The Future of Complete Denture Prosthetics
Creating stability and maintaining age-appropriate esthetics.
By Robert Kreyer, CDT; and Brian Carson, CDT
The future of any profession or industry depends on a properly trained or educated young domestic workforce. This is especially true in dental laboratory technology, because the majority of dental laboratory owners specializing in removable prosthetics in North America are over the age of 55. It is important to mentor the technicians that have a true passion for prosthetic dentistry in order to ensure the future of technical removable prosthetics in North America.
In this removable prosthetic column, I would like to introduce Brian Carson, CDT. Brian, a young dental laboratory owner specializing in removable prosthetics, possesses the passion, persistence, and perseverance needed in dental laboratory technology in the future. In his article, Brian Carson’s technique illustrates the direction in which complete denture prosthetics is going in regards to esthetics and functional occlusion.
Introduction
Implant-retained options for ill-fitting and loose mandibular prostheses are now more affordable and are becoming a widely accepted treatment alternative for patients. However, as the popularity of implant-retained dentures grows, this treatment option can cause unexpected pitfalls for the technician. In order to achieve the desired successful outcomes from implant-retained prostheses, communication is vital. Photography is the simplest, yet most overlooked, communication tool. Images showing the patient prior to implant placement as well as during the various restorative stages of treatment allow the technician to identify and focus on the desired expectations of both the patient and dental team in completing the case. Including photography in the laboratory operating guide increases the effectiveness of the final product and promotes a technician’s unique skill set.
Case Overview
The patient presented with several complaints about his maxillary/mandibular complete prosthesis. The two issues mentioned most often were instability and anterior dislodgement of the maxillary prosthesis, with uncomfortable pressure in the areas of teeth Nos. 10 and 11. The patient also expressed dissatisfaction with the current overall look of the denture and its “fangy” appearance (Figure 1).
When a patient presents with base instability, process bases are an excellent choice. The denture base is processed in the final acrylic, thus giving the patient a defining glimpse of the fit before the final delivery. The technique allows the patient and the clinician time to evaluate fit during both the bite registration and tooth try-in phases. Reverse engineering in this manner is a fantastic deductive tool and conversation starter about the need for a more advanced treatment option.
With this particular case, work was started on both dental arches using the process base method (Figure 2). The mandibular denture was retained with two locator implants (Figure 3). To help eliminate any possible issues, the locator housing was processed directly before the bite registration, so access holes were created in the base.
As with this case and most implant-retained lower denture cases, there were no mandibular ridges. Therefore, due to the high likelihood of impression anomalies and of creating discrepancies while adjusting the base at delivery, laboratory processing of the locator housings should be avoided. Employing this technique early allowed a solid foundation to be created before any other work was performed. When following this technique, the clinician physically maintained contact until the locator housing was set (Figure 4). By activating the locator housing before final delivery, accuracy of the final denture was increased due to the lack of tooth interference when the patient bit the base into place.
Next, the bite rims were created. Vanilla pre-fabricated rims (Schutz Dental, www.schutz-dental.com) were employed to increase clinician/technician communication. The contrasting color serves well for this application. Using this technique and material, clear delineation was obtained between the patient’s facial and oral features, greatly helping to establish proper anterior tooth placement (Figure 5 and Figure 6).
After registration and repeatable closure were verified, working casts were created and all information was transferred to the articulator (Figure 7). After reviewing the clinical information provided and comparing it to the case on the articulator, it was assumed that the initial occlusal scheme with the current denture would exacerbate the combination syndrome (Figure 8). The combination syndrome is associated with cases where the maxillary is opposing a solid foundation, as in natural dentition, or in this case, implant-retained. The most certain solution is using implants in the maxillary. However, when this is not an option, proper tooth placement for directing the forces at a 90° angle to the ridge or an area of support assists in managing this condition for the patient. In this case, the lower anteriors were in direct contact with the opposing anteriors. Notice the maxillary six and the flaring (Figure 9). Not only was this not a natural emergence profile, but with the lower six in direct occlusion, it also created a hammering and pushing effect, which is a recipe for dislodgement.
Upon further assessment on the articulator, it was apparent the case presented with ridges less than 80° of alignment. This relationship dictated setting the occlusion in a crossbite (Figure 10). By setting the maxillary anterior teeth with the proper emergence profile and setting the appropriate posterior teeth in a pre-determined location, it was now possible to begin building a solid foundation (Figure 11).
To garner the most advantageous position for the posterior teeth, the Palameter (Heraeus Kulzer, www.heraeus-kulzer.com) was used. This is an excellent means of determining the placement of the mandibular first molar in conjunction with the descending arm of the ramus (Figure 12). In this case, no teeth were used past the mandibular first molar. Doing this helped eliminate any pushing or forward thrusting during closure, which is very important in managing the combination syndrome associated with the maxilla (Figure 13 and Figure 14). Illustrations published in the 1972 and 1979 issues of the Journal of Prosthetic Dentistry1,2 showed the similarity between forces of natural anterior teeth compared to an implant-retained prosthesis with anterior abutments. The similarities between a tooth-retained and implant-retained denture include the loss of vertical dimension, occlusal plane discrepancy, and poor adaptation of the maxillary complete denture prosthesis.
The anterior teeth were set in almost an end-to-end fashion, thus removing the current hammering and pushing effect by the current denture (Figure 15).
The patient interview had revealed the desire for a less “denture look” and more of a natural age- appropriate design to include a more realistic shade. Creaperal (Jensen Dental, www.jensendental.com) teeth in shade C1 were used along with individual modification and coloring using Lite Art Color Pastes (Shofu Dental, www.shofu.com) (Figure 16 and Figure 17).
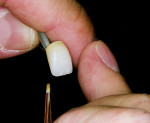
Modification was made very simple with the color pastes. (The author recommends creating a mental visual of the end result before starting.) Modifying the teeth before setting is the cleanest and yields the most natural appearance. For optimal results in bonding, it is recommended to lightly air-abrade the surface with aluminum oxide (Figure 18). Recontouring the tooth and creating the desired surface texture and incisal character was then performed. The author prefers using a small-diameter diamond at a very low speed (Figure 19). In nature, the older the patient is, the more muted and slick the surface texture becomes near the incisal edges. Wear and chips created by modification should follow the pattern of the opposing teeth. This also relates to any twisting or individualization of tooth position.
After steaming and cleaning the prepared tooth surface, a bonder is used to cure the pastes in accordance with manufacturer’s specifications. The bonder used in this application was primoStick (Primotec, www.primogroup.net); it was cured for 10 minutes (Figure 20). The color paste of choice should then be selected. In this case, a small amount of white was used to create decalcification and craze lines, and then was cured for a 1-minute cycle (Figure 21). The khaki paste was then used around the cervical and interproximal areas and cured for a 1-minute cycle, followed by a small application of blue gray to give the appearance of translucency. This was cured for a 1-minute cycle as well. For optimum results, each color step should be performed in liberal increments, until the desired effect is achieved. Finally primoglaze (Primotec, www.primogroup.net) should be used to seal the surface (Figure 22). This extra value-added step increases the personalization of the denture teeth (Figure 23 and Figure 24).
Conclusion
In today’s evolving nature, it is paramount to increase knowledge and skill while keeping up with technology. By always seeking to leave the clinician and patient feeling elevated, dental laboratory technicians can secure their place in the constantly changing landscape of dental technology.
Acknowledgment
Clinical photography is courtesy of Dr. David Hall, DDS.
References
1. Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 1972;27(2):140-150.
2. Saunders TR, Gillis Jr RE, Desjardins RP. The maxillary complete denture opposing the mandibular bilateral distal-extension partial denture: treatment considerations. J Prosthet Dent. 1979;41(2):124-128.
About the Authors
Robert Kreyer, CDT
Director of Removable Prosthodontics
Microdental/DTI
Dublin, California
Brian Carson, CDT
Owner
Signature Dental Lab
Fayetteville, North Carolina