Innovative Staged Treatment of a Worn Dentition
Dana G. Colson, DDS, MBA
Abstract: Often patients adapt to a decline in their oral condition over time and choose to live in discomfort, and sometimes pain, until it becomes intolerable. Ongoing parafunctional habits and other disease conditions may contribute to and exacerbate the problems. This case report illustrates an innovative approach to a full-mouth rehabilitation by staging complex treatment planning in the restoration of teeth severely damaged by the effects of gastroesophageal reflux disease compounded by clenching. Occlusal landmarks were identified and maintained, which allowed for both case completion and accommodation of the patient's travel commitments. The successful outcome resulted in a grateful patient who could chew comfortably with a stable occlusion and a pleasing, confident smile.
Extreme changes in an adult dentition can occur rapidly when multiple risk factors are combined. In the case presented, the male patient's dentition changed dramatically over an 8-year period due in large part to gastroesophageal reflux disease (GERD) and daytime clenching. Significant generalized enamel and dentin loss had occurred, and the patient's maxillary lateral teeth had shifted despite a healthy periodontium.
This case presented challenges because despite the urgency to protect the vitality of the posterior teeth from continued severe erosion, treatment staging was necessary due to the patient's need to travel out of country. A Kois deprogrammer was used to establish an orthopedic reference position other than maximum intercuspation (MIP), and this reference position was a starting point for the functional treatment planning decisions. A diagnostic wax-up utilizing this reference position served as the blueprint to provide treatment with predictable results. After the vertical dimension and a repeatable bite position were verified, the posterior occlusion was established. Limited orthodontic treatment was then utilized to reposition anterior teeth for the preservation of maximum tooth structure prior to full anterior crown preparation and to help center the midlines of the arches. This altered sequence of treatment may be an option for other cases that require staging due to the need for patient travel or to accommodate financial limitations.
Clinical Case Overview
The serious consequences of awake bruxism (clenching) and GERD on a middle-aged dentition were quite apparent in this case. A 69-year-old man had originally presented to the office in 2009 for a comprehensive examination but did not immediately return for treatment. He returned 8 years later with the chief concerns of pain in his mandibular left molar (tooth No. 18) and a desire to improve his bite. He reported jaw muscle tenderness despite wearing a thermoplastic retainer at night and while exercising. Generalized severe erosion and attrition were evident. Teeth Nos. 7 and 10 had shifted despite good bone support.
After experiencing tooth pain and seeing the photographic evidence of wear and tooth destruction over the previous 8 years, which was presented to him at this time, he was now motivated to follow through with a comprehensive treatment plan to address the root causes of the problems. The treatment plan was segmented to accommodate the patient's extended travel itinerary.
Medical and Dental History
The patient was classified as American Society of Anesthesiologists (ASA) II. He was taking apixaban, an anticoagulant, for atrial fibrillation and reported a prostate disorder. Upon questioning, he revealed that he used a continuous positive airway pressure (CPAP) machine nightly and had experienced gastric reflux, which subsided after he started using the CPAP.
The dental history included fear of dental treatment, a history of broken and/or chipped teeth, toothaches (No. 18) and/or cracked fillings, food trapping between his teeth, an awareness that his teeth had changed in the past 5 years, and past use of a bite plate. He was uncomfortable and self-conscious about the appearance of his teeth. He reported awareness of clenching during the daytime.
Diagnosis, Risk Assessment, and Prognosis
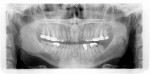
Periodontal: The periodontal examination revealed generalized clinical attachment loss but no pockets greater than 3 mm, no bleeding on probing, and no significant mobilities of any teeth. Adequate attached gingiva was present on all teeth. Home care was acceptable. Generalized tissue and bone loss was evident on the buccal surfaces of the posterior teeth. His periodontal disease was classified as stage II, generalized, grade A based on the radiographic bone loss of more than 2 mm but less than 4 mm interdentally and the comparisons of interdental bone level from his two panographic radiographs taken 8 years apart.
Risk: Moderate
Prognosis: Fair
Biomechanical: Significant tooth structure loss had occurred between 2009 and 2017 (Figure 1 through Figure 3). Severe attrition had occurred on the anterior teeth, especially tooth No. 11. Severe erosion and abrasion were present on teeth Nos. 11, 18, 20, 21, 28, 29, 31, and 32 (Figure 4). The patient had generalized sensitivity, and tooth No. 18 was painful due to deep erosion, which approached the pulp chamber. Teeth Nos. 7 and 10 had moved out of position and rotated (Figure 5). The progression of erosion over the 8-year period could also be seen radiographically and was especially noticeable on tooth No. 18 (Figure 6 and Figure 7). The occlusal resins were lost on the mandibular molars, and the erosion and abrasion from the opposing crowns continued to erode the tooth structure.
Risk: High
Prognosis: Poor
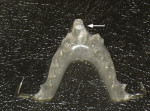
Functional: Attrition was noted on the teeth that were not protected with full-coverage crowns (Figure 8 and Figure 9). While wearing a Kois deprogrammer for about 1 month prior to restorative treatment, the mandibular teeth wore a notch in the deprogrammer platform, confirming clenching and the possibility of an impaired cortical control of the central pattern generator (Figure 10).1 All platform variables were verified and proper design of the Kois deprogrammer was followed. (The notch in the deprogrammer was repaired, leaving a smooth, flat surface to allow the proper position of the mandible to be determined.) The temporomandibular joint examination revealed normal opening with no joint sounds. The load and immobilization tests were normal. All the muscles, except the masseter, had no tenderness to palpation. Trigger points were palpable within the masseter muscles, which were hypertrophied. The diagnosis was determined to be occlusal dysfunction with the addition of awake bruxism and clenching. Upon questioning, the patient shared that he clenched while playing tennis daily, which he was very passionate about. The evidence that he was not grinding at night was the fact that tooth No. 11 was extremely cupped and not flattened. This ruled out a diagnosis of sleep bruxism, as the incisal edge would have become flat due to lateral movements of the mandible.
Risk: High
Prognosis: Poor
Dentofacial: There was no gingival display in the patient's Duchenne smile. Teeth Nos. 7 through 10 were not visible in repose. His tooth shade was noted as A4 on the Ivoclar shade guide (Universal A-D Shade Guide, Ivoclar, ivoclar.com). The patient wished to have whiter teeth and feel more confident smiling.
Risk: Low
Prognosis: Poor
Treatment Goals
The treatment goals were to create an esthetic smile, prevent further destruction of tooth structure, relieve tooth discomfort, and increase awareness of daytime clenching. A daytime biteplate would be worn while playing sports and a nightguard for nighttime protection.
Treatment Plan
The treatment plan encompassed a six-prong approach. First, a repeatable reference position of the mandible would be created to facilitate planning and execution of increasing the vertical dimension, developing a functional occlusion, and improving esthetics. Second, periodontal and endodontic treatment would be provided to resolve the discomfort on tooth No. 18. Third, posterior teeth would be restored with zirconia crowns at a new vertical dimension of occlusion, leaving an anterior open bite to facilitate orthodontic movement while providing a solid occlusion during the patient's travels. Fourth, clear aligner orthodontics (Invisalign®, Align Technology, Inc., invisalign.com) would be used to appropriately position the anterior teeth. Fifth, the anterior teeth would then be restored with lithium-disilicate crowns. Sixth, and finally, postoperative protection would be provided through the use of long-term protective appliances to manage parafunctional habits.
Treatment Phases
Diagnosis and Occlusal Records
Compete diagnostic records were taken, including intraoral photographs; full-mouth x-rays; panoramic, cephalometric, and transcranial radiographs; a digital scan; and a facebow registration. A comprehensive treatment plan was presented to the patient, which he accepted.
The patient underwent routine periodontal care and was placed on a 4-month re-care frequency. He was given treatment options for tooth No. 18 and elected to have the tooth treated endodontically.
The patient wore the Kois deprogrammer for 1 month.2 New photographs and models were then taken. A bite registration (Regisil®, Dentsply Sirona, dentsplysirona.com) was taken with the deprogrammer in place at the new vertical dimension.3 The models were mounted on an articulator (Panadent, panadent.com) using a facebow (Kois Dento-Facial Analyzer, Kois Center, koiscenter.com). The records were sent to the laboratory for a diagnostic wax-up.4,5 Photographs were used by the lab to aid in creating the wax-up.6-8
Initial Restorative Phase
The maxillary posterior teeth were prepared for full-contour zirconia crowns. The deprogrammer was placed in the mouth and composite was added to the lingual surfaces of teeth Nos. 8 and 9 to create a centric and vertical stop at the new vertical dimension. A tooth preparation guide was fabricated from the wax-up and used to minimize tooth structure removal while allowing the necessary occlusal reduction to be obtained.
After preparation, a two-step self-etch bonding agent (Clearfil™ SE Bond, Kuraray, kuraraydental.com) was applied to the preparations and light-cured. A dental laser (Waterlase iPlus®, Biolase, Inc., biolase.com) was used to create visible supragingival margins for the digital scan (iTero®, Align Technology, Inc., itero.com).9 The teeth were temporized with a bisphenol A-glycidyl methacrylate (bis-GMA) resin (Luxatemp®, DMG America, dmg-america.com) and cemented with a zinc-oxide eugenol-based temporary cement (Temp-Bond™, Kerr, kerrdental.com). Composite was added to the mandibular posterior molars to create a solid posterior occlusion.
Two weeks later the maxillary zirconia crowns were cemented with a self-adhesive universal resin cement (RelyX™ Unicem, 3M Oral Care, 3m.com) after verifying the margins, interproximal contacts, color, and esthetics. The prepared teeth were microetched, and a single-step self-adhesive bonding agent (Universal All-Bond®, Bisco, bisco.com) was applied and cured. The crowns were microetched, washed, and dried. A ceramic primer (Z-Prime®, Bisco) was applied with a microbrush for 1 minute on each individual crown, and the aforementioned self-adhesive universal resin cement was dispensed into each crown prior to seating. Excess cement was removed.
The mandibular posterior teeth were then prepared for full-contour zirconia crowns, scanned, and temporized as described for the maxillary arch. A few weeks later the mandibular posterior crowns were cemented (RelyX Unicem) (Figure 11) with the same protocol used for the maxillary posterior crowns. The occlusion was equilibrated and verified to have equal, simultaneous, and bilateral contacts.
Orthodontics
A new scan and photographs were taken and submitted to Invisalign with the goal of utilizing clear aligner orthodontic therapy to straighten the mandibular anterior teeth and match the maxillary midline. In addition, a more ideal alignment of the mandibular anterior teeth would minimize tooth reduction on teeth Nos. 23 and 24 (Figure 11). The clear aligner trays were delivered prior to the patient's departure for a lengthy stay at another home out of country.
Second Restorative Phase
When the patient returned 7 months later, the anterior teeth were better aligned, an overjet was created, and the midline was centered (Figure 12). The preparations on teeth Nos. 6 through 13 and 22 through 27 for lithium-disilicate crowns (e.max®, Ivoclar) were completed, scanned, and temporized. The temporaries were used to verify that the desired esthetic changes were accomplished. The same chairside procedure was used for temporization as with the posterior molars. The amount of display of the anterior teeth was increased 1 mm to be visible in repose. A stump photograph was taken with the shade guide for the laboratory. Photographs were taken for lab communication, and the patient went to the lab for custom shading.
Three weeks later the patient returned to the office for the cementation procedures. After clinical assessment of proximal contacts, marginal integrity, and patient approval of the esthetics and speech patterns, the crowns were cemented. The maxillary incisors had a pleasing display in repose (Figure 13). The same cementation protocols were used as in the initial restorative phase, except silane was applied to the internal surfaces of the crowns. Occlusion was verified, ensuring no functional interferences on the anterior teeth (Figure 14).Shimstock was used to verify stable centric occlusal MIP contacts on the posterior teeth. Articulating film (AccuFilm®, Parkell, parkell.com) verified positioning of the cusp-to-fossa relationships with a minimum of one stable contact for each tooth, and 200-µm blue paper (Bausch, bauschpaper.com) was used to verify that there were no lateral streaks when the patient was sitting up at a 45-degree incline while chewing on the paper. A post-treatment full-face photograph is shown in Figure 15.
Discussion
An accurate diagnosis was essential and was used to determine the proper materials for posterior crown design and post-treatment appliance usage to ensure long-term treatment success. The patient interview was critical in this case because most of his answers on the dental history form were negative, and important information was only revealed during the interview. The patient was educated repeatedly about the need for and importance of long-term dental protection and maintenance. A nighttime bite appliance was made, and the patient requested a sports mouthguard to protect his teeth when playing tennis. Ongoing instructions were given to the patient about being conscious of his tendencies to clench. He was instructed to keep his lips together and teeth apart.10
Conclusion
This case demonstrated a systematic and predictable method for a full-mouth rehabilitation that required segmenting the treatment due to the patient's travel requirements. Many patients adapt to their gradual dental decline without noticing it until discomfort creates an urgency to address it. For this patient, fear of being in a dental office had been a barrier to receiving dental care, but once he was made aware of how significant the destruction had become, he was willing to move forward with treatment. The patient and his spouse were thrilled with the result. Due to the high risks from the patient's parafunctional habits,11 this case must continue to be monitored closely.
Acknowledgment
The author thanks dentalstudios-Burlington (Burlington, Ontario, Canada) for the talent and artistry it provided, and its president, Trevor Laingchild, RDT, AAACD, for his exceptional creation of this case; John C. Kois, DMD, MSD, for his teaching on the art of restoring occlusion; and Susan A. Sheets, DDS, and Matthew West, DMD, for their guidance and encouragement to manifest this article.
About the Author
Dana G. Colson, DDS, MBA
Creator of Wellness Based Dentistry™️; Private Practice, Toronto, Ontario, Canada; Mentor, Kois Center; Fellow, Academy of General Dentistry; Accredited Member, International Academy of Oral Medicine and Toxicology; Fellow, American Academy of Clear Aligners; Author,Your Mouth, the Gateway to a Healthier You
References
1. Lavigne GJ, Kato T, Kolta A, Sessle BJ. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14(1):30-46.
2. Kois J, Hartrick N. Functional occlusion: science-driven management. J Cosmetic Dent. 2007;23(3):54-57.
3. Misch CE. Guidelines for maxillary incisal edge position-a pilot study: the key is the canine. J Prosthodont. 2008;17(2):130-134.
4. Tak On T, Kois JC. Digital smile design meets the dento-facial analyzer: optimizing esthetics while preserving tooth structure. Compend Contin Educ Dent. 2016;37(1):46-50.
5. Kois JC. Diagnostically driven interdisciplinary treatment planning. Seattle Study Club J. 2002;6(4):28-34.
6. Kois JC, Phillips KM. Occlusal vertical dimension: alteration concerns. Compend Contin Educ Dent. 1997;18(12):1169-1174.
7. Spear F. The maxillary central incisor edge: a key to esthetic and functional treatment planning. Compend Contin Educ Dent. 1999;20(6):512-516.
8. Simon H, Magne P. Clinically based diagnostic wax-up for optimal esthetics: the diagnostic mock-up. J Calif Dent Assoc. 2008;36(5):355-362.
9. Lowe RA. Clinical use of the Er,Cr: YSGG laser for osseous crown lengthening: redefining the standard of care. Pract Proced Aesthet Dent. 2006;18(4):S2-S9.
10. Colson DG. Your Mouth: The Gateway to a Healthier You. DJC Corp; 2011:34-71.
11. Lavigne G, Kato T. Usual and unusual orofacial motor activities associated with tooth wear. Int J Prosthodont. 2005;18(4):291-292.