Esthetics in the Maxillary Arch and Function With the Mandibular Arch
A rationale for predictable treatment of the moderately worn dentition
When a motivated patient presents with a moderately worn dentition, the restorative dental team may see challenges, including determining the end point of treatment and how to achieve it. In the absence of a system for diagnosis and treatment, the team may miss information crucial to the predictability and longevity of the definitive restorations.1
An individualized risk profile is developed so that a treatment plan can be designed to address the areas of most significant risk without causing problems elsewhere.2 The dominant risk factors relating to esthetics and function drove this patient’s treatment plan. Restoring the maxillary arch satisfied the patient’s esthetic needs, and her functional compromises were remedied with the mandibular restorations (Figure 1 through Figure 3).
Diagnostic Findings
Findings from the clinical examination revealed multiple teeth had moderate erosion. All existing restorations had questionable prognoses, potentially from an occlusal etiology. All teeth had evidence of moderate attrition from normal forces. The patient had been using a nightguard and requested a new one due to her concern about the loss of tooth structure. However, a diagnosis of parafunction was ruled out due to the absence of horizontal notches in her nightguard and her negative responses in the functional section of her dental history form.
The maxillary and mandibular teeth required modification due to diastemas, rotations, and inappropriate length. The patient’s chief esthetic concerns were the loss of tooth length and color (Figure 4).
Treatment Plan
Initially, the Kois deprogrammer would be used to establish the mandibular treatment position of adapted centric relation. A wax-up at this position utilizing the Kois Dentofacial Analyzer (www.koiscenter.com) was fabricated, establishing the maxillary esthetic parameters, the posterior occlusal design, and the estimated final vertical dimension of occlusion (VDO).
The teeth would be prepared for IPS e.max (Ivoclar Vivadent, www.ivoclarvivadent.us) restorations—a posterior porcelain-fused-to-metal (PFM) fixed partial denture—and provisionalized using the wax-up as a guide. After delivery of the definitive maxillary restorations, a new deprogrammer would be fabricated and delivered.
An occlusion record could then be made and definitive mandibular restorations fabricated. At try-in of the mandibular restorations, the patient’s occlusion would be equilibrated, using the deprogrammer as a guide.
Phases
After the patient was fully deprogrammed, upper and lower casts and a bite record were made for the diagnostic wax-up fabrication.3
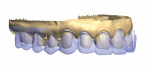
The Kois Dento-Facial Analyzer was used to communicate the position of the maxillary cast on the articulator to the dental laboratory. The casts were duplicated and both sets articulated. Utilizing a series of diagnostic photographs, a wax-up was fabricated, which established the appropriate lengths and positions of the final restorations, creating a roadmap for treatment (Figure 5 and Figure 6).
The first step in restoring the esthetics is to establish the maxillary incisal-edge position. After the mounting platform had been adjusted vertically on the articulator to reflect the desired final tooth length and maxillary occlusal plane, the maxillary anterior teeth were waxed. The maxillary posterior teeth were then waxed using the platform as a guide to level the occlusal plane. The esthetic parameters of the maxillary teeth were established, including the length and horizontal position of the teeth, the position and inclination of the midline, and the relative proportions of the teeth (Figure 7).
The lower model was then placed on the articulator. The final adjustment to the vertical dimension was determined by evaluating the length of the mandibular anterior teeth and the posterior occlusion from the patient’s photographs. The pin on the articulator was set to a vertical dimension that provided room to keep the mandibular anterior teeth at the predetermined length and level the posterior plane of occlusion.4 (While not necessary for this patient, some cases may require modification of the maxillary wax-up to balance compromises between the maxillary and mandibular occlusal planes and esthetic needs.) The posterior teeth were then waxed to achieve bilateral simultaneous contact—the treatment goal for occlusal stability (Figure 8).
The team determined that the most predictable treatment sequence would be to care for the maxillary arch first to satisfy the esthetic parameters. After seating the maxillary restorations, the lower arch could be restored to establish the vertical dimension and bilateral simultaneous occlusion—the functional parameters.
A matrix of the wax-up was used to create a template of the final result.5 This provided an opportunity for the patient to visualize the treatment endpoint and the dental team to generate a guide for tooth preparation. The teeth were prepared with depth cuts through the matrix, so tooth structure removal was kept to the minimum required for the final restorations and not determined by current tooth position.
The maxillary teeth were prepared for IPS e.max restorations. The preparations were designed to minimize the biomechanical risk to the teeth, provide adequate retention and resistance form, and allow sufficient space to satisfy the esthetic parameters of the restorative material (Figure 9 and Figure 10).
At the preparation appointment, the final impression of the maxillary preparations was made in a polyether impression material.6 Bite records were made of the upper preparations to the mandibular teeth to articulate the casts. After final adjustment of the provisional restorations, a model, occlusion record, and facebow record of the provisionalized maxillary arch were sent to the laboratory to communicate threedimensionally the esthetic outcomes desired. One week later, the mandibular teeth were prepared, an impression was made, and provisional restorations were fabricated. However, final restorations were not prescribed for the mandibular teeth (Figure 11).
Upon completion, the models were scanned into the 3Shape Dental Designer (3Shape, www.3shape.com), and a virtual design of the final crowns was developed utilizing the study model of the provisional restorations. The designs were then milled in wax for final processing as pressed e.max.
After pressing and fitting down the cores, they were prepared for final characterization and layering with a minimal cutback for the facial veneer layer of IPS e.max Ceram (Ivoclar Vivadent). All the natural incisal effects were created internally from materials in the Impulse kit. After final glaze and polishing, the fit surfaces were etched with 9% hydrofluoric acid and silanated in preparation for try-in and final cementation (Figure 12 through Figure 15).
Final maxillary restorations were returned for insertion. Under local anesthesia, the patient verified and accepted the fit and esthetics before final cementation. The restorations were cemented with RelyXTM Unicem Self-Adhesive Universal Resin (3M ESPE, solutions.3m.com), and occlusion was verified against the mandibular provisional restorations.
A study cast of the new maxillary restorations was made for the fabrication of a new Kois deprogrammer. The patient returned a week later for the final occlusal records of the maxillary restorations against the lower prepared teeth.
After fabrication, the fit, contacts, and esthetics of the definitive mandibular restorations were verified. After minor adjustment, the restorations were cemented with RelyX Unicem. The occlusion was adjusted to establish bilateral simultaneous posterior contacts utilizing the Kois deprogrammer. The chewing envelope was refined using 22-micron articulating tape (Figure 16 through Figure 22).
Conclusion
A comprehensive examination was completed and diagnostic risk profile was developed for this patient who presented with a moderately worn dentition. A treatment plan was established to return her to dental health. By establishing the esthetic parameters with the maxillary arch, the patient’s functional goals were finalized with the completion of treatment in the mandibular arch.
Acknowledgments
The authors would like to acknowledge the staff members at Prosthodontics and Implants NW and Protea Dental Studio, Inc, for their hard work and dedication to changing people’s lives.
References
1. Kois JC. New challenges in treatment planning: shifting the paradigm toward risk assessment and perceived value—part 1. Journal of Cosmetic Dentistry. 2011;26(4):62-69.
2. Kois JC. New challenges in treatment planning: shifting the paradigm toward risk assessment and perceived value—part 2. Journal of Cosmetic Dentistry. 2011;27(1):110-121.
3. Jayne D. A deprogrammer for occlusal analysis and simplified accurate case mounting. Journal of Cosmetic Dentistry. 2006;21:96-104.
4. Kois JC, Phillips KM. Occlusal vertical dimension: alteration concerns. Compend Contin Educ Dent. 1997;18(12):1997.
5. Kois DE, Schmidt KK, Raigrodski AJ. Esthetic templates for complex restorative cases: rationale and management. J Esthet Restor Dent. 2008;20(4):239-248.
6. Vakay RT, Kois JC. Universal paradigms for predictable final impressions. Compend Contin Educ Dent. 2005;26(3):199-200.
About the Authors
Leon Hermanides, CDT, graduated from College in South Africa with a National Higher Diploma in Dental Technology, the equivalent of a bachelor’s degree in the US. He has worked in South Africa, London, and Seattle laboratories, specializing in all stages of advanced reconstructions, implants, and anterior esthetics. Mr. Hermanides is a clinical instructor at the Kois Center and a member of study clubs around the Puget Sound area. He has served on the board of directors of the Washington State Dental Laboratory Association since 2005 and served as president in 2012. He is the chair of the Foundation for Dental Technology for 2014 and participates on the board of the National Association of Dental Laboratories and the Advisory Board for the Dental Technology program at Bates Technical College. Mr. Hermanides has lectured internationally to clinical and technical groups on subjects ranging from implant restorations to esthetics and restorative failures. In 1998, Mr. Hermanides established Protea Dental Studio in Redmond, Washington, which is a DAMAS-certified laboratory that specializes in providing comprehensive, implant, and anterior restorative cases.
Kim E. Larson, DDS, is a prosthodontist and practices in Puyallup, Washington at Prosthodontics and Implants Northwest. He graduated from Northwestern University Dental School in 1983, obtaining his DDS degree. In 1986, he graduated from Northwestern University Graduate Prosthodontic program, where he obtained his Certificate in Prosthodontics. For the past 11 years, he has been heavily involved at the prestigious Kois Center in Seattle, Washington. He is also a Kois Center graduate, mentor, clinical instructor, and recognized specialist.