Digital Denture Diagnostics
Improve communication and visualization for case planning
By Robert Kreyer, CDT
This is the second part of IDT's ongoing digital denture series by Robert Kreyer.
Dental technicians play an integral role in the prosthetic dental team while having a symbiotic relationship with the restorative prosthetic clinician. Laboratory technicians should always strive to anticipate clinical needs for the next prosthetic procedure, and the clinician should strive to understand the technical needs of the dental laboratory technician. Collaboration with a multidisciplinary approach to prosthetic design and case planning among all members of the restorative team will improve communication of interdisciplinary treatment parameters such as prosthetic techniques, esthetics, functional occlusion, materials, and potential maintenance issues.
In this article, the author will discuss the importance of understanding prosthetic variables during case planning and how to improve communication and visualization using digital files instead of mounted stone casts.
Complete Prosthetic Case Planning Expectations
Understanding a patient's expectations and desires is critical to success with complete denture prosthetics. How can one know how to properly design an anterior smile for complete conventional dentures without understanding a denture wearer's desires and expectations?
Esthetics in the smile zone is one of the main reasons complete denture prosthetics fail. Not fulfilling the esthetic expectations will certainly result in an unhappy patient and require a remake. A denture wearer looks at their complete denture prosthetic when they smile in the mirror, while they clean their dentures, and before placing them in their mouth. If a patient is not satisfied with the esthetics and appearance of their complete prosthetic they will not smile with confidence, thus affecting their self-esteem. A very esthetic and functional complete denture prosthetic helps to restore self-confidence while enabling a denture wearer to not only do but to enjoy such things as eating, smiling, speaking, laughing, and singing. The ability to effectively change a life by restoring these precious blessings through understanding desires and expectations is our optimal goal during complete denture prosthetic treatment. Understanding a patient's expectations and desires is the gateway to successful complete prosthetic treatment.
Collaboration
To exceed those expectations, the clinician and technician must understand what each other's needs are during treatment. If the goal is to provide optimal prosthetic treatment and care, there must be clinical and technical collaboration. The best way for a dental technician to understand these expectations is to see the denture wearer or the current prosthetic situation through digital photos. The digital camera should be an integral tool in both the dental office and the dental laboratory.
All prescriptions to the dental laboratory should be accompanied by a series of photos. The preliminary impressions should be sent with photos of a patient's full face in repose, smile, and high lip line, plus profile and intraoral. Complete denture baseplates and occlusal rims with established records should be returned with photos of final contoured rims in the mouth showing full face, smile, high lip line, and profile. At the try-in appointment, the patient should also have photos taken with waxed teeth in the mouth showing the smile design and any changes that need to be done in the dental laboratory. The ability to provide a before-and-after photo truly creates value to the prosthetic service provided for an edentulous patient.
Case Planning Digital Model Analysis
The goal of model analysis is to understand prosthetic variables and obtain information that will guide clinicians and technicians in the design of complete denture prosthetics while understanding individual biomechanical considerations and limitations.
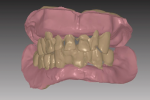
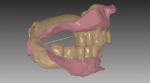
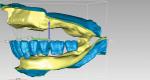
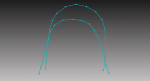
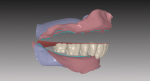
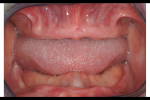
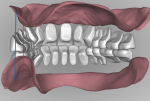
The impressions or master casts must capture all necessary dentate or edentulous anatomy within the denture space of the oral environment. An accurate maxillo-mandibular relationship and vertical dimension of occlusion records are essential to a successful prosthesis. After scanning the impressions or master casts and relationship record, the laboratory technician can then visualize the inter-residual ridge relationship and negative space for designing the complete denture prosthesis (Figure 1 and Figure 2).
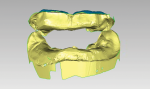
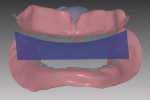
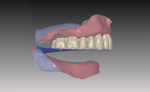
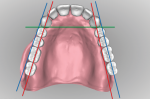
This virtual or digital model analysis enables the technician and clinician to understand all the variables involved with this immediate complete prosthetic case before actual treatment has begun. Understanding variables such as Class-I, -II, or -III skeletal relationships as well as restorative space for implant-retained or -supported prosthetics will help determine the proper occlusal scheme and functional design. To design immediate maxillary and mandibular complete dentures, the teeth are virtually extracted, then prosthetic space is evaluated for transitioning immediate dentures to implant-supported prosthetics (Figure 3).
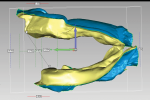
To determine if adequate prosthetic space exists, the inter-residual ridge space is measured to achieve a minimum of 28 mm between the maxillary and mandibular ridge crests. The mandibular is virtually reduced according to surgeon's specifications (Figure 4).
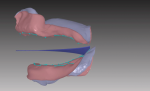
To confirm mandibular prosthetic space, anterior and posterior teeth are virtually set for prosthetic space confirmation. There is always a compromise between bone reduction and increasing the vertical dimension of occlusion. In this case, to achieve desired space the VDO will have to be increased 3 mm or 1.5 mm on the maxillary arch and 1.5 mm on the mandibular arch (Figure 5). Figure 6 shows how the prosthetic space has been established and marked with ridge crest lines and the occlusal plane was established with virtual compensating curve template. In the sagittal view, placement of the virtual template in relation to retromolar pads can be seen and evaluated (Figure 7).
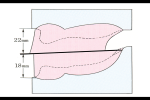
A maxillary intervestibular measurement of 22 mm and mandibular of 18 mm is used as in diagram of occlusal rims showing plane of occlusion in relation to retromolar pads (Figure 8).
With knowledge of all variables involved before prosthetic treatment has started, the clinician and technician will have the necessary information to design a treatment plan and create a virtual complete prosthesis that will exceed functional expectations.
When conducting a digital case plan and model analysis, the technician can assess the height, shape, and contour of residual ridges, and classify the throat form, all of which affect the design of a complete denture base. Another area that must be assessed during the model analysis is stability of the denture base under occlusal load. The mandibular bearing surface or area of support is much smaller than the maxillary edentulous arch. As the mandibular residual ridge extends to the posterior, the bone begins an upward plane toward the retromolar pad and ascending ramus (Figure 9). This inclined plane can contribute to instability of the mandibular complete denture if the occlusal forces are not distributed properly at a right angle to the area of support.
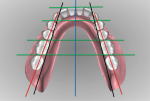
During the model analysis, the maxillary and mandibular posterior residual ridge relationship is analyzed for a cross-bite occlusion in the first molar area. According to Gysi, when the residual ridges were so resorbed that the inter-alveolar ridge line was inclined at less than 80 degrees to the horizontal, a cross-bite occlusal relationship existed.1 Sears wrote about the point of centralization where a line drawn on each opposing (maxillary and mandibular) ridge crest bisect represents where the maximum occlusal force can be exerted.2 This point is illustrated on mounted edentulous casts. In a Class-I and -II occlusal scheme, the point of centralization is usually in the second pre-molar or first molar region (Figure 10). In a Class-III scheme, these ridge crest lines usually do not bisect since the mandibular ridge is much broader than the maxillary edentulous ridge.
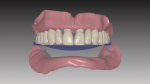
This initial model analysis provides information for inter-residual horizontal and vertical ridge relationships that is critical for proper tooth placement, increasing stability through functional complete denture occlusion, and evaluating restorative space for implant prosthetics. The maxillary anterior and posterior teeth are set to a virtual template in a lingualized occlusal scheme (Figure 11). In the facial view of maxillary teeth set to a virtual template, note how the posterior buccal cusp tips are raised 1 mm from the template (Figure 12). The mandibular teeth are arranged in relation to the ridge and virtual template (Figure 13). Completed maxillary and mandibular teeth are arranged with a gingival denture base (Figure 14).
Conducting a conventional cast or virtual model analysis, the ability to visualize then design tooth arrangement according to ridge relationships and vector forces is essential to improving stabilization of the maxillary and mandibular complete dentures (Figure 15). The ability to visualize an edentulous oral environment understanding where to place lost bone, tissue, and dentition in relation to the denture space is an important part of the creative prosthetic process (Figure 16). An advantage of digital models is the ability to analyze, evaluate, and design the denture before starting clinical treatment.
In evaluating the design, understanding where teeth must not be set is important to final outcome. As in Figure 17, a red line is drawn down the maxillary ridge crest and a blue line is drawn buccal to canines and ridge crest. On the left side, it's possible to see that the posterior teeth are set too far buccal outside of the blue line and directly over the vestibule. This position of the posterior teeth on the patient's left side will contribute to instability and palatal fracture from flexure in centric occlusion.
Evaluating the same digital design from a posterior perspective enables the technician to see the relation of maxillary posteriors to ridge and mandibular posteriors to ridge crest. A vertical blue line is drawn buccal to the ridge crest-denoting where the buccal surface of maxillary posteriors should be positioned-and a vertical red line bisects the ridge crest. The patient's left side could be set into a cross-bite relationship to improve stabilization of mandibular denture (Figure 18).
To achieve maximum stability, the mandibular posterior teeth are analyzed in relation to the retromolar pads and the ridge crest. Pound's line or triangle is an imaginary line drawn from the medial aspect of the retromolar pad to the mesial incisal line angle of the canine. All the lingual surfaces of the posterior teeth should come close to contacting this lingual line. The problem is that when severe residual ridge resorption exists, the lateral aspect of the pad can be lingual to the ridge crest. When this variable exists, such as on the patient's left side, this rule cannot be exactly followed. The first and second molars on the left side can be moved lingual, which will cause all the opposing maxillary teeth to be moved palatal as well (Figure 19). There is always a compromise when setting posterior teeth in situations like this where the retromolar pad is lingual to the ridge.
Conclusion
Creating a complete prosthetic digital case plan enables the technician and clinician to view the denture space and ridge relationship of an edentulous oral environment in a perspective that cannot be viewed with conventional methods. This digital design file can also be emailed for viewing and case plan evaluation, which is much faster and safer than shipping mounted stone casts from laboratory to dental office. Having the STL design files, a clinician can present an entire case plan to their patient from impressions to finished dentures, showing and explaining individual prosthetic variables during proposed treatment presentation. Digital diagnostics has changed how technicians and clinicians collaborate to provide optimal complete prosthetic treatment for a compromised edentulous patient.
Acknowledgement
The author would like to thank AvaDent Digital Dental Solutions for the design software used in this article.
About the Author
Robert Kreyer, CDT
Dentgnostix
Danville, California
References
1. Gerber A, Steinhardt G. Dental occlusion and the temporomandibular joint. Hanover Park, IL: Quintessence Publishing Co.; 1990.
2. Sears VH. Principles and technics for complete denture construction. London: Kimpton; 1949.