Single-Unit Screw-Retained Implant Restoration Using GC Gradia®
Finding the right solution and materials for implant restorations.
The debate about the choice between cement-retained and screw-retained dental implants is ongoing and one with an extensive history.1 This article will offer a sound solution to some of the concerns raised by both sides. The major reasons clinicians prescribe screw-retained restorations are to avoid using cement because of possible health concerns and when limited space between the implant fixture and the opposing dentition preclude the use of a cemented restorative option.2-4 On the other hand, clinicians are likely to prescribe cement-retained implant restorations mainly because of their heightened esthetics due to the absence of an access hole and the increased stability of cement-retained crowns compared to porcelain-fired, screw-retained restorations.5
Restorative Options
GC GRADIA® (GC America, www.gcamerica.com), a micro-ceramic composite, is an attractive option for fabricating screw-retained implant restorations (SR) because of its flexural properties for stability, layering capabilities for esthetics, and its ability to seal the access hole during delivery, thus providing an uninterrupted compressive force.6 In this article, the author will examine the process for fabricating a single-unit, screw-retained implant using GC Gradia and a CAD/CAM titanium abutment customized with the NobelProcera™ Scanner (Nobel Biocare, www.nobelbiocare.com).
GC Gradia is a micro-ceramic light-cured composite composed of 80% ceramic. The high amount of ceramic allows it to retain its color, shine, and vitality. In use in the United States since 2002, GC Gradia was initially used in crown and bridge with conventional metal substructures, as CAD/CAM titanium was not as prevalent as it is today. The bond strength of this composite to CAD/CAM titanium is measured at 29.96 MPa.6 This procedure will provide technicians with acceptable bone strength—slightly above the minimum standards of 25 MPa—only if the same materials and technique are used to produce the resin-to-titanium bond.
GC Gradia has been used for screw-retained hybrid type restorations with conventional alloys as well as CAD/CAM titanium abutments and bars, crown-and-bridge restorations with metal substructures, and inlays and veneers.7 Its attributes allow it to be used for single-unit, screw-retained titanium implants because it has more flexural strength than fired porcelain and will absorb more of the impact.
A composite can be layered using the same strategies as when stacking porcelain, but the feel is similar to that of waxing a crown. An experienced ceramist with extensive waxing experience will be proficient in little time. The material should be applied in increments from the inside out, then each layer will be pre-cured for 5 to 10 seconds, and then final cured when build-up is complete. In this case, the Optilux light-cure machine (Demetron Corporation) was used for the step cure, and the Sculpture® Light cure unit, (Pentron, www.pentron.com) was used for the final cure. Because it is a composite, the restoration does not require the conventional firing step. The advantage of working with a cured versus fired material is that what you see is what you get in terms of color and translucency. Dimensional changes are minimal during the final curing process, so you can either build into correct occlusion and intercuspal position (IP) contacts or build into proper morphology and grind in wear facets to uncover natural worn esthetics (Figure 1). After delivery, if additions are needed, the clinician can add composite adjustments into the mouth without removing the restoration. In order to accomplish this, the clinician can roughen the surface with a diamond bur, apply GC Composite Primer (GC America), light cure primer for 1 minute, and then apply GC GRADIA as needed. The final step cure and polishing of GRADIA can be accomplished in the mouth.
The compressive force of a material is an important part of the bonding mechanism for metal ceramics. By design, traditional porcelain-fired, screw-retained implants require the access hole to be open. At delivery, when the restoration is torqued into place, the access hole is then filled and sealed with a light-cured chairside composite material. A more recent option for porcelain-fired, screw-retained implant restorations is to produce for the access hole a porcelain plug, which is cemented into place after torqueing. Both options introduce cement as the second material. The composite does not support the free porcelain around the access hole, and the plug is not a homogeneous part of the crown because it is separated by cement. Using GC GRADIA for screw-retained implant restorations eliminates these factors. By using this composite to build up the crown, the access hole, which will still be open, can be sealed at delivery and no secondary material, like cement, will be needed. A pre-cured plug should not be cemented in this case because the compressive force needs a homogeneous continuance, not a cement joint. To prepare for the application of the composite at delivery, the laboratory sandblasts the material into the access hole prior to shipping the case to the office. Then, at delivery, the clinician applies and light cures GC Composite Primer for 1 minute, fills the hole with GC GRADIA, final cures, and polishes. This encapsulates the titanium abutment with no joints or secondary material.
Building a Screw-Retained Implant Restoration
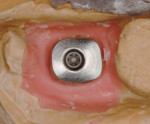
The technician designs the implant abutment with undercuts, which are needed to aid in the stability of the restoration (Figure 2). The gingival finish line can be more subgingival because there is no cement gap (Figure 3). The completed abutment is finished using a carbide bur, being careful to smooth any sharp edges and accentuate the undercuts where needed. The finishing line should be crisp and clear to prevent any micro-leakage between resin and metal substructure. It is important to remember that composite materials do need mechanical retention to aid in the stability of the restoration, and undercuts are an easy method of attaining this using the CAD software from NobelProcera.
The abutment is then sandblasted above the finish line using 125-µm aluminum oxide at 3 bars of pressure (Figure 4). The abutment is then rinsed and put in an ultrasonic bath to clean off any aluminum oxide residue. It is important to wear gloves from this point on until the opaque has been applied.
The next step is to apply a metal primer liberally onto the abutment using a brush and letting it dry. A foundation opaque is then applied to cover all of the gray metal. It usually takes two layers to completely mask the metal (Figure 5). A shaded opaque is applied over the foundation opaque (Figure 6), and then a 50/50 mixture of the desired shade and margin opaque is applied to the gingival and occusal groove (Figure 7). Care should be taken to avoid blocking the access hole during this process. For the next steps in the fabrication process, the abutment will need to be screwed into the model. Overall, the foundation and opaque layers should be about 0.5-mm thick.
Model hardener and separator will need to be applied to the working and the opposing models. The dentin build-up can be to full contour and cut back or built up to mimic natural dentin structure without cutting back—whichever strategy is most familiar when stacking porcelain. The author showed the build-up without cutback. The opacious dentin was applied to about 80% of the space that the dentin layer would occupy (Figure 8 and Figure 11). The author could then complete the dentin structure with dentin material (Figure 12 and Figure 13) and apply mamelon stain or intensive color to mimic natural internal color, mamelons, and crack lines (Figure 14). Next, he applied a thin layer of translucent material (Figure 15 and Figure 16) and then enamel effects, like enamel intensive and enamel, were used to full contour above the height of the contour and enamel at the marginal ridges (Figure 17 and Figure 18). This application adds to the perception of depth in these areas. The author used pearl enamel for the triangular ridges and filled in the rest of the occlusion with the same enamel that was used to finalize the coronal shape (Figure 19).
The next step was to unscrew the restoration and fill the IP void with opacious dentin and overlay it with cervical translucency below the height of contour. If there is a large void in the IP area and the opaque is visible, opacious dentin should be added. Finally, the IP area was overlaid with enamel above the contour height (Figure 20) and final cured for at least 3 minutes.
Contour
Using a diamond bur or cross-cut carbide bur, the author fitted the IP contacts, occlusal contacts, and gross contoured the crown. It is okay to use a friction grip carbide for detailing the occlusal anatomy. The author used a cross-cut carbide and a rubber wheel for final contour and to check the contacts (Figure 21). Next, he cleaned the finish line and rubber wheeled the titanium emergence profile. It is not advisable to polish the metal at this point because GRADIA that has not been glazed or polished will collect residue from the polishing compound. The metal should be polished only after Optiglaze is final-cured.
Glaze and Polish
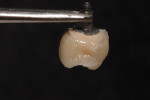
The finished restoration was sandblasted with aluminum oxide at 2-bar pressure, rinsed, brushed with light detergent, and put in an ultrasonic bath for 2 minutes. The restoration was then dried completely using an air hose, but only after it was freed of moisture and oil. A thin coat of Optiglaze was applied to the dry surface and light cured. It is important to avoid over-working this material to minimize a tendency to pucker. The author then final-cured the Optiglaze (Figure 22), re-polished the titanium with a rubber wheel (which should be done only if needed), and brought the metal to a high shine. Using a soft rubber wheel, he then polished wear facets, height of contour, and emergence profile to produce a smooth surface free of voids (Figure 23). In completion, the author buffed the crown with GC Polish Paste (GC America) and a Robinson brush (Buffalo Dental Manufacturing Co., Inc. www.buffalodental.com) to his desired sheen (Figure 24). Note that dental technicians who need to add composite must roughen the surface and apply composite primer before adding material.
References
1. Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997 ;77(1):28-35.
2. Sailer I, Mühlemann S, Zwahlen M, et al. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res. 23 (suppl 6):163-201.
3. Chee W, Jivraj S. Screw versus cemented implant
supported restorations. Br Dent J. 2006 ;201(8):501-507.
4. Magne P, Magne M, Jovanovic SA. An esthetic solution for single-implant restorations – type III porcelain veneer bonded to a screw-retained custom abutment: a clinical report. J Prosthet Dent. 2008 ;99(1):2-7.
5. Torrado E, Ercoli C, Al Mardini M, et al. A comparison of the porcelain fracture resistance of screw-retained and cement-retained implant-supported metal-ceramic crowns. J Prosthet Dent. 2004 ;91(6):532-537.
6. Fernandes CA, Ribeiro JC, Larson BS. Microtensile bond strength of resin-based composites to Ti–6Al–4V. Dent Mater. 2009 ;25(5):655-661.
7. Atcha I, Kahng L. Implant-Retained Prosthetics. Inside Dental Technology. 2010 ;1(2):58-63.
Disclosure
The author has received an honorarium from GC America for writing this article.
About the Author
Mike Dominguez, CDT, TE
Owner
Kymata Dental Arts
Seattle, Washington