Using GuttaFlow®, ParaPost® Fiber Posts, and ParaCore Build-up Materials to Restore Damaged Teeth
Ricardo Caicedo; Paulino Castellon; Joseph Fullmer
It is generally accepted that the successful treatment of a severely damaged tooth with pulpal disease depends not only on good endodontic treatment, but also on good prosthetic restoration of the tooth immediately after root canal treatment is completed. It is recommended that a post-and-core system is used to restore an endodontically treated tooth that has suffered significant loss of coronal structure. The post-and-core systems contain three components of different rigidity: the post, the cement, and the core material. As the most rigid component, the post is able to resist forces without distortion; as a result, stress is transferred to the least rigid substrate, the dentin, and may lead to failure.1
The difference between the elastic modulus of dentin and post material is a source of stress for the root structures. Metal cast posts have been used to restore endodontically treated teeth, but ideal canal preparation is paramount for the success of this type of post.2 As a result, the use of composite glass ionomers and amalgam core has been advocated to avoid the insertion of metal posts into the root canal.3
Using new adhesive materials and technology, clinicians can bond the post securely to the dentin in the root canal space, the core build-up to the post, and the final crown restoration to the core and tooth, with all components having similar physical properties bonded together as one unit.
Retention between bonding systems and the core material is vital to the longevity of the restoration. For optimum bond strength, adhesive and core materials must be compatible.4 ParaPost® Fiber White, ParaPost® Fiber Lux, ParaCem®, and ParaPost® ParaCore (Coltene/Whaledent Inc, Cuyahoga Falls, OH) materials all meet these criteria.
It is important to remember that the success of a post-and-core restoration hinges upon many factors, one of which is the success of the endodontic procedure. In this article we will discuss the GuttaFlow® method of root canal treatment with which the cases presented were treated. The GuttaFlow system is a new self-curing filling system for root canals that combines two products in one: gutta percha in particle form (less than 30 µm) and sealer. This injectable system provides a reliable and time-saving obturation. The flowable gutta percha is composed of polydimethylsiloxane, gutta-percha powder, zinc oxide, zirconium dioxide, silicone oil, paraffin-base oil, colloidal silver (preservative), hexchioroplatinic acid (cata-lyst), and coloring. Properties of GuttaFlow include: high sealing ability requiring only one master gutta-percha point, homogeneously mixed flowable gutta percha that flows into isthmuses and lateral canals, and radiopaqueness. GuttaFlow consists of two components in one capsule that are activated by compression. The capsule is mixed for only 30 seconds in a standard triturator. Removal of the GuttaFlow, in preparation for post insertion, is similar to that of traditional gutta percha.
This article describes a post-and-core technique previously used in 17 cases over a period of 24 months and described in a separate article where a severely damaged molar was restored.5 During that period, there were no failures on the restored teeth due to root fracture, debonding, or core failure.
CASE 1
A 62-year-old man needing treatment of teeth Nos. 23 through 26 was referred to our clinic for evaluation due to periapical radiolucencies in the above mentioned teeth (Figure 1). He reported a period of cold and hot sensitivity 8 months prior but had not had any temperature tenderness for several months. The pulpal and apical diagnosis was necrosis in addition to chronic apical periodontitis.
CASE 2
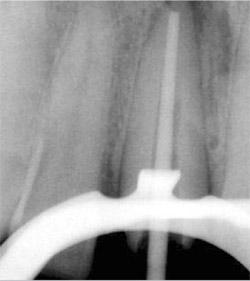
A 53-year-old woman who had had previous root canal treatment and a prefabricated post-and-core restoration on tooth No. 8 (Figure 2) was referred to the endodontic clinic because of periapical radiolucence. The patient reported throbbing pain in the maxillary central incisors region for several weeks. The apical diagnosis was chronic apical periodontitis because of root canal failure. The post was removed using ultrasonic energy (Figure 3 and Figure 4).
CASE TREATMENTS
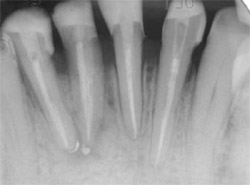
Root canal treatments using the crown-down technique and GuttaFlow filling material were performed on the canals of each case (Figure 5 and Figure 6). The crown structure of the teeth in Case One was restored with ParaPost Fiber White, and in Case Two with ParaPost Fiber Lux after post removal (Figure 7 and Figure 8). The posts were cemented with ParaCem, and the build-ups with ParaPost ParaCore, and full metal-ceramic crowns were posteriorly cemented as a part of the patients’ general treatment plan (Figure 9, Figure 10, Figure 11). Both cases were followed up on clinically for 12 months.
On the final periapical radiograph following obturation, the apical space, width, and length of the root canals were checked (Figure 5 and Figure 8). The working field was isolated with a rubber dam. Two thirds of the total canal length of the canals was used for the post space. The GuttaFlow was removed to the desired depth using a Touch’n Heat 5004 instrument (SybronEndo, Orange, CA) leaving 5 mm of GuttaFlow in the canals (Figure 8 and Figure 12).
A rotary reamer was selected according to the canal thickness on the radiograph using a template provided in the post system in both cases. The canals were prepared using a low-speed handpiece. For Case 1, a 4.5-mm rotary reamer was selected for the canals. ParaPost Fiber White drills was used with a slow-speed contra-angle. The 4.5 ParaPosts Fiber White were cut at the apical aspect to the required length with a diamond-finishing bur (Figure 7) in Case 1. A 5.5 ParaPost Fiber Lux was used in Case 2 (Figure 8).
After try-in and before cementation, the posts were cleaned gently with an alcohol swipe. The canals were cleaned and disinfected using a chelating agent with an ultrasound activation for 30 seconds and thorough irrigation of sodium hypochlorite.6,7 At that point, the canals were etched for 15 seconds with 37% phosphoric acid, rinsed with water, and dried with paper points, leaving the surface slightly moist.
ParaBond Non-Rinse Conditioner from the ParaPost Cement Intro Kit was applied. Equal parts of adhesive conditioner ParaBond A and ParaBond B were mixed, applied to the canals with an endodontic paper point, and air-dried for 3 seconds. Conditioner was applied along the posts. The ParaCem base and catalyst were mixed in equal parts and layered uniformly along the canals using an endodontic file.
Cement was applied along the canals, using an endodontic file of the same size as the canals, and the posts were placed into the canals to full depth, allowing excess cement to vent. Excess cement was cleaned; at that point, the dentin and coronal portions of the posts were etched for 15 seconds with 37% phosphoric acid, rinsed with water, and blotted dry, leaving a moist surface (Figure 13).
A ParaForm matrix was adapted, and ParaCore was injected around the post, tooth structure, and matrix form. Excess ParaCore was removed with an explorer, and each surface of the tooth was photo-cured for 30 seconds. At that point, the tooth was ready to be prepared for prosthetic restoration (Case 1: Figure 14, Figure 15, Figure 16, Figure 17; Case 2: Figure 18 and Figure 19).
DISCUSSION
Straight-line access of the canal system is desirable in endodontic treatment to minimize the unnecessary instrumentation and removal of root-dentin structure.8 The most important consideration regarding the use of a post system are the following principles:
- removal of the smear layer, debris, and sealer/gutta-percha remnants in order to increase retention with a pretreatment of the dentinal canal wall with a chelating agent, ultrasound activation, and sodium hypochlorite before the etching procedure and post cementation;
- adequate length;
- adequate resistance form and adequate strength to allow preservation of dentin structure; and
- an adequate ferrule.
If these principles are followed, most post systems will perform well.7
The ParaPost Fiber White and ParaPost Fiber Lux translucent fiber-reinforced post-and-core system, together with an adhesive cementation procedure, may reduce the incidence of root fracture compared to metal posts. However, posts differ among brands, making careful selection very important. Although this new generation of bonded fiber posts seems promising, long-term clinical data are still accumulating, and other fiber post-and-core systems merit investigation.
DISCLAIMER
The authors have no commercial affiliation with the company manufacturing the products used in these clinical cases.
REFERENCES
1. Sorensen JA, Martinoff JT. Clinically significant factors in dowel design. J Prosthet Dent. 1984;52(1):28-35.
2. Shillingburg HT, Hobo S, Whitsett LD, et al. Fundamentals of Fixed Prosthodontics, 3rd edition. Chicago, IL: Quintessence Publishing Co.;1997: 194-204.
3. Sorensen JA, Engelman MJ. Effect of post adaptation on fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;64(1): 419-424.
4. Dietschi D, Romelli M, Goretti A. Adaptation of adhesive post and cores to dentin after fatigue testing. Int J Prosthodont. 1997;10(6):498-507.
5. Caicedo R, Castellon P. Using ParaPost Tenax fiberglass and ParaCore build-up material to restore severely damaged teeth. Gen Dent. 2005;53(3): 200-203.
6. Standlee JP, Caputo AA. Endodontic dowel retention with resinous cements. J Prosthet Dent. 1992;68:913-917.
7. Serafino C, Gallina G, Cumbo E, et al. Ultrasound effects after post space preparation: An SEM study. J Endod. 2006;32 (6): 549-552.
8. Caicedo R, Clark S, Rozo L, et al. Guidelines for access cavity preparation in endodontics. Dental CE Digest. 2006;3(2):13-20.
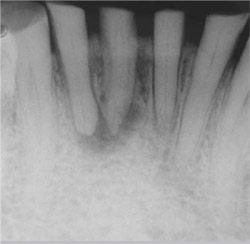 | 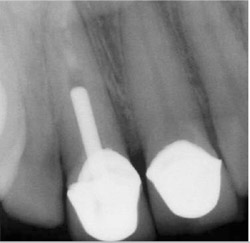 | ||||||||
| Figure 1 Preoperative radiograph of teeth Nos. 23 through 26. Note the loss of coronal tooth structure. | Figure 2 Preoperative radiograph of tooth No. 8 showing the previous metal post and failed root canal treatment. | ||||||||
 |  | ||||||||
| Figure 3 Metal post removed with ultrasonic energy from failed restoration. | Figure 4 Radiograph of tooth No. 8 showing canal space after post was removed using ultrasonic energy. | ||||||||
 |  | ||||||||
| Figure 5 Root canal treatment of teeth Nos. 23 through 26 using GuttaFlow. | Figure 6 Root canal treatment of tooth No. 8 using GuttaFlow with gutta-percha master cone. | ||||||||
 |  | ||||||||
| Figure 7 ParaPost Fiber White posts adapted and ready for cementation. | |||||||||
| Figure 8 Radiograph of tooth No. 8 showing ParaPost Fiber Lux before cementation. | |||||||||
 |  | ||||||||
| Figure 9 Postoperative view of the final restoration using the ParaPost Fiber White system. | Figure 10 Postoperative photograph of finished restoration of tooth No. 8 using ParaPost Fiber Lux esthetic system. | ||||||||
 |  | ||||||||
| Figure 12 Prepared canals ready for placement of Fiber White glass fiber posts. | |||||||||
 | |||||||||
| Figure 11 Postoperative radiograph of final restoration of tooth No. 8 using the ParaPostFiber Lux esthetic system. | Figure 13 Occlusal view of teeth Nos. 23 through 26, showing acid-etching with 37% phosphoric acid after the posts have been cemented in each canal. | ||||||||
 |  | ||||||||
| Figure 14 Core material cured and ready for preparation for the final restoration. | Figure 15 Postoperative radiograph of teeth Nos. 23 through 26 shows Fiber White posts are cemented to adequate length and periapical lesions are healing. | ||||||||
 |  | ||||||||
| Figure 16 Prepared teeth Nos. 23 through 26. | Figure 17 Temporary restorations using the ParaPost Fiber White system. | ||||||||
 Figure 18 Radiograph showing cemented ParaPost Fiber Lux in place in tooth No. 8 and prepared core. |  | ||||||||
| Figure 19 The prepared tooth with ParaPost ParaCore. | |||||||||
| |||||||||





