You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
A 73-year-old woman presented with a complete upper denture fabricated more than 15 years prior and a lower partial denture made within the past 5 years. Her chief desires were a more esthetic look unlike her existing worn denture teeth; wanting to show more teeth in her smile; "a better fit," which equated to more retention; and to chew better.
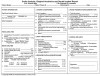
An examination revealed that her maxilla had lost a significant amount of bony support, leaving a relatively flat ridge along with a very small vestibular space. The ridge was especially resorbed in the anterior region due to her lower supra-erupted teeth. The teeth had an uneven occlusal plane (Figure 1) and were monoplane in design.
The lower partial fit well, but the alignment of her lower right posterior teeth was off the occlusal plane and based on the occlusion of her upper denture. Her vertical dimension was slightly over-closed.
Clinical Procedure
Using the Pala Digital Dentures process and tools (Heraeus Kulzer, heraeus-kulzer-us.com), the clinician took all necessary impressions and records in one visit, filled out the Pala prescription, and sent it to the laboratory. In this case, the clinician wrote on the prescription that they would be raising the lower right teeth on the partial to create the ideal occlusal plane for the upper denture. The lingualized occlusion option with 20° teeth was selected.
The dentist had the choice of requesting a 3D printed full model or a 3D printed model of the base with a waxup of the teeth, and the latter was selected. This way, the dentist and patient could select the tooth color at the initial appointment and have the teeth set-up on the same 3D model for the try-in appointment to confirm the tooth color and also, if needed, to modify the setup or the occlusion at this appointment. In this case, the clinician decided to adjust the occlusion with a new wax bite.
At the try-in appointment, a pickup impression of the lower partial was taken, such that the laboratory could raise the lower right teeth on the partial to match the prescribed ideal occlusion for the upper prosthesis from the first appointment.
Laboratory Procedures
Upon receipt of the case, the laboratory technician read the prescription thoroughly and scanned the impressions and bite registration with a 3Shape D800 scanner (3shape.com). The resulting STL files were sent to the Pala centralized manufacturing facility for the design and fabrication of a 3D printed prototype.
The unique, proprietary software allowed the CAD designer to determine tooth position based on the data from the scanned impressions, registrations, and lip measurements. This further reduced clinical appointment time by eliminating many of the traditional record achievements normally required.
The remaining determinations were derived from the algorithms in the software. Twenty-six anatomical landmarks found in every patient were used, including the incisive papilla, midline suture, fovea palatine, and retromolar pads. The measurements associated with occlusion rims illustrated the application of these "anthropometric averages." The design was accomplished from these accumulative data points as seen in Figure 2.
Historically, milling has been the most common production technology associated with the fabrication of dental restorations. We are entering the next phase of technology adaptation, involving 3D printing for production purposes. This additive method is recognized in general manufacturing to be more productive and less wasteful than subtractive technology, but it has been significantly more expensive until recently.
Only one denture base resin is currently available with the required FDA 510(k) clearance for definitive clinical use, however, the author’s testing to this point has found it to be esthetically unacceptable.
Based on these findings, Hereaus Kulzer chose to 3D print a fully contoured prototype for the clinical try-in to streamline the fabrication process, bringing the 3D printing advantage to the marketplace.
The curing shrinkage associated with this particular printer and material combination results in less than 1% polymerization shrinkage, assuring an excellent fit.
The prototype was then converted to a functional prototype (stabilized wax prototype), utilizing the highly accurate printed base fitted with wax-attached Mondial prosthetic teeth (Heraeus Kulzer). The functional prototype was sent to the laboratory for evaluation and delivery to the clinician (Figure 3).
This hybrid offering is unique within the digital denture category. It allows the clinician to manage the case as usual by refining anterior tooth position and, where indicated, take a check bite for occlusal refinements by the laboratory technician. This maintains and preserves the original laboratory/client relationship.
Upon achieving a satisfactory try-in, the case was returned to the centralized manufacturing facility for completion. The usual shades of methyl methacrylate resin were available for processing with a proprietary injection method, ensuring minimal polymerization shrinkage and a superior clinical fit.
Conclusion
The final delivery required no adjustments on the flanges and the retention was excellent. There were slight adjustments to refine centric occlusion on the bicuspids and to teeth Nos. 9 through 11 to harmonize the excursive function (Figure 4). The final denture can be seen in Figure 5.
The Pala Digital Dentures system allowed the practitioner to deliver a fully edentulous prosthesis in three appointments. Without the need for custom trays, multiple visits were saved as the clinician took the final impression, recorded the VDO, captured the bite, took an excellent gothic arch tracing, and measured the length of the teeth in a truly streamlined process.
The process also empowered the dental laboratory to produce complete dentures with improved quality, especially with regard to fit. From a business perspective, it allows laboratories to increase capacity without the need for any additional labor or associated overhead.
The system also provides a backup when situations arise that affect the laboratory's production capacity, ie, unforeseen turnover, a big influx of cases, vacation schedules, or illness. Meanwhile, it allows small to medium-sized fixed laboratories to enter the growing removable space.
The ultimate benefactor is the patient. The reduction in chair time improves the overall treatment experience, and the excellent fit ensures functionality and confidence.