturation technique or which sealer was used.4
A dog model was used to assess and compare in vivo the efficacy of gutta-percha and AH-26 sealer vs Resilon with Epiphany primer and sealer-filled roots in preventing apical periodontitis subsequent to coronal inoculation with oral microorganisms. Mild inflammation was reported in 82% of roots filled with gutta-percha and AH-26 sealer, which was statistically more than roots filled with Resilon-obturated teeth (19%). Resilon was also associated with significantly less apical periodontitis (82% vs 19%, McNemar paired analysis, P < .05), which may be due to its superior resistance to coronal microleakage.5
As measured using dye penetration methodology, the least apical leakage was shown with Resilon.6,7 The differences in leakage among the groups in this study showed gutta-percha with AH-26 (2.4 mm, standard deviation [SD]: 1.87 mm), gutta-percha with AH plus (2.1 mm, SD: 1.69 mm), and Resilon (1.7 mm, SD: 1.32 mm) were statistically significant (P < .001). An alternative study, using the fluid transport method of teeth filled with gutta-percha and AH-26, exhibited the most leakage. The least leakage was seen with Epiphany sealer and Resilon core material. The differences in leakage among the groups were statistically significant (P < .05).8 It was concluded that of the materials tested under the conditions of this study, Epiphany allowed the least leakage. This was supported in an independent study where two-way ANOVA analysis indicated significantly less (P < .05) leakage using Resilon with Epiphany sealer compared to gutta-percha and AH-26 plus sealer.9
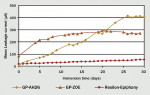
The results of dye penetration and fluid filtration studies were supported by electrophoresis leakage studies conducted by this author. A detector electrode was placed coronally in each specimen root in the study, which was in contact with the obturation system and sealed in place with the apices left patent. The teeth were immersed in 0.9% sodium chloride with a stainless steel counter electrode. A 20-V potential was then connected between the electrode and each tooth in turn, with current flow determined by voltage drop across a standard resistor. Leakage was followed for 30 days and statistically analyzed for differences between groups. When comparing specimens obturated with gutta-percha and AH-26 to Resilon-Epiphany, there was a significant difference (P < .001) in leakage behavior between the groups.10 Further electrophoresis leakage studies looking at gutta-percha and ZOE sealer also found significantly superior (P < .001) leakage resistance in the Resilon-Epiphany specimens (Figure 1).11
The findings of these studies indicated that when teeth were obturated with Resilon-Epiphany, the leakage behavior was an order of magnitude less than that found with conventional obturation. These and previous findings suggest that when the Resilon-Epiphany system is used under conditions common for dentin bonding, it can provide a significant improvement in leakage resistance compared to gutta-percha techniques.
Obturation
Calcium hydroxide has been advocated as an intracanal medicament when endodontics cannot be completed in a single appointment. When obturation is to be performed at a subsequent appointment, it is recommended that irrigation with 17% ethylenediaminetetracitic acid (EDTA) be used to remove any remnants of the calcium hydroxide. When this was performed it was found that calcium hydroxide did not adversely affect the seal of the root-canal system filled with Resilon.12
Additionally, standard obturation techniques call for disinfection of the obturation cones to be immersed in either sodium hypocholorite (NaOCl) before introduction into the canal system. Some practitioners are alternatively using chlorhexidine. One study found that a 1-minute immersion in either solution did not show any significant deterioration on the Resilon cone’s surface.13 However, since NaOCl affects dentin bonding, chlorhexidine appears to a better choice as an immersion agent for cones.
Resin sealers have been shown to have potential setting issues in oxygen-rich environments (aerobic), but set well in an anaerobic environment. It has been reported that Resilon sealer sets in 30 minutes in anaerobic environments, such as those normally found in the canal following obturation. However, in the presence of air, Resilon took 1 week to set.14 The key is limiting oxygen in the canal system. Irrigants and lubricants that can liberate oxygen or inhabit resin setting (ie, NaOCl, peroxides) in the canal may be used but flushing out the tooth with a neutralizing irrigant such as EDTA or chlorhexidine will create an environment that will allow setting in the allotted time.
Occasionally an endodontically treated tooth will require retreatment. The concern with resin obturation is that the progression of an instrument to working length may be extremely difficult if not impossible due to the hardness associated with resins. Resilon obturation consists of a soft core material (Resilon) with a methacrylic resin sealer (Epiphany). Reports in the literature support the ability of progression of a file through the Resilon-obturated canal, permitting retreatment should it be necessary. Actually, Resilon was faster to remove than gutta-percha and resulted in cleaner canal walls in the apical third of the teeth obturated with Resilon when compared to gutta-percha.15,16
But what if a perforation occurs during instrumentation? Can a resin obturation still be used? A study reported by Maltezos and Glickman found that compared to mineral trioxalate (MTA) there was no statistical significance in bacterial leakage, but Resilon leaked significantly less than Super-EBA™ (Bosworth, Skokie, IL) when used as a apical filling material.17 Resilon may be a viable option as a retrograde filling material with good surgical isolation and moisture control. With regard to perforations, this offers indications that a good seal can be achieved when exposed to the periodontal ligament (PDL) space, and placement of MTA to seal the perforation before obturation may not be necessary.
Fracture Resistance
Consideration of the structural aspects of the tooth is critical in the long-term management of endodontically treated teeth. Forces placed on the tooth during function make the tooth vulnerable to fracture.18,19 Microfractures present prior to endodontic therapy may propagate under load, leading to clinically significant cracks that can eventually lead to the loss of the tooth. The process of instrumentation itself may weaken the tooth as the canals are enlarged to properly shape and disinfect the root canal system.20 Endodontically treated teeth have been reported in the literature to be more susceptible to fracture because they possess reduced dentinal toughness, lower water content, and deeper cavities.21
Additionally, the cervical aspect of the tooth is subjected to significant compressive, tensile, and torsional forces during function and bruxism, which can lead to the fatigue of the weakened tooth structure, increasing its likelihood of fracture.22 Therefore, root canal treatment should include stabilization of the canal and coronal aspect. A key element in this methodology is obturation to assist in reinforcing the remaining tooth structure.24-26
Studies have reported a significant increase in the fracture resistance of endodontically treated teeth. When restored with a composite intracoronally with routine acid-etch and bonding procedures, they can achieve strength levels almost approximating those of intact teeth.27 Resilon, because of its intracanal bond, has been shown to increase resistance to tooth fracture when compared to obturations using gutta-percha and commonly used sealers (ie, ZOE or AH-26).28 Micro push-out studies comparing the bond strength of Resilon to that of gutta-percha found that mean bond strength to root canal dentin was significantly higher in the Resilon/Epiphany group.29 The advantage to the use of resin obturation materials in the management of endodontically treated teeth can result in a stronger, more retentive restoration. This may be a significant benefit for teeth weakened by endodontic procedures.30 One study found that canals obturated with Resilon/Epiphany obturation material increased the in vitro resistance to fracture when compared with standard gutta-percha techniques. Resilon demonstrated a 25% increase in root strength than gutta-percha samples.28 Indications are that resin obturation may provide enhanced resistance to tooth fracture.31
Biocompatibility
Cytotoxicity is an important consideration when selecting an obturation material. The obturation material should not negatively affect the hosts cells found in the PDL. The literature has repeatedly reported gutta-percha as well tolerated by host cells with no inflammatory reaction noted. Examination of fibroblast cells found that Resilon was similar to gutta-percha in how the cells reacted. But the sealers used can lead to more reactions as these have to undergo a setting reaction and may potentially have a cytotoxic potential. Epiphany was found to be less cytotoxic than Grossman’s sealer (ZOE- based) at both the 1- and 24-hour time periods. But Epiphany was found to be more cytotoxic than Sealapex (SybronEndo), which is calcium hydroxide-based, at the 1-hour time period but less cytotoxic at the 24-hour time period.32
In evaluating intraosseous biocompatibility that may occur when sealer is extruded past the apex, Sousa studied AH-26, EndoRez, and Epiphany. After analyzing both time periods, the inflammatory tissue reaction to EndoREZ was considered severe. In the AH Plus group, the reaction changed from severe to moderate, while biological compatibility to Epiphany was observed with bone formation and a slight to no inflammatory reaction. The conclusion was that Epiphany root canal sealer was the only material that presented intraosseous biocompatibility.33
Conclusion
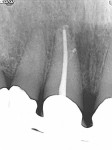
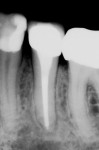
Coronal leakage has been increasingly recognized as a major cause of endodontic failure. Multiple studies have demonstrated that Resilon offers a significant improvement in leakage resistance compared to gutta-percha and the traditional sealers ZOE or AH-26. Additionally, resin obturation may strengthen the remaining tooth structure, improving the long-term prognosis for teeth obturated with Resilon (Figure 2; Figure 3; Figure 4; Figure 5; Figure 6; Figure 7; Figure 8).
Disclosure
The author has received honoraria from Pentron Clinical Technologies for lecturing and has participated in funded research on Resilon/Epiphany.
References
1. Khayat A, Lee SJ, Torabinejad M. Human saliva penetration of coronally unsealed obturated root canals. J Endod 1993;19(9):458-461.
2. Britto LR, Grimaudo NJ, Vertucci FJ. Coronal microleakage assessed by polymicrobial markers. J Contemp Dent Pract. 2003;4(3): 1-10.
3. Teixeira FB, Teixeira EC, Thompson J, et al. Dentinal bonding reaches the root canal system. J Esthet Restor Dent. 2004;16(6):348-354.
4. Shipper G, Orstavik D, Teixeira FB, et al. An evaluation of microbial leakage in roots filled with a thermoplastic synthetic polymer-based root canal filling material (Resilon). J Endod. 2004;30(5):342-347.
5. Shipper G, Teixeira FB, Arnold RR, et al. Periapical inflammation after coronal microbial inoculation of dog roots filled with gutta-percha or resilon. J Endod. 2005;31(2):91-96.
6. Bodrumlu E, Tunga U. Apical leakage of Resilon obturation material. J Contemp Dent Pract. 2006;7(4):45-52.
7. Aptekar A, Ginnan K. Comparative analysis of microleakage and seal for 2 obturation materials: Resilon/Epiphany and gutta-percha. J Can Dent Assoc. 2006;72(3):245.
8. Tunga U, Bodrumlu E. Assessment of the sealing ability of a new root canal obturation material. J Endod. 2006;32(9):876-878.
9. Stratton RK, Apicella MJ, Mines P. A fluid filtration comparison of gutta-percha versus Resilon, a new soft resin endodontic obturation system. J Endod. 2006;32(7):642-645.
10. von Fraunhofer JA, Kurtzman GM, Norby CE. Resin-based sealing of root canals in endodontic therapy. Gen Dent. 2006;54(4):243-246.
11. Kurtzman GM, von Fraunhofer JA, Oliveira DP. Endodontic Leakage Resistance of Fiber Obturators. Poster presentation AADR, Orlando, FL 2006, #1443.
12. Wang CS, Debelian GJ, Teixeira FB. Effect of intracanal medicament on the sealing ability of root canals filled with Resilon. J Endod. 2006;32(6):532-536. Epub 2006.
13. Isci S, Yoldas O, Dumani A. Effects of sodium hypochlorite and chlorhexidine solutions on Resilon (synthetic polymer based root canal filling material) cones: an atomic force microscopy study. J Endod. 2006;32(10):967-969.
14. Nielsen BA, Beeler WJ, Vy C, et al. Setting times of Resilon and other sealers in aerobic and anaerobic environments. J Endod. 2006;32(2):130-132.
15. de Oliveira DP, Barbizam JV, Trope M, et al. Comparison between gutta-percha and resilon removal using two different techniques in endodontic retreatment. J Endod. 2006;32(4):362-364.
16. Ezzie E, Fleury A, Solomon E, et al. Efficacy of retreatment techniques for a resin-based root canal obturation material. J Endod. 2006;32(4):341-344.
17. Maltezos C, Glickman GN, Ezzo P, et al. Comparison of the sealing of Resilon, Pro Root MTA, and Super-EBA as root-end filling materials: a bacterial leakage study. J Endod. 2006;32(4):324-327.
18. Gutmann JL. The dentin-root complex: Anatomic and biologic considerations in restoring endodontically treated teeth. J Prosthet Dent.1992;67(4):458-467.
19. Lindauer PA, Campbell AD, Hicks ML, et al. Vertical root fractures in curved roots under simulated clinical conditions. J Endod. 1989;15(8):345-349.
20. Trope M, Ray HL Jr. Resistance to fracture of endodontically treated roots. Oral Surg Oral Med Oral Pathol. 1992;73(1):99-102.
21. Madison S, Wilcox LR. An evaluation of coronal microleakage in endodontically treated teeth. Part III. In vivo study. J Endod. 1988;14(9):455-458.
22. Caputo AA. Standlee JP. Biomechanics in Clinical Dentistry. Berlin: Quintessence Publishing; 1987;21-27.
23. Craig RG, Farah JW. Stress analysis and design of single restorations and fixed bridges. Oral Sci Rev. 1977;10:45-74.
24. Kanca J 3rd. Conservative resin restoration of endodontically treated teeth. Quintessence Int. 1988;19(1):25-28.
25. Share J, Mishell Y, Nathanson D. Effect of restorative material on resistance to fracture of tooth structure in vitro. J Dent Res. 1982;61(Special Issue #622):247.
26. Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol. 1985;1(3):108-111.
27. Hernandez R, Bader S, Boston D, Trope M. Resistance to fracture of endodontically treated premolars restored with new generation dentin bonding systems. Int Endod J. 1994;27(6):281-284.
28. Teixeira FB, Teixeira EC, Thompson JY, et al. Fracture resistance of roots endodontically treated with a new resin filling material. J Am Dent Assoc. 2004;135(5):646-652.
29. Skidmore LJ, Berzins DW, Bahcall JK. An in vitro comparison of the intraradicular dentin bond strength of Resilon and gutta-percha. J Endod. 2006;32(10):963-966. Epub 2006.
30. Teixeira FB. Ideal obturation using synthetic root-filling systems: coronal sealing and fracture resistance. Pract Proced Aesthet Dent. 2006;18(3):S7-11.
31. Hafez et al. Regional Bond Strength of Epiphany/Resilon to Intraradicular Dentin. University of Iowa, Iowa City, IA. Abstract: #PR12, J Endod. Vol. 32(3), March 2006.
32. Key JE, Rahemtulla FG, Eleazer PD. Cytotoxicity of a new root canal filling material on human gingival fibroblasts. J Endod. 2006;32(8):756-758.
33. Sousa CJ, Montes CR, Pascon EA, et al. Comparison of the intraosseous biocompatibility of AH Plus, EndoREZ, and Epiphany root canal sealers. J Endod. 2006;32(7):656-662.
About the Author
Gregori M. Kurtzman, DDS
Private Practice
Silver Spring, Maryland