Interdisciplinary Treatment in an Esthetically Challenging Case
Fabricating a screw-retained PFM for an anterior implant following complex orthodontic treatment
Sergio Rubinstein, DDS; Barry P. Levin, DMD; Elizabeth R. Michalczyk, DMD, PhD; Yan Razdolsky, DDS; and Toshiyuki Fujiki, RDT
Often providing a first impression about someone, a person's smile can be a personal trademark that both serves as a means of communication and is indicative of the individual's self-confidence. A smile plays an integral role in psychological-social well-being and emotional health.1-5 Therefore, many people wish to modify their smiles, and this presents dentists with a number of considerations when planning patient care. Should the treatment be conservative or invasive? Are there physical and/or emotional limitations to achieving the desired goals? What treatment options are available? What will the length of time and cost be to complete the treatment? Oftentimes a treatment can become quite complex, and to accommodate such cases an interdisciplinary approach from the outset may be needed to provide patients the best, most efficient care.
In the clinical case presented, poor planning and execution had led to inferior orthodontic treatment, which needed to be salvaged. A new, interdisciplinary esthetic-prosthetic management plan was put into effect to achieve a successful result from the standpoint of both oral health and an esthetically pleasing smile. This case is representative of many others like it that require careful consideration for the cosmetic challenges of treating anterior teeth, and for how treatment modalities and outcomes can vary depending on the all-important surrounding frame: the gingivae.
Clinical Case
A 7-year-old patient presented to the orthodontist in 2002 with a congenitally missing maxillary left central incisor (Figure 1). The patient underwent orthodontic treatment for 6 years that resulted in an unacceptable smile and compromised state for future restorative/prosthetic outcome, as the right central incisor had been moved into the patient's midline (Figure 2). Additionally, the patient's improper course of treatment and unsatisfactory progress resulted in lost time during growth as well as the expenditure of considerable finances. Because of the complexity of the case, other dental disciplines should have been included in the treatment planning and care from the outset but were not.
Referral to Prosthodontist
The orthodontist referred the patient to the prosthodontist (the author, SR) for a consultation to determine how an esthetic outcome could be achieved. The prosthodontist attempted to rectify the improper course of treatment while working with the orthodontist; however, it eventually became apparent to the prosthodontist that a new interdisciplinary team would be needed. Despite the prosthodontist's guidance, poor orthodontic mechanics and improper anchorage execution had led to excessive buccal flaring (Figure 3). Although temporary, overarch expansion during the orthodontic treatment had created an unacceptable cosmetic situation for the now 14-year-old boy, with an extreme edentulous space having been created in the area of the left central incisor. This led to psychological-social concerns for the patient such as shyness, introversion, and being uncomfortable smiling.
To address the situation, with the congenitally missing tooth being the maxillary left central incisor and the orthodontically moved adjacent teeth now being in improper positions, the prosthodontist deemed it necessary to extract the maxillary left first premolar to create the necessary space for the upper left central incisor future implant and crown. A short-term esthetic solution was implemented by bonding a denture tooth using an orthodontic wire on the palatal surface of the right central incisor. This procedure slightly improved the cosmetic concern (excessive diastema) and served as a helpful guide for the original orthodontist by providing the correct width needed to close the large existing space. In this instance, an extreme concave buccal contour on the maxillary right central incisor was diagnosed, and it was determined that the final restoration of this tooth would be conservatively addressed with either direct bonding or a porcelain veneer.
Space closure for the missing central incisor and improved esthetics were achieved, but the anterior teeth had an undesirable and unacceptable buccal flaring (Figure 4).
New Orthodontist Brought in
At this point the prosthodontist made referrals to a new orthodontist and a periodontist in anticipation of achieving a satisfactory outcome. The prosthodontist presented the patient and parent with a new treatment plan. The plan, developed by the newly formed interdisciplinary team, was predicated on repositioning the patient's teeth into their proper locations and allowing for the replacement of the missing left central incisor with an implant and implant-supported crown. This, the team determined, would lead to an esthetic, healthy, and long-lasting result.
Anatomical evaluation of adjacent teeth and hard and soft tissue should be considered at early stages of therapy, in the authors' opinion, because this can alter the sequence of treatment for the replacement of missing teeth. In this case, as can be seen in Figure 3, it was clinically evident that the missing tooth was associated with a deficient alveolar ridge, and bone grafting would be required for the placement of an implant and to improve esthetics. As treatment progressed, it was important to look beyond the orthodontic progress and the space closure (Figure 5) and consider the implant position for the replacement of the missing tooth.
Flaring of the anterior teeth became a concern because 8 years of orthodontic treatment had left the buccal bone extremely thin. Although bone grafting was considered for the involved teeth, there was concern regarding correction of the narrow ridge on the edentulous area. With the aid of a cephalometric radiograph, the new interdisciplinary team had to consider whether the buccal inclination of the anterior teeth was an acceptable or correct position for both the short and long term, especially because an implant was to be placed. Cephalometric analysis is the clinical application of cephalometry; it is analysis of the dental and skeletal relationships of a human skull, and is frequently used by dentists, orthodontists, and oral and maxillofacial surgeons as a treatment planning tool.
While the temporary esthetic result achieved with the bonded tooth in the position of the left central incisor was an improvement, excessive buccal flaring of the maxillary anterior teeth was a concern with regard to longevity, as was a compromised implant placement with regard to proper position/angulation. The orthodontist was consulted to determine if an even better esthetic outcome could be achieved, and the interdisciplinary team agreed on a new treatment plan that included retraction of the upper and lower incisors, occlusal considerations for long-term function of an implant and crown, and a second round of orthodontic treatment.
Implants are known to absorb vertical loading forces significantly better than lateral forces.6 Consequently, when considering the placement of an implant to replace an anterior tooth, anterior guidance, excursive movements, and their loading forces must be taken into account. Without a second phase of orthodontic treatment, the implant would have been placed in relation to teeth that were improperly positioned, resulting in off-axial loading and esthetic compromise. Although the second phase of orthodontics was limited due to the fact that the patient had already concluded much of his growth and treatment time was, therefore, not fully sufficient, the treatment result nonetheless was highly effective, as a proper space was created for the future implant and tooth restoration, anterior teeth protrusion was reduced, and a proper, healthy occlusion was established. This treatment was completed in 16 months. Final orthodontic and debond images revealed a noticeable reduction of incisor protrusion and proper mesial-distal distance from the teeth adjacent to the future implant (Figure 6 and Figure 7).7
Evaluation of Progress
In patients with severe dental bimaxillary protrusion—a protrusive dentoalveolar position of maxillary and mandibular dental arches that produces a convex facial profile—several treatment options may be possible depending on facial profile, space requirements, and cephalometric findings. Extracting teeth (such as four bicuspids) may lead to the creation of excessive space and flattening of the facial profile during retraction. In addition, consideration must be given such that airway space is not encroached upon during significant retraction.8 An acceptable alternative to extractions may be the placement of mini-implants or mini-plates in the posterior of the mandible and maxilla to distalize the upper and lower dentitions.9 The ultimate result is judged not only by the esthetic outcome and proper function but also by a long-lasting healthy outcome and a proper tissue biotype to protect the implant and restoration.
Upon completion of the orthodontic treatment, occlusion and esthetic tooth alignment were evaluated. To assess the space allocation on the missing tooth, a radiograph was taken to ensure that the future implant would have adequate mesial-distal space and not be in close proximity to adjacent roots (Figure 7).
Furthermore, a final cephalometric radiograph was taken to evaluate the patient's profile and proclination of the anterior teeth. Several parameters must be established before fixed orthodontic appliances are removed. It has been suggested that at least 1.5 mm to 2 mm of interproximal bone be maintained between teeth and implants.10,11 The diameter of the future implant used for the tooth being replaced has an impact on not only the biomechanical and esthetic functions but also the proximity to adjacent teeth and the preservation of healthy buccal and lingual bone. The restorative contact point and its relationship to the underlying proximal bone helps to determine the presence or absence of a papilla.12 In implant therapy, formation of biologic width is consistent with varying degrees of bone remodeling.13 This relates to the presence or absence of the proximal periodontium of the adjacent tooth.14
Implant-Supported Restoration
Facial osseous integrity is required for not only osseointegration but also the stability and health of soft tissues. A deficiency in this area will lead to recession.15,16 When teeth are congenitally missing, typically there is a ridge of inadequate thickness to receive an implant unless a staged or simultaneous bone grafting procedure is performed. Numerous techniques have been proposed to reconstruct the localized alveolar ridge to facilitate implant placement.17-19 Regardless of the mode of regeneration, adequate bone thickness must be achieved for a sustainable, healthy, and esthetic outcome.
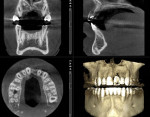
Additionally, a CBCT scan is paramount for proper 3-dimensional implant planning to determine the optimal bone grafting protocol and location for the implant and its proximity to adjacent teeth, and to evaluate the quantity and quality of the surrounding osseous foundation (Figure 8). Also, the surgeon should know at this point if the final restoration will be cemented or screw-retained, and any concerns should be addressed to avoid potential miscommunications regarding the final implant position and design for the final restoration. In this case the knife-edge ridge was also corrected to provide a proper foundation for the implant. Due to an extreme deficient buccal concave contour on the maxillary right central incisor, the final contour of this tooth also had to be considered, as the adjacent edentulous area would need a bone graft to correct the edentulous knife-edge ridge, and the implant size and position and final crown contour would have to be evaluated.
When replacing an anterior tooth with an implant-supported restoration, as in this case, it is important to develop hard and soft tissue using a provisional restoration to facilitate an ideal emergence profile and optimal esthetics (Figure 9). The tissue should be allowed to mature so the laboratory technician can fabricate the final crown to accurately represent the clinical situation. The ultimate goal is to provide patients a healthy, stable, functional, and highly esthetic result with which they can be well pleased.
Laboratory Process
The prosthodontist engaged the laboratory technician when the patient was starting the final restoration process, thoroughly explaining the patient's history. The technician decided to utilize a castable screw-retained prosthetic because the access hole had sufficient depth and was located appropriately. Additionally, the patient's future was considered; the technician believed that a screw-retained restoration would be easier to monitor after completion, and more hygienic overall, as retrieving the restoration from the mouth during recall visits is much easier than working with cemented restorations. It is also much healthier for the soft tissue and eliminates the undesirable potential for peri-implantitis to occur.
Once the implant had been placed, an analog was utilized to send the information to the laboratory for fabrication of the implant-supported restoration (Figure 10 and Figure 11). The technician waxed up the screw-retained frame (Figure 12 and Figure 13) and then cast the wax-up in 65% gold ceramic alloy (Figure 14 and Figure 15). The technician then built porcelain onto the casted and conditioned framework (Figure 16). The technician has utilized 65% gold precious metal for more than 20 years and has found it to be very reliable as a substructure for porcelain in comparison with zirconia. This case also provided enough space for the technician to build up the porcelain using gold ceramic alloy, and it was sufficient esthetically.
The final screw-retained central was placed on the model (Figure 17) and then tried in the patient's mouth (Figure 18), and final adjustments and steps were made for the emergence profile, ensuring that the restoration's contours properly establish the ideal emergence profile for the restored central (Figure 19 and Figure 20). The technician then performed a final check of the restoration on the model (Figure 21 through Figure 23).
The final restoration was placed in the patient's mouth, and the entire team was satisfied with a strong esthetic and functional result (Figure 24 through Figure 26).
Conclusion
As this case demonstrated, complex diagnoses require the assembly and cooperation of an interdisciplinary team. Although treatment may be administered over a long period of time and may not necessitate that every dental specialist be involved in every step of the process, it is essential that the treatment team follow the patient's progress together. In this case, the recognition of failure to achieve an ideal outcome with the first phase of orthodontic treatment demanded a mid-treatment revision. By following this framework clinicians can help ensure that a successful outcome is achieved and the patient is happy with the results.
About the Authors
Sergio Rubinstein, DDS
Private Practice limited to Prosthodontics, Cosmetic Dentistry, and Implant Dentistry
Skokie, Illinois
Toshiyuki Fujiki, RDT
Laboratory Technician
Skokie, Illinois
Barry P. Levin, DMD
Clinical Associate Professor,
Department of Graduate Periodontology
University of Pennsylvania School of Dental Medicine
Philadelphia, Pennsylvania
Private Practice limited to Periodontics and Implant Dentistry
Jenkintown, Pennsylvania
Diplomate, American Board of Periodontology
Elizabeth R. Michalczyk, DMD, PhD
Resident, Georgia School of Orthodontics
Atlanta, Georgia
Yan Razdolsky, DDS
Private Practice limited to Orthodontics
Buffalo Grove, Illinois
Diplomate, American Board of Orthodontics
References
1. Morley J, Eubank J. Macroesthetic elements of smile design. J Am Dent Assoc. 2001;132(1):39-45.
2. Newton JT, Prabhu N, Robinson PG. The impact of dental appearance on the appraisal of personal characteristics. Int J Prosthodont. 2003;16(4):429-434.
3. Davis LG, Ashworth PD, Spriggs LS. Psychological effects of aesthetic dental treatment. J Dent. 1998;26(7):547-554.
4. Klages U, Claus N, Wehrbein H, Zentner A. Development of a questionnaire for assessment of the psychosocial impact of dental esthetics in young adults. Eur J Orthod. 2006;28(2):103-111.
5. Kokich VO Jr, Kiyak HA, Shapiro PA. Comparing the perception of dentists and lay people to altered dental esthetics. J Esthet Dent. 1999;11(6):311-324.
6. Koyano K, Esaki D. Occlusion on oral implants: current clinical guidelines. J Oral Rehabil. 2015;42(2):153-161.
7. Livas C, Jongsma AC, Ren Y. Enamel reduction techniques in orthodontics: a literature review.Open Dent J. 2013;7:146-151.
8. Oksenberg A, Arons E. Sleep bruxism related to obstructive sleep apnea: the effect of continuous positive airway pressure. Sleep Med. 2002;3(6):513-515.
9. Ohura R, Kuroda S, Takahashi T, et al. Efficient usage of implant anchorage to treat overerupted maxillary first molar and mesially inclined mandibular molars.Am J Orthod Dentofacial Orthop. 2011;139(1):113-122.
10. Borges T, Lima T, Carvalho A, Carvalho V. Clinical outcome of inter-proximal papilla between a tooth and a single implant treated with CAD/CAM abutments: a cross-sectional study. J Oral Maxillofac Res. 2012;3(3):e4.
11. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75(9):1242-1246.
12. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
13. Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74(12):1785-1788.
14. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
15. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
16. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113-119.
17. Cordaro L, Amadé DS, Cordaro M. Clinical results of alveolar ridge augmentation with mandibular block grafts in partially edentulous patients prior to implant placement. Clin Oral Implants Res. 2002;13(1):103-111.
18. Miyamoto I, Funaki K, Yamauchi K, et al. Alveolar ridge reconstruction with titanium mesh and autogenous particulate bone graft: computed tomography-based evaluations of augmented bone quality and quantity. Clin Implant Dent Relat Res. 2012;14(2):304-311.
19. Misch CM. Bone augmentation of the atrophic posterior mandible for dental implants using rhBMP-2 and titanium mesh: clinical technique and early results. Int J Periodontics Restorative Dent. 2011;31(6):581-589.