Correction of a Single Discolored Anterior Tooth Due to Internal Resorption: A Clinical Report
Megan Todd, DMD; William Brackett, DDS; and Mario Romero, DDS
Abstract
For patients with a single discolored tooth who desire to have it lightened, a thorough examination and radiographic analysis need to be performed prior to initiating any bleaching treatment so that the cause of the discoloration can be determined. Underlying pathology, such as internal resorption, is often asymptomatic and difficult to diagnose and if left untreated could result in tooth loss. This article describes a case of a patient with a discolored maxillary central incisor resulting from internal resorption and the subsequent endodontic and bleaching therapy performed to resolve the pathology and achieve an acceptable esthetic result.
Single discolored anterior teeth present a difficult diagnostic and treatment planning challenge. It is important to diagnosis the underlying cause before initiating any treatment to correct the discoloration. Teeth discolor for a variety of reasons, such as caries, abscessed/necrotic pulp, failing restorations, or post-endodontic discoloration. However, the cause could also be a less frequently encountered pathology such as internal/external resorption, which is much more difficult to detect.1
While the exact prevalence of internal resorption is not well known,2 it is regarded as a rare and incidental finding, with approximately only 2% of cases presenting with symptoms.3 Several studies have reported that routine radiography does not always detect the presence of a resorptive lesion and does not show its true size.2,4,5 Recently, cone-beam computed tomography (CBCT) has gained popularity in endodontic diagnosis and treatment planning due to its ability to produce a 3-dimensional image allowing the clinician to evaluate the true nature and severity of the lesions.1,5 Treatment of resorptive lesions is very predictable and successful as long as the lesion does not perforate the canal walls.3,6
Several restorative options can be used to correct a single discolored anterior tooth, but the least invasive and most cost-effective one is bleaching.7,8 For endodontically treated teeth, both internal and external bleaching options exist; therefore, the clinician must weigh the benefits/risks associated with each and choose the appropriate method for the patient.9,10 In 35% to 50% of internal bleaching cases the esthetic effect will dissipate within 1 to 5 years, and the process will need to be repeated by removing the lingual access restoration, which can result in the removal of additional tooth structure.11 Additionally, about 7% of teeth that have undergone internal bleaching will develop external resorption defects.11 The cause for this is not well known; however, the patients in which external root resorption occurred tended to be younger than 25 and most had had a traumatic injury.10,11 Considering this information, external bleaching seems to be the safest method for teeth with internal resorption subsequent to trauma, particularly in young patients. Nightguard vital bleaching using 10% carbamide peroxide has been proven to be the safest and most efficacious method with the least side effects.7,8
This clinical report describes the diagnosis and treatment planning of a case of a discolored maxillary central incisor resulting from internal resorption and the subsequent endodontic and bleaching therapy performed to resolve the pathology and achieve an acceptable esthetic result.
Clinical Case Report
A 25-year-old Caucasian female patient with an unremarkable medical history noticed when reviewing photographs that her left maxillary central incisor was discolored (Figure 1). Prior to this, the patient had not noticed the discoloration. Her dental history revealed past orthodontic treatment and possible trauma due to a tubing accident.
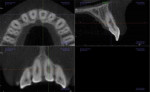
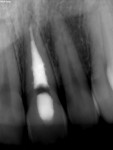
The initial clinical examination showed an intact crown with no caries or restorations present and a vital pulp. However, periapical radiographs revealed a well-defined symmetrical radiolucency, which ballooned out of the pulp chamber (Figure 2). No periapical lesion or widening of the periodontal ligament space was found. The patient had an endodontic consultation, which included an intraoral examination, shifted periapical radiographs, and a CBCT image (Figure 3), to assess the presence and type of resorption. CBCT imaging is crucial in differentiating between internal and external resorption and determining the extent of the lesion, which will affect the treatment plan and outcome.1,5
Electric pulp testing of the maxillary left central incisor was within normal limits, but the tooth exhibited a delayed response to cold. A diagnosis of asymptomatic irreversible pulpitis due to internal resorption with normal apical tissues was established. Two treatment options were presented to the patient: 1) nonsurgical root canal therapy (NSRCT) followed by internal bleaching; or 2) NSRCT with external bleaching. Due to the patient’s young age combined with her history of orthodontics and trauma, NSRCT with external bleaching was chosen to minimize the risk of external root resorption. Also, because of time constraints on the patient, the bleaching process was started prior to completion of root canal therapy.
To facilitate bleaching, a horseshoe shaped stone cast was made from an irreversible hydrocolloid impression of the patient’s maxillary arch.11 A vacuum-formed thermoplastic tray (Sof-Tray® 0.035”, Ultradent Products Inc, www.ultradent.com) was fabricated over the stone cast. The bleaching process was divided into two phases: phase one included a single-tooth tray, and phase two included a maxillary full-arch tray. The design for the single-tooth tray was non-scalloped, no-reservoir with the teeth molds on either side of the discolored tooth cut out (Figure 4). A pink mark was placed on the left central incisor on the stone cast to ensure the tray was not cut out in that area. The design for the full-arch tray was also non-scalloped, no-reservoir and covered all teeth in the patient’s maxillary arch. The patient was given 10% carbamide peroxide (Opalescence®, Ultradent Products Inc) bleaching gel and instructed to use the single-tooth tray, only applying bleaching gel to the left central incisor, and to wear the tray overnight for 2 weeks.
At the conclusion of phase one, the left central incisor was lighter than the adjacent teeth; therefore, the patient was instructed to use the full-arch tray and apply the bleaching gel to all maxillary teeth and wear the tray overnight for an additional 2 weeks. At the conclusion of phase two a uniform shade was achieved to the patient’s satisfaction (Figure 5 and Figure 6). The NSRCT was completed without any signs of canal wall perforation and the lingual access was restored with Kerr Premise composite resin shade A1 (Figure 7). A 1-year follow-up will be performed.
Discussion
This case presents a unique diagnostic and treatment planning challenge for the general practitioner. It emphasizes the importance of conducting a thorough clinical examination prior to initiating bleaching on a single dark tooth. Routine radiography, which usually includes only bitewings in a low caries-risk patient, would not have detected the pathology. In this case, the tooth was asymptomatic and the discoloration was so slight the patient did not notice it. The intraoral photographs taken were useful in initially diagnosing the discoloration, without which the pathology would have been undiagnosed for a longer time, making the treatment outcome and prognosis less predictable.
Internal resorption is inherently difficult to diagnosis because of its insidious nature and varying clinical presentation. It has been established that intraoral radiographs reveal limited information, which can lead to misdiagnosis and ineffective management of resorptive lesions.5 In recent years, a useful diagnostic tool has emerged for assessing the presence, type, and extent of resorptive lesions. CBCT allows the clinician to view the anatomy in three dimensions to confidently diagnose and manage the defect.1,5 For a non-perforating internal resorption defect, NSRCT is the treatment of choice and has been proven to have a high degree of success.6
Because the tooth in this case was previously unrestored with no caries present and well aligned in the arch, bleaching was the most conservative and suitable treatment to correct the discoloration.8 External bleaching with 10% carbamide peroxide was chosen over internal bleaching due to the potential risk for external cervical root resorption associated with internal bleaching combined with the convenience of an at-home bleaching regimen and the ability to achieve a customized predictable result.3,6,8,10 For the single-tooth tray design, the authors used the method described by Haywood and DiAngelis in which two teeth adjacent to the discolored tooth are cut out of the tray, ensuring the bleaching gel will only be applied to the single discolored tooth.12 After 2 weeks of using the single-tooth tray, the shade was not uniform throughout the arch so a maxillary full-arch tray was fabricated for the patient to wear for an additional 2 weeks.
After 4 weeks of external nightguard bleaching, both the patient and the authors were satisfied with the esthetic result and shade achieved (Figure 5 and Figure 6). The patient will have a 1-year follow-up to evaluate both the endodontic therapy and esthetic result.
Summary
This case highlights the importance of performing a thorough clinical examination and radiographic analysis prior to initiating bleaching treatment to correct a single discolored anterior tooth. There are several causes of discoloration where bleaching could mask the pathology and compromise the prognosis by delaying proper treatment. In cases where root resorption is suspected, obtaining a CBCT is recommended for establishing the diagnosis and determining the extent of the resorptive lesion. If the lesion is detected early, before it perforates the canal wall, treatment is predictable and the prognosis is favorable.
About the Authors
Megan Todd, DMD
Instructor
Department of Restorative Sciences
Dental College of Georgia at Augusta University
Augusta, Georgia
William Brackett, DDS
Professor
Department of Restorative Sciences
Dental College of Georgia at Augusta University
Augusta, Georgia
Mario Romero, DDS
Assistant Professor
Department of Restorative Sciences
Dental College of Georgia at Augusta University
Augusta, Georgia
References
1. Patel S, Dawood A, Wilson R, et al. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. Int Endod J. 2009;42(9):831-838.
2. Gabor C, Tam E, Shen Y, Haapasalo M. Prevalence of internal inflammatory root resorption. J Endod. 2012;38(1):24-27.
3. Thomas P, Krishna Pillai R, et al. An insight into internal resorption. ISRN Dent. 2014;2014:759326.
4. Patel S, Ricucci D, Durak C, Tay F. Internal root resorption: a review. J Endod. 2010;36(7):1107-1121.
5. Patel K, Mannocci F, Patel S. The assessment and management of external cervical resorption with periapical radiographs and cone-beam computed tomography: a clinical study. J Endod. 2016;42(10):1435-1440.
6. Caliskan MK, Turkun M. Prognosis of permanent teeth with internal resorption: a clinical review. Endod Dent Traumatol. 1997;13(2):75-81.
7. Ritter AV, Leonard RH Jr, St Georges AJ, et al. Safety and stability of nightguard vital bleaching: 9 to 12 years post-treatment. J Esthet Restor Dent. 2002;14(5):275-285.
8. Caughman WF, Frazier KB, Haywood VB. Carbamide peroxide whitening of nonvital single discolored teeth: case reports. Quintessence Int. 1999;30(3):155-161.
9. Plotino G, Buono L, Grande NM, et al. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008;34(4):394-407.
10. Zimmerli B, Jeger F, Lussi A. Bleaching of nonvital teeth. A clinically relevant literature review. Schweiz Monatsschr Zahnmed. 2010;120(4):306-320.
11. Summit JB, Robins JW, Hilton TJ, et al. Fundamentals of Operative Dentistry: A Contemporary Approach. 3rd ed. Chicago, IL: Quintessence; 2006:437-462.
12. Haywood VB, DiAngelis AJ. Bleaching the single dark tooth. Inside Dentistry. 2010;6(8):42-52.