Flexibility in CAD/CAM Denture Design
Using an open-source 3D graphics software to create a customized dental CAD program allows for more freedom and control of denture design
Craig J. Holland
At the onset of the COVID-19 pandemic in 2020, many dental school faculty members had to adapt to teach their courses remotely. The author had previously discussed the development of an educational CAD software with Wendy AuClair Clark, DDS, MS, a Clinical Assistant Professor at the University of North Carolina Chapel Hill's Adams School of Dentistry. This emerging need for remote education options along with the unexpected closures of many dental offices provided the author's laboratory with the time and opportunity to make the project a reality. This subsequently led to the development of additional software that proved useful to the laboratory's production workflow.
The team began by learning the basics of coding (scripting) in the common computer language Python in order to use a free, open-source 3D computer graphics software (Blender™). The software has an open license, which encourages users to modify and rescript it—improving and personalizing the software to meet their individual needs. A dental anatomy software was then developed as the first educational module, which mimicked conventional waxing exercises, allowing students to digitally sculpt a tooth. The second module created was a removable partial denture (RPD) design software. This allowed for the remote instruction of surveying and designing RPDs. To complete the educational package, a final module was developed for the design and fabrication of custom trays for a complete denture course. The final customized software was beta tested with students from the University of North Carolina and the University of Iowa. Each student was able to download the software onto their own personal laptops, allowing the professors to teach concepts remotely that otherwise would have required in-person laboratory time—which at the time was limited due to the COVID guidelines.
Together, the three modules became an educational software suite (3PX Merlin, 3 Point Dental Studios), which was made available to download for free by any school or individual wanting to use it to supplement their education.
After the successful creation of that suite, the laboratory team decided to develop a package that would be accurate and user friendly for the daily production needs of both the dentist and the commercial laboratory. The result of that endeavor became another software platform (3PX Excalibur, 3 Point Dental Studios). The openness of the platform allows more flexibility than more closed software does. Designed and developed by dental technicians and prosthodontists, it attempts to follow the step-by-step clinical and laboratory workflows. The following case report demonstrates how a software such as this can be utilized in designing a milled zirconia all-on-X restoration.
Case Report
A patient presented with a need for a full-arch maxillary implant prosthesis opposite an existing full-arch mandibular prosthesis. The restoring clinician verified the master cast with an accuracy verification system (AVS) and adjusted the patient's conversion prosthesis to the correct occlusal relationship. Impressions were made of the provisional prosthesis, opposing prosthesis, and occlusion with an intraoral scanner (TRIOS®, 3Shape). Upon receiving these scans, the technician imported STL files into the Models Module of the CAD software (3PX Excalibur) and aligned to the scans of the verified master casts (Figure 1). Once the scans were aligned, adjusted titanium cylinders were seated on the model and then scanned and aligned to the other scans (Figure 2). This allowed the final design to mimic the patient-approved provisional prosthesis in both function and esthetics. A custom object was designed in the software to represent the cylinders and the access holes (Figure 3). These objects were used to cut material away from the final design, leaving a negative representation of the objects as space for the cylinders to attach to after fabrication of the prosthesis.
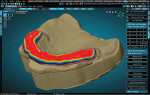
Teeth were imported from an attached library (found in the RPD Module of the CAD software) and aligned to the scans of the provisional (Figure 4). The teeth were then customized using the sculpt tools in the software to emulate the provisional more closely. All of the scan files were then hidden from the scene except for the base models. The Digi Flipper Module was then opened and utilized to create the tissue base of the final restoration. The outline was formed to create a border and help control the placement of the tissue replication (Figure 5). Next, the RPD Module was accessed again to create the tissue base, carefully painting the model within the area outlined in the previous step (Figure 6). This painted area was duplicated and extracted from the model at the desired thickness (Figure 7). The RPD Module was accessed again to isolate areas for specific extraction of the tissue in a selected direction (Figure 8). This replaced the need for layering and exhaustive sculpting by adding material quickly in a controlled manner.
The previously designed teeth were brought back into the scene to aid in the fine tuning of the tissue replication. After final sculpting of the tissue area was completed, the teeth, tissue, and tissue base outline were selected and joined into one object (Figure 9). The objects that were created for cutting the access holes and cylinders were brought back into the scene (Figure 10) and the Boolean difference modifier was applied (Figure 11). The restoration was re-meshed to ensure there were no holes, and another Boolean difference was performed to cut the base model from the restoration. The opposing arch scan was turned on, and the design and occlusion were evaluated for possible final adjustments (Figure 12). The minimal thickness was checked using the C&B Module Thickness Assessment feature (Figure 13). The red areas show where the restoration is less than 0.5 mm thick and can be isolated and extruded to meet minimal requirements. The final restorations were prepared for milling to ensure they were manifold (not containing holes or reversed faces) and were then exported as an STL file.
Once the final restorations were designed, the nesting of the bridges was performed in the CAM software (hyperDENT®, FOLLOW-ME! Technology Group). Because this was a full-arch design, the bridge was nested with the labial area close to the outside of the puck to allow the mill to have the most advantageous angles (Figure 14). The connectors (bars that attach the restoration to the puck) were placed at the height of contour as marked by the software. The software option to remove 80% of the connectors was utilized as a final step to aid in the removal of the restoration from the puck post-milling. The software was used to simulate the milling of the internal surfaces in order to confirm the fit of the sintered bridge.
After the nesting was completed, the appropriate 3Y zirconia puck (STS Zirconia [B1], MiDenta Digital Dentistry™) was placed in the milling machine (AMD-500, Aidite®), which was 5-axis simultaneous milling platform with a large processing angles to allow up to 90° (vertical) milling of the restoration (Figure 15). Because the mill was allowed to freely carve the restoration as designed, the time needed for post-mill/pre-sinter modifications was minimized.
After the mill process was completed, the remainder of the connectors were carefully removed, and the points of connection were smoothed with a medium grit diamond bur in a slow speed handpiece. If needed, the interproximal areas can be cut with a diamond disc to create a more individualized look between connected teeth. Polishing wheels (ProArt Polishing Wheels, Ivoclar Vivadent) were used to further smooth any lines from the milling process and the connector areas. The restoration was then blown vigorously with compressed air to remove any micro-dust particles.
After polishing was completed, sintering was performed (Cameo® AGT-L Fast Sintering Furnace, Aidite). The cycle used for sintering will always be dependent on the number and size of units to ensure a full sintering of the material and proper cooling period.
The post-sintering processing included fine-tuning of the margins under a 45x power microscope (AmScope), adding any texture needed, and minor contour corrections were made using an assortment of grinding stones (Diamond Grind Stones, MiDenta Digital Dentistry). By running the grinding stones at extremely low speeds (2,000 rpm to 4,000 rpm), the technician could make minor adjustments slowly and meticulously without concern of overheating or incorporating microfractures into the zirconia.
The final step of the process was staining and glazing (MiYO® Esthetic System, Jensen Dental). The chosen stains were set based on translucency effects to allow for the illusion of translucency when placed properly. Tissue shades (MiYO Pink Liquid Ceramic, Jensen Dental) were chosen to match the same translucency aspect as the tooth shades (MiYO Liquid Ceramic, Jensen Dental). The combination of the matching tooth and tissue shades allowed for the 3Y zirconia to look natural on the bench as well as in the mouth (Figure 16).
Conclusion
Using an open-source CAD program has its advantages and disadvantages. Standard dental CAD software bundles are written specifically for dental use, minimizing the potential for user error; however, open programs can remove restrictions, allowing for more freedom and control of the design and its parameters. This type of software, once mastered, can become an asset to any laboratory and offer an affordable way for all laboratories and dentists to participate in digital dentistry.
About the Author
Craig J. Holland
Owner
3 Point Dental Studio
Fremont, Ohio