The Esthetic Management of Multiple Missing Anterior Teeth
Frank M. Spear
Replacing a single anterior tooth with implants or a fixed partial denture can be difficult, but it results in a fairly predictable esthetic outcome. Even if significant bone and soft tissue were lost with the tooth, in the hands of a skilled team of dentists the result is generally acceptable. The loss of multiple missing anterior teeth, especially if they are adjacent to each other, is a much more difficult esthetic challenge. This difference has to do with the biology of the periodontium and the response of the bone and soft tissues when one tooth is lost as opposed to multiple teeth. The understanding of these differences has progressed dramatically over the last two decades thanks to the research that has been done on the soft tissue and osseous response surrounding tooth removal and the placement of anterior implants.
Single Tooth Loss
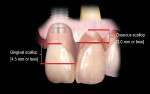
It is helpful to look at the differences in soft tissue response to the possible scenarios a dentist might face, starting with the loss of a single anterior tooth and then progressing to the loss of multiple adjacent teeth. If a single tooth implant is placed, the interproximal papilla levels will be determined by the height of the interproximal bone on the adjacent natural teeth, not the interproximal bone on the implant.1-3 In the average patient the papilla height will be 4 mm to 4.5 mm above the interproximal bone on the adjacent natural teeth (Figure 1). If the natural teeth have no bone loss, the papilla height will be very similar after tooth loss to what they were before tooth loss because the average papilla height above bone between natural teeth is also 4.5 mm.4,5
The facial margin around the implant, however, is not related to the bone on the adjacent natural teeth but rather to the facial bone levels on the implant as well as the thickness and position of the free gingival margin before the tooth removal.6,7 On a single tooth implant, it is much easier to gain gingival margin thickness and height with augmentation procedures than it is to gain papilla thickness and height.8 For a single anterior implant, the least predictable soft tissue outcome is when the adjacent natural teeth have interproximal bone loss, because managing the papilla heights can be very difficult.
These same rules hold reasonably true for the replacement of a single anterior tooth with a pontic as well. The final papilla location is influenced by the bone on the adjacent natural teeth, and the free gingival margin location is dictated by the location of the bone and the thickness of tissue on the facial of the pontic. The one significant difference when comparing pontics with implants concerns the height of interproximal tissue above the bone. Whereas this height averages 4.5 mm between natural teeth, or between a natural tooth and an implant, it has been shown that following soft tissue grafting the amount of tissue above the bone interproximally between a pontic and a natural tooth or between a pontic and an implant averages 6.5 mm. In fact, in some patients it can be as high as 9 mm.9 Therefore, if the adjacent natural teeth in a single tooth replacement situation have bone loss, soft tissue ridge augmentation followed by placement of a pontic can achieve greater coronal height of the papilla than a single tooth implant could in the same situation. To match the esthetics of the pontic with a single tooth implant, it is necessary to erupt the adjacent natural teeth to move the interproximal bone coronally, and then crown-lengthen the facial to re-create the correct length of the adjacent teeth.
Multiple Tooth Loss
With an understanding of what occurs biologically when a single anterior tooth is removed, it is now possible to discuss in detail the loss of multiple anterior teeth. If the multiple teeth being lost are not adjacent to each other, the rules of treatment are the same as with a single tooth. The real challenge of multiple tooth replacement occurs when adjacent teeth have been lost or are already missing.
In the loss of two maxillary central incisors, the response of the papilla between them and adjacent remaining lateral incisors would be the same as in a single tooth replacement situation. That is, the interproximal bone on the remaining lateral incisor will determine the papilla height between the centrals and laterals. The facial free gingival margin height on each central will also be similar in response to a single missing tooth. That is, the facial bone level and tissue thickness will determine where the facial gingival margin ends up. Just as in the single tooth situation, if the facial gingival margin is less than ideal, it is much easier to augment in both height and thickness on both centrals with a soft tissue procedure than it is to improve the height of the papilla.
The real challenge when removing the two centrals is to evaluate what happens to the papilla between them following extraction.10,11 Before extraction the osseous crest around both centrals, assuming no periodontal disease exists, roughly follows the scalloped nature of the cemento-enamel junctions as they flow from the facial into the interproximal resulting in an average osseous scallop of 3 mm. Therefore the average interproximal bone height is 3 mm coronal to the facial crest of bone. Since the soft tissue typically follows the scallop of the bone, the osseous scallop results in a gingival scallop of 3 mm. However, when teeth are present an interesting phenomenon occurs. The gingiva on the facial of the tooth is positioned so that on average the free gingival margin is 3 mm coronal to the crest of bone. But as we saw earlier, the interproximal papilla between teeth is positioned on average 4.5 mm coronal to the interproximal crest of bone, 1.5 mm on average more coronal to the crest of bone than the facial tissue is. This additional 1.5 mm with the 3 mm average osseous scallop results in the tip of the papilla being an average 4.5 mm to 5 mm coronal to the facial free gingival margin (Figure 2).
To understand the challenge following tooth removal, it is necessary to understand what occurs to the osseous scallop and papillary soft tissue height above bone following tooth removal. To a certain extent the answer is determined by how the central incisors will be replaced, and how the method of replacement affects the soft tissue and underlying bone.
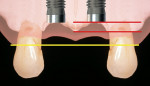
Two Single Impants
One option is to place two single implants adjacent to each other. Traditionally implants are non-scalloped or flat, coronally. This means that during placement the implant is placed apically until the platform of the implant is level with the facial crest of bone. However, because the bone is scalloped, the interproximal platform of the implant may be apical to the interproximal crest of bone by as much as 3 mm. A certain amount of bone adjacent to the implant is expected to resorb over time, usually to the first thread of the implant.12,13 As these bony changes occur, the interproximal crest of bone that was present at the time of tooth removal might resorb, resulting in a flattening of the osseous crest and a corresponding flattening of the gingival architecture as a result of the papilla losing height as the interproximal bone is lost. Several different approaches to resolving this bone loss are being researched at this time. Scalloped implants, platform switching, altered coronal implant surface design, and microgap location are just some examples of methods being used to alter the bone resorption surrounding implants. A discussion of these approaches is beyond the scope of this article, but the maintenance of the interproximal crest of bone is critical to maintaining the height of the papilla between adjacent implants. Many experts agree keeping 3 mm of space between the platforms of the adjacent implants is critical to maintaining the crest of bone.14 It is also necessary to understand what occurs to the height of the interproximal soft tissue above the bone. The research states the papilla height as being 4.5 mm above bone between adjacent teeth and bone, or 4.5 mm above the bone on the natural teeth and an adjacent implant.9 However, it appears that when adjacent implants are placed, the papilla height above the bone reduces from 4.5 mm to a range of 3 mm to 3.5 mm.14 Therefore, when adjacent implants are placed, even if they maintain the interproximal crest of bone perfectly, the papilla between the implants will be 1 mm to 1.5 mm apical to where it was between the teeth simply from the change in soft tissue levels (Figure 3). Adding this 1-mm to 1.5-mm change to any changes in interproximal crestal bone height, it becomes easy to understand why the maintenance of the papilla height between adjacent implants is difficult (Figure 4). The use of pontics rather than adjacent implants to replace the two centrals poses an interesting alternative, but one that has its own challenge.15 The facial tissue and the soft tissue between the central pontics and the lateral abutments will behave the same as when using a pontic to replace a single tooth. The challenge becomes the papilla between the adjacent pontics, just as it was between the adjacent implants. However, when pontics are used it is almost guaranteed that the interproximal crestal bone between the extracted centrals will resorb, creating a flat bony ridge and a subsequent loss of papillary height. The difference is that it is possible to augment the soft tissue between pontics significantly more above the flattened osseous crest (average 6.5 mm) as opposed to the typical tissue above interproximal bone between adjacent implants (3 mm to 3.5 mm). Ultimately it is possible to have a papilla between central pontics 3 mm more coronal than a papilla between adjacent implants for the same interproximal crest location. The purpose of this background information on the osseous and gingival response to removing multiple teeth is to make the dentist aware of the limitations of treatment before deciding upon a final course of action any time multiple anterior teeth must be lost. In addition, it provides a basis of understanding for predicting the outcome of treatment for the four most common presentations a dentist is likely to see. Each of these presentations will be reviewed. Management possibilities and the most likely compromises in the final result will be addressed. The most predictable of all presentations is the patient who needs multiple teeth removed and has no periodontal disease. The challenges in these patients are usually related to the use of implants vs. a fixed partial denture, and if implants are used, how many to use and where to place them. The answers generally depend upon which teeth are being removed. For example, if the two maxillary centrals are being removed and have good bone, placing adjacent implants can result in a predictable and esthetic final result because of the following:Pontics
Treatment Scenarios
Teeth Present
This same patient could be treated with a fixed prosthesis using the lateral incisors as abutments; but because the interproximal bone between the extracted centrals will most likely be lost, the risk of greater recession of the papilla between the centrals exists. However, soft tissue augmentation would create an excellent papilla in this location before the restoration is completed.
If the teeth to be removed involve a central and lateral or a lateral and cuspid, the treatment choices are not quite as clean cut. It is very difficult to place adjacent implants in a central and lateral position, or a lateral and cuspid position, and have 3 mm between the platform of the implants. This leaves a high risk of losing the interproximal crest of bone between the implants over time with subsequent loss of papillary height (Figure 10, Figure 11, Figure 12, Figure 13). Papillary height might be lost between the central and lateral on one side while natural teeth still exist on the other. The discrepancy in papilla heights is much more noticeable than a slight loss of papilla height between adjacent central incisor implants. Also, using adjacent implants to replace a central and lateral or lateral and cuspid is unnecessary because of the lower occlusal forces in the anterior. The author almost always chooses to cantilever the lateral incisor off of a single central implant or a single cuspid implant because it is esthetically more predictable and as functionally as acceptable as adjacent implants.
Another option for the missing central and lateral or missing lateral and cuspid is the use of soft tissue augmentation and a fixed prosthesis. Whereas this can create a pleasing esthetic result, it is a more complex restoration structurally, especially when replacing the lateral and a cuspid with pontics.
When three or four adjacent anterior teeth with good periodontal support need to be removed, the author prefers to separate them by one or two pontics. For this reason, if both centrals and a lateral need to be removed, the author places a central implant, central pontic, and lateral implant. This design allows excellent papilla heights in all locations owing to the predictability of the soft tissue augmentation in the pontic site (Figure 14, Figure 15, Figure 16, Figure 17, Figure 18). If all four incisors need to be removed and good periodontal support exists, there are two acceptable options. One is to place implants in both lateral incisor locations and use both centrals as pontics. The other is to place the implants in both central locations and cantilever the lateral incisor pontics. Both options will produce acceptable esthetic and structural results.
If the same scenarios are presented but the teeth have pre-existing bone loss, new challenges exist. Specifically, the papilla height in the areas of the periodontal disease becomes less predictable following tooth removal. This often leads to a greater degree of papillary recession and a more apically placed contact in the restorations to avoid an open gingival embrasure. In these situations the dentist is faced with the choice of using implant restorations that will be functionally and structurally acceptable, but esthetically less attractive, or using soft tissue grafting and fixed partial dentures where the ability of grafting and the use of pontics can produce significantly more soft tissue over the interproximal bone—3.5 mm between adjacent implants vs 6.5 mm above bone for pontics. As a rule the decision is based upon the esthetic needs of the patient (ie, high lip line vs the condition of the teeth). If the adjacent teeth are unrestored, it might still be preferable to use the implants rather than prepare the unrestored teeth and live with some esthetic compromise.
The other option to consider is slow orthodontic eruption before extraction.16 The eruption of a single tooth to be extracted does not alter the final papilla heights because they are dictated by the bone on the adjacent teeth. When multiple teeth are erupted before extraction, it is possible, but not always predictable, to move the interproximal bone coronally. However, it is critical to apprise the patient that a perfect esthetic result is unlikely, and that short papilla, long contacts, and more rectangular looking final restorations could be expected (Figure 19, Figure 20, Figure 21, Figure 22, Figure 23, Figure 24).
Teeth Missing
The next two presentations are the most difficult to manage esthetically because in both cases the teeth have already been removed. When this happens, the bony ridge tends to flatten rapidly unless something is done to alter the process. In cases where the teeth have been missing for a significant period of time, the interproximal crest of bone is completely gone. Vertical bone augmentation to re-create the interproximal crest is very difficult and unpredictable. Therefore using adjacent implants always ends up with an inadequate papillary height. However, using a connective graft and pontics can create and maintain significantly more soft tissue above the interproximal bone than is possible with adjacent implants. Because of this, the patient must be informed that the best esthetic result may involve pontics rather than implants. Using connective tissue grafting and a pontic next to implants, however, can create an excellent result (Figure 25, Figure 26, Figure 27, Figure 28).
The most difficult of all the scenarios to manage esthetically is when the teeth are missing and a significant ridge defect exists. In these cases there is a logical tendency to use bone grafting followed by soft tissue grafting to correct the situation. Realistically there are limitations in both techniques as to how much vertical augmentation is possible. It is possible for the patient to go through multiple surgical procedures and still end up with a result that is significantly deficient in the correct soft tissue levels. Ultimately, this places the restorative dentist in a difficult position as the use of conventional fixed restorations may result in a less-than-adequate esthetic result. The accepted solutions are to use pink porcelain to replace the missing gingiva on a fixed restoration or to use a removable prostheses or a fixed restoration with a removable gingival mask (Figure 29 and Figure 30).
The challenge of using the pink porcelain and removable prosthesis or removable gingival mask is to hide the junction of the artificial gingiva and the ridge in a high smile. Anytime a significant ridge deformity exists, it is critical to assess two things: does the existing ridge show in a high smile, and if it is augmented, can the augmentation be successful at eliminating the need for prosthetic gingival replacement? If the ridge doesn’t show currently in a high smile, and the augmentation can’t eliminate the need for prosthetic gingival replacement, it may be far more esthetic to not augment the ridge at all and keep the junction of the prosthetic gingiva and ridge under the high lip line rather than risk the augmentation, which should make that junction visible.
Conclusion
Because the outcome can be so variable when treating multiple missing teeth, it is critical that the treating dentists and the patient are clear about what can be realistically expected and what changes may need to be made in the plan dependent upon the outcome of each phase of treatment. This allows the patient and clinician to proceed with a clear understanding of the potential complications and financial costs of treating these clinically challenging but highly rewarding situations.
Acknowledgment
The author would like to thank Greggory Kinzer, DDS, MSD, and Bobby Butler, DDS, MSD, for Figures 5 through 9; David Mathews, DDD, Vince Kokich, DDS, MDS, and Barret Rochefort, DDS, MSD, for Figures 19 through 24; and David Mathews and Roger Lawton, DDS, for Figure 25 through Figure 28.
References
1. Choquet V, Hermans M, Adriaenssens P,et al. Clinical and radiographic evidence of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontal. 2001;72(10):1364-1371.
2. Grunder U. Stability of the mucosal topography around single-tooth implants and adjacent teeth: 1-year results. Int J Periodontics Restorative Dent. 2000;20(1):11-17.
3. Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: An evaluation of maxillary anterior single implants in humans. J Periodontal. 2003;74(4):557-562.
4. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995-996.
5. van der Velden U. Regeneration of the interdental soft tissue following denudation procedures. J Clin Periodont. 1982;9(6):455-459.
6. Kois JC. Predictable single-tooth peri-implant esthetics; five diagnostic keys. Compend Contin Educ Dent. 2004;25(11):895-898.
7. Smukler H, Castellucci F, Capri D. The role of the implant housing in obtaining esthetics: generation of peri-implant and papillae- Part 1. Pract Proced Aesthet Dent. 2003;15(2);141-149.
8. Mathews DP. Soft tissue management around implants in the esthetic zone. Int J Periodontics Restorative Dent.2000;20(2):141-149.
9. Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: A guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998;10(9):1131-1141.
10. Elian N, Jalbout ZN, Cho SC, Froum S, Tarnow DP. Realities and limitations in the management of the interdental papilla between implants: Three case reports. Pract Proced Aesthet Dent. 2003;15(10);737-744.
11. Saadoun AP, Le Gall MG, Touati B. Current trends in implantology: Part II- Treatment planning, aesthetic considerations, and tissue regeneration. Pract Proced Aesthet Dent. 2004;16(10):707-714.
12. Hermann JS, Cochran DL, Nummikoski PV, Buser D. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol.1997;68(11)1117-1130.
13. Hermann JS, Buser D, Scenk RK, Cochran DL. Crestal bone changes around titanium implants. A histometric evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol. 2000;71(9):1412-1424.
14. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
15. Spear FM. Maintenance of the interdental papilla following anterior tooth removal. Pract Periodontics Aesthet Dent. 1999;11(1):21-28.
16. Salama H, Salama M, Kelly J. The orthodontic-periodontal connection in implant site development. Pract Periodontics Aesthet Dent.1996;8(9):923-932.
About the Author
Frank M. Spear, DDS, MSD
Founder and Director, Seattle Institute for Advanced Dental Education
Seattle, Washington
Affiliate Assistant Professor, University of Washington School of Dentistry
Seattle, Washington
Private Practice
Seattle, Washington