Redefining What Is Possible
Treating function and enhancing esthetics using a risk management system
Kris Swanson, DDS; and Leon Hermanides, CDT
When a patient presents to a practice with concerns of an uncomfortable bite, joint pain, and a feeling that she needs to squeeze to get her teeth together, dentists are often inclined to rush to complete treatment on these multiple complex problems. This can lead to frustration as well as inconsistent and unpredictable treatment outcomes.
The authors utilized the systematic approach taught at the Kois Center1,2 to treat a patient with those concerns. This patient's uncomfortable bite was addressed, increasing her trust in the clinician as well as motivating her to treat her esthetic issues. Because treating the patient's constricted chewing pattern (CCP) would involve treating her posterior teeth in an adapted centric position, the uneven visual crown height of the posterior teeth was addressed. The technique utilized involved recontouring the abutments and implant restorations to increase the visual length of the teeth. Collaboration between the clinician and the laboratory technician was vital in creating a clear vision of the desired outcome.
Clinical Case Overview
A 64-year-old former dental assistant (Figure 1) was referred to the dental office, which was more than 700 miles from her home, so the treatment phasing was adjusted to accommodate her travel schedule. Her dental history included orthodontics at age 52, and she reported bite/temporomandibular disorder (TMD) issues occurring after additional extensive dental treatment. She had become increasingly unhappy with her smile (Figure 2). She was concerned about the black triangles between her lower anterior teeth and the uneven gingival margin positions of her posterior implant restorations. Her maxillary anterior teeth were previously restored with large Class III composites, which had become worn and chipped. She was worried about breaking her front teeth and wanted something more permanent than repairing them with direct composite bonding (Figure 3 and Figure 4).
Medical and Dental History
The patient's medical history included an underactive thyroid, acid reflux, and Type II diabetes (A1C 5.7), all of which were controlled with medication. She had received regular dental care and had a family history of periodontal disease. She had a history of broken and/or chipped teeth, but no active decay in the past 3 years.
Diagnosis, Risk Assessment, and Prognosis
The patient's periodontal diagnosis was Stage II Grade B, a moderate risk with a fair prognosis.3 Some isolated pockets were found on the molar implants. No active caries were noted. Teeth Nos. 7 through 11 had a fair prognosis due to existing large composite fillings. Teeth Nos. 4 and 5 had a poor prognosis as they were structurally compromised and had previously received root canal treatment. Her biomechanical risk was moderate, and her prognosis was fair.
The patient reported soreness and bilateral popping of her temporomandibular joint (TMJ) but had no clicking or locking. She avoided many foods due to fear of breaking teeth. Over the past 5 years, she noticed that her upper and lower anterior teeth had become shorter and that she now hit harder on her anterior teeth than in the posterior. She reported having to squeeze to make her teeth fit together and was aware of daytime and nighttime clenching. She had worn a nightguard for many years. The diagnosis of her occlusion was a CCP.4 This presents as a moderate risk with a poor prognosis.
The patient had visible gingival display in both her natural and Duchenne smile. The maxillary anterior teeth had acceptable gingival symmetry and were in an acceptable position. As she wanted to recreate the smile she used to have and not a smile she never had, this simplified her treatment. Her prognosis was therefore modified from hopeless to poor; however, this situation is considered a high esthetic risk due to the visible tooth display.
Treatment Goals
The treatment goals were to achieve the patient's vision of a more harmonious smile without increasing the structural risk to the teeth, and to fabricate long-lasting, functional restorations. A repeatable mandibular position would be determined using a deprogramming appliance (Kois Deprogrammer, Kois Center),5 and then the teeth would be restored with the mandible in the deprogrammed condylar position. The facial contour of the maxillary posterior implant restorations would be altered to harmonize with the gingival levels of the anterior teeth.
Pretreatment Consultation and Deprogramming
After the initial examination, a 3D printed deprogramming appliance was fabricated by the dental laboratory, and the patient returned for delivery and to discuss treatment options. The final treatment plan would be confirmed after deprogramming and subsequent bite registration. The treatment included opening the vertical dimension of occlusion (VDO) by restoring her posterior teeth. This would relieve the CCP, allowing the upper anterior teeth to be lengthened. Due to her concern about the existing large Class III maxillary anterior composites, the patient requested indirect restorations for the maxillary anterior teeth. To accommodate the patient's esthetic concerns, the mandibular anterior teeth would be bleached. She was instructed to wear the deprogramming appliance at all times, except when eating.
After wearing the appliance for 3 weeks, the patient returned, and occlusal records were obtained. She reported joint comfort and being free of pain when wearing the appliance. A dento-facial analysis tool (Kois Dento-Facial Analyzer, Kois Center) was used to mount the upper cast, and the deprogrammed bite record was used to articulate the lower cast on an articulator (Panadent). The point of initial occlusal contact was on the anterior teeth, confirming the diagnosis of CCP.
Finalized Treatment Plan
A diagnostic wax-up would be fabricated using the Kois 10 Step Treatment approach.1 With lips in repose, the cuspid display was -1 mm; therefore, 1.5 mm was added to the cuspid length, and the upper arch was leveled.6 To harmonize with the anterior teeth, the maxillary posterior teeth would be lengthened apically approximately 1 mm to 3 mm. The mandibular teeth would be leveled to the length of tooth No. 23.
Indirect restorations would be placed on teeth Nos. 4 through 6, 7 through 11, and 29; custom abutment-supported implant crowns would be placed on teeth Nos. 3, 19, 20, 30, and 31; and a custom abutment-supported implant bridge would be placed on teeth Nos. 12 through 14. Direct composite restorations would be placed on the occlusal surfaces of teeth Nos. 21 and 28 and the incisal edges of Nos. 22 through 27. Additionally, composite would be placed interproximally to close the black triangles in the gingival third of teeth Nos. 22 through 27.7 The VDO would be opened approximately 1 mm to flatten the chewing pathway and allow for longer maxillary anterior teeth.8 The inappropriate visual coronal length in the upper left would be addressed with tissue alteration around implant abutments and an ovate pontic site to give a more symmetrical and pleasing smile. The patient would receive routine periodontal maintenance care from her local dentist.
Maxillary Arch
Teeth Nos. 4, 5, and 7 through 10 were prepared for conservative full-coverage restorations, while teeth Nos. 6 and 11 were prepared for partial-coverage restorations. The implant restorations on teeth Nos. 2 and 3 and the upper-left implant-supported bridge were removed, open-tray impression copings were placed, and a polyvinyl siloxane (PVS) impression was taken.
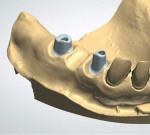
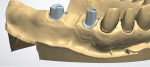
Upper provisional restorations were fabricated from the diagnostic wax-up using a PVS matrix, with the posteriors retained on temporary abutments.9 The posterior crowns would be fabricated from layered zirconia for strength and opacity to block out the underlying metal abutments. The anterior crowns would be lithium disilicate due to the enhanced esthetic quality of that material. The visual length of the maxillary implant teeth was determined in the laboratory first (Figure 6 through Figure 10), with the clinical gingival management done at the seat appointment. Slight occlusal adjustment was needed on the mandibular arch to create bilateral equal posterior contact in occlusion. The patient returned the following day for impressions of the provisional restorations and photographs, and to obtain centric occlusion records. The record was taken by creating a small direct composite deprogrammer on the palatal surface of teeth Nos. 8 and 9, opening the bite 0.5 mm.10 The maxillary posterior provisional restorations were removed, tall healing caps were placed in the implants, and a bite registration was taken. Healing caps were removed and sent with the case to the laboratory for mounting.
The patient returned 1 month later to seat maxillary restorations. To allow for complete seating of the abutments and restorations, gingival tissue recontouring in the upper left was completed before restoration try-in. After anesthesia was administered, the cover screws were placed to protect the implants. Additional anesthetic was infiltrated around the implant and pontic sites to help with pain management and control bleeding. After evaluation of the implant and pontic sites on the working model, a diamond bur (KS5 FG Super Coarse Football Diamond 35010.31.005, Brasseler USA) was used to alter the tissue and allow passive seating of the custom abutments and implant restorations (Figure 11). Radiographs confirmed complete seating of the implant components prior to cementation.
All restorations were then evaluated for esthetics, complete seating, occlusion, and proximal contacts. The patient was seated upright to view the new restorations. She was overjoyed and gave approval for permanent seating. Teeth were microetched using 27-µm aluminum oxide, and implant abutments were torqued to 35 Ncm. The lithium disilicate crowns on teeth Nos. 6 through 11 were cleaned, silanated, and seated cohesively using a self-adhesive resin cement (RelyX™ Unicem 2, 3M Oral Care). The maxillary posterior zirconia crowns were microetched, cleaned, primed with MDP monomer (Z-Prime™, BISCO), and seated cohesively on teeth Nos. 4 and 5 and the custom implant abutments. An occlusal adjustment using a printed deprogramming appliance was completed to refine the occlusion on the mandibular arch.
Mandibular arch
The mandibular arch was treated the next day. The occlusal and incisal edges of teeth Nos. 21 through 28 were restored with direct bonding, guided by the diagnostic wax-up. A polyvinyl lingual matrix was used to add microhybrid composite (A1 Vit-l-escence™, Ultradent) to the incisal edges of teeth Nos. 22 through 27. The black triangles in the anterior were bonded and closed using a technique the clinician developed,7 utilizing an anterior matrix (Blue View™ VariStrip™, Garrison Dental) with a built-in curvature that facilitates ideal interproximal contours and marginal adaptation. Tooth No. 29 was prepared and an open-tray PVS impression was taken for custom abutments and implant crowns on teeth Nos. 19, 20, 30 and 31, and for a crown on tooth No. 29. Mandibular provisionals were fabricated from the diagnostic wax-up using a PVS matrix and temporary abutments. The printed deprogramming appliance was inserted and a new centric bite was taken with the bite opened approximately 0.5 mm; the posterior provisionals were removed and healing caps were placed. The provisional restorations were seated, and healing caps were sent to the laboratory to facilitate mounting the case accurately.
The patient returned 3 weeks later for seating of the lower restorations. The same protocols used for the cementation of the maxillary crowns were followed. A deprogramming appliance was used again to refine the occlusion and achieve equal bilateral simultaneous contact. The patient was seated upright and asked to chew on 220-µm paper, and all the chewing interferences were removed in the envelope of function.
Postoperative Check and Final Photographs
The patient returned 1 month after completing treatment for a postoperative examination and to have final photographs taken. She was thrilled with the comfort of her new bite and her beautiful smile (Figure 12 through Figure 17).
Discussion
A patient with a history of significant dental treatment sought a solution for her worsening symptoms due to an uncomfortable bite and jaw pain. For the patient, the ongoing pain in her jaw joints and her concerns for the fracture or loss of her anterior teeth were driving the treatment. However, her experience with the deprogramming appliance and the relief of her symptoms enhanced her trust in the restorative team to adequately restore her to functional and esthetic harmony.
Once the mounted casts were articulated with the deprogrammed occlusal records, it was determined that replacement of the maxillary and mandibular posterior restorations would be required to restore a bilateral simultaneous occlusion. This would also allow the posterior maxillary implants to be restored to a visible tooth length more harmonious with the gingival levels and length of the maxillary anterior teeth.
From the diagnostic mounting, a blueprint of the final restorations was generated to guide the patient's treatment decisions and create matrices for the provisional restorations. In the dental laboratory, a soft-tissue model was poured to replicate the patient's clinical situation. Before designing the custom milled abutments, and with the diagnostic cast as a reference, the dental technician was able to alter the soft-tissue coronal to the implant fixture (Figure 6 through Figure 8). Preparing the tissue prior to 3D scanning for the abutment design made it possible to control the emergence and create more visible tooth structure (Figure 9 and Figure 10), harmonizing with the gingival position of the anterior teeth and addressing the patient's concern with the visible length of the restorations.11
Though tissue management would have been possible during the provisional phase, consideration was given to the restraints of treating a patient from out of state; reducing chair time and achieving a more predictable outcome were prioritized. This choice required no esthetic or biological compromise in the final treatment outcome.
Conclusion
Addressing the patient's chief concern—her joint pain—motivated her to focus more comprehensively on her goals for dental treatment. Despite restorations being replaced multiple times, her symptoms continued to worsen, and her esthetic expectations had not been met. In managing her risk profile and esthetic concerns, a systemic approach to diagnosis and treatment planning was vital in creating and implementing the vision of what was possible.
About the Authors
Kris Swanson, DDS
Mentor
Kois Center
Seattle, WA
Private Practice
Swanson Dental Associates
Bellevue, WA
Leon Hermanides, CDT
Clinical Instructor and Scientific Advisor
Kois Center
Seattle, WA
Founder
Protea Dental Studio
Redmond, WA
References
1. Kois JC. New challenges in treatment planning: incorporating the fundamentals of patient risk assesment - Part 2. J Cosmetic Dent. 2011;21(1):110-121.
2.Kois JC. New challenges in treatment planning: shifting the paradigm toward risk assesment and percieved value - Part 1. J Cosmetic Dent. 2011;26(4):62-69.
3. Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89 suppl 1:S159-S172.
4. Huff C. A systematic method for accurate functional diagnosis. Compend Contin Educ Dent. 2017;38(5):308-316.
5. Revilla-León M, Zeitler JM, Kois DE, Kois JC. Utilizing an additively manufactured Kois deprogrammer to record centric relation: a simplified workflow and delivery technique. J Prosthet Dent. 2022;S0022-3913(22)00364-X. doi: 10.1016/j.prosdent.2022.04.034.
6. Misch CE. Guidelines for maxillary incisal edge position - a pilot study: the key is the canine. J Prosthodont. 2008;17(2):130-134.
7. Swanson KK. Predictable, conservative closure of black triangles. Inside Dentistry. 2018;14(12):32-38.
8.Kois JC, Phillips KM. Occlusal vertical dimension: alteration concerns. Compend Contin Educ Dent. 1997;18(12):1169-1177.
9. Kois DE, Schmidt KK, Raigrodski AJ. Esthetic templates for complex restorative cases: rationale and management. J Esthet Restor Dent. 2008;20(4):239-250.
10. Solow RA. The anterior acrylic resin platform and centric relation verification: a clinical report. J Prosthet Dent. 1999;81(3):255-257.
11. Phillips K, Kois JC. Aesthetic peri-implant site development. The restorative connection. Dent Clin North Am. 1998;42(1):57-70.