Narrow-Diameter Implants: Dual Function as a Tent Pole for Vertical Ridge Augmentation and a Guide for Definitive Implant Position
Takanori Suzuki, DDS, PhD; Ismael Khouly, DDS, MS, PhD; Sang-Choon Cho, DDS; and Stuart Froum, DDS
Abstract:
Vertical bone defects present a challenge for the placement of implants in sufficient bone with proper position for a successful treatment outcome. This case report describes the use of a narrow-diameter (2.2 mm) implant as a tent pole for guided bone regeneration and documents the vertical bone augmentation achieved. In addition, following removal, the narrow-diameter implant served as a guide for the proper positioning and angulation of the final implant and its supporting restoration. The protocol and step-by-step procedure are described.
High degrees of success have been documented for dental implant restorations in patients who have fully and partially edentulous arches.1,2 In addition, the availability of ridge-augmentation procedures have clearly widened the scope of implant therapy. Presurgical site development is often necessary to allow implant placement in ideal positions for prosthetic restoration. However, successful bone augmentation of vertical maxillary and mandibular alveolar ridge defects is, in many cases, difficult to achieve.
Various techniques have been described for the reconstruction of alveolar defects. Among these, guided bone regeneration (GBR) has been documented as a predictable approach.3-6 However, GBR has been reported to be more successful for horizontal augmentation compared with vertical.7 Autogenous onlay block grafts,8-11 GBR with reinforced membranes or titanium mesh,12,13 distraction osteogenesis,14 and a combination of these15-17 are alternatives capable of regenerating vertical height. However, these techniques have disadvantages that include requiring a secondary surgical procedure, exposure of the membrane or mesh, risk for neurosensory damage, and technique sensitivity.12-15
Marx et al18 described a viable option for restoring the severely resorbed mandible through the simultaneous placement of endosseous dental implants to serve as tent poles with an autogenous corticocancellous bone graft. Bach et al19 successfully gained vertical height by using titanium screws in combination with particulate human mineralized allografts in a “tenting” fashion to augment alveolar ridges. Recently, Fontana et al7 used stainless-steel miniscrews (6 mm to 12 mm in length) as tenting screws to support the titanium-reinforced expanded polytetrafluoroethylene (e-PTFE) membrane to maintain space for bone regeneration in vertical-ridge augmentation. With this technique, they were able to maintain space and minimize the resorption of the bone-graft materials. They reported a mean increase of 4.02 ± 1.53 mm in vertical augmentation. However, these techniques have increased the risks for improper placement and malposition of dental implants, as well as a higher risk for dehiscence, which may result in total failure of the implants and grafts.
Similar tent-pole concepts can be applied using narrow-diameter implants (NDIs). Narrow-diameter implants (category 1, < 3.0 mm in diameter) were introduced as transitional implants to support immediately loaded provisional restorations in a single-stage surgery.20-25 Achieving high levels of stability with sufficient length when anchored into natural bone, these NDIs were designed to be removed at the end of the provisionalization and replaced with definitive implants.26,27 However, NDIs can be used clinically not only for fixed provisionalization and space maintenance, but also as guides for proper position and angulation of the final implants.
The purpose of this case report is to describe a step-by-step technique for the use of an NDI as a tent pole in a GBR procedure and its additional use as a guide for proper positioning and angulation of the final implants.
Clinical Case Report
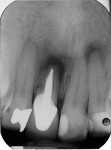
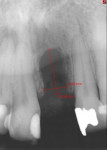
A 57-year-old man presented to Ashman Department of Periodontology and Implant Dentistry at New York University in New York, New York. The patient’s chief request was to have an implant placed in the maxillary central left incisor area (tooth No. 9). The patient had no history of systemic disease, radiation or chemotherapy, smoking, or periodontal disease. The patient’s dental history revealed that root-canal treatment and an apicoectomy had been performed on tooth No. 9 2 years previously. However, as a result of therapy, the tooth was structurally compromised and needed to be extracted (Figure 1 through Figure 3). Four months after the extraction (Figure 4 and Figure 5), radiographic scan findings revealed vertical bone loss of 10.9 mm and normal position of the interproximal-bone height on the adjacent teeth (Figure 6). A complete examination of oral hard and soft tissues was conducted, and a treatment plan was formulated in conjunction with the treating restorative dentist. Computerized tomographic scans, diagnostic casts, wax-ups, and surgical templates were prepared. The patient was educated about the surgery and signed an institutional review board-approved informed consent form. The clinical protocol to treat this defect utilized an NDI as a tent pole and implant guide. The step-by-step procedure was performed as follows.
The patient was prescribed 2 grams of amoxicillin (TEVA Pharmaceuticals, tevausa.com) 1 hour prior to surgery. Local infiltration anesthesia was obtained using 2% lidocaine with 1:100,000 epinephrine (Henry Schein, henryschein.com). A crestal incision was made, followed by 2 vertical releasing incisions on the distal aspects of teeth Nos. 8 and 10. These incisions extended apically to the mucogingival junction. A full-thickness mucoperiosteal flap was raised exposing a Class 3 ridge defect28 that extended 5.8 mm horizontally and 10.9 mm vertically (Figure 7). The initial osteotomy was made considering optimal angulation and position for the planned final implant. Using a surgical stent fabricated from an ideal wax-up, a 1.3-mm-diameter needle drill (CePo, Dentatus, dentatususa.com) at 1500 rpm with copious irrigation was employed to a depth of 4 mm in the existing natural bone. Decortication was performed on the buccal plate using a No. 1 round diamond bur with high-speed and copious irrigation. An NDI (Smart Slim, EBI North America, ebiimplantusa.com), 2.2 mm in diameter and 16 mm in length, was placed 5.8 mm into the existing natural bone, leaving 10.2 mm of the NDI exposed (Figure 8). Measurements mitutoyo.comof the exposed NDI were made with an electric caliper (Absolute Snap Caliper Series 573, Mitutoyo, mitutoyo.com) to the nearest 0.01 mm. A GBR procedure was performed simultaneously with NDI placement. A contoured nonabsorbable titanium-reinforced membrane (Cytoplast™ barrier membrane Ti-250, Osteogenics Biomedical, osteogenics.com) with small-particle (0.25 mm to 1.0 mm) anorganic bovine bone mineral (ABBM) (BioOss®, Geistlich Pharma North America, geistlich-na.com) were used to treat the defect. Chromic gut 4.0 sutures (Henry Schein) were used to secure the membrane to the periosteum (Figure 9). Tension-free primary closure was achieved using 4.0 chromic gut resorbable suture material for closure of the crestal incision. Interrupted sutures using 5.0 chromic gut were used to close the vertical incisions. A radiograph was made to evaluate the NDI position (Figure 10). The patient was monitored with 4- to 5-week follow-up appointments during the next 4 months.
Following a healing period of 6 months, a crestal incision was made slightly palatal to the previous incision, followed by intrasulcular incisions on the adjacent teeth. This procedure was performed under local infiltrate anesthesia using 2% lidocaine with 1:100,000 epinephrine. A full-thickness mucoperiosteal flap was reflected only in the crestal area in order to avoid exposure of the buccal plate (Figure 11). The titanium-reinforced membrane was cut with a 15C blade and surgical scissors to create a round 4-mm-diameter hole to accommodate implant placement. Bone formation was observed immediately apical to the membrane. The NDI was removed using an implant adapter connected to a counter torque ratchet. Prior to NDI removal, the amount of the NDI still exposed was measured to the nearest 0.01 mm with the same digital caliper. This enabled a precise measurement of the amount of vertical bone augmentation achieved. The permanent implant, with a 4.1-mm platform in diameter and 14 mm in length, (SLActive®, Straumann, straumann.us), was placed following the long axis of the explanted NDI. The permanent implant engaged 3 mm to 4 mm of the patient’s native bone (Figure 12). Implant stability (>35 Ncm) was established with a torque wrench. A radiograph was taken to check the position of the implant (Figure 13). An implant platform-level impression was created to fabricate the provisional restoration (Figure 14). Interrupted sutures were placed using 4.0 chromic gut (Henry Schein) to close the incisions. The patient was given prescriptions for 0.12% chlorhexidine gluconate oral rinse to be used twice daily for 2 weeks and an antibiotic (amoxicillin) 500 mg tid for 1 week. After final implant placement, the patient was monitored with routine surgical follow-up for 3 to 4 months. Six months following implant placement, a small crestal incision was made slightly toward the palatal side and a screw-retained provisional crown was inserted. After the desired soft-tissue contour was obtained, the final crown was delivered (Figure 15 through Figure 17).
Following treatment, the patient was monitored with maintenance visits every 3 months. Soft and hard tissues were evaluated at 3 years and at 5 years following placement of the final crown. Probing depths were 3 mm or less, no bleeding on probing was observed, and stable bone and soft-tissue level were noted (Figure 18 through Figure 23). Composite restoration was applied on mesial sides of tooth No. 8 and the mesial aspect of tooth No. 9 for closing the black triangle between teeth Nos. 8 and 9 (Figure 24).
Results
This patient with a severe localized vertical ridge defect of 10.9 mm received treatment with tent-pole/NDI-guided procedure. The vertical augmentation that was obtained measured 10.9 mm. Adequate tension-free closure over the grafted area was achieved, and no postoperative wound infections occurred. The implant has been maintained with stable bone and soft-tissue levels for 3 years.
Discussion
Bone remodeling after tooth extraction results in horizontal and vertical bone loss.29,30 Depending on the anatomic position and size of the defect, different surgical techniques can be performed to improve the bone volume of the implant site. Many authors have reported on the use of autogenous bone grafts to restore bony defects and to allow for the correct positioning of implants.3-5,8,9,11,15,16,18,31 However, when treating a severely atrophic alveolar ridge, it is common to encounter large-volume 3-dimensional defects that must be fully reconstructed to create an esthetic and functional result. To reconstruct these large-volume defects, obtaining autogenous bone from extraoral sources is often necessary. However, with the GBR tent-pole technique reported by Marx et al, by appropriately placing titanium screws interposed by particulate graft, it was possible to augment large vertical ridge defects with no need for the use of autogenous bone. This technique involved expanding the soft-tissue volume and using fixtures as “screw tent poles” for the surrounding particulate graft. This helped to prevent the soft tissues from collapsing over the particulate graft and subsequently displacing the graft, thus avoiding a compromised outcome.18 In the present case report, ABBM particles were used as the grafting material. These particles were hydrated with saline for approximately 1 to 2 minutes prior to placement to allow adhesion of the graft material. The membrane then covered, contained and compressed the graft against the natural bone.32,33 The graft served to allow space maintenance for the titanium-reinforced nonresorbable d-PTFE membrane. This was shown in a study by Urban et al34 to result in stable regeneration of bone in cases of vertical ridge augmentation. The anorganic bovine bone mineral acted as a scaffold for new bone formation. A histologic study35 in humans showed ABBM placed around implants had 70.3% of the particle surfaces covered by mature bone, as shown in biopsies taken 14 to 80 months after implant placement with simultaneous grafts.
Berglundh and Lindhe36 studied the osteoconductive potential of ABBM when placed in large self-contained defects in the mandibles of beagle dogs. Following 3 to 7 months of healing, the defect had been eliminated and the graft particles had become surrounded and, in part, substituted by parallel-fibered and lamellar bone. In addition, Simion et al37 utilized a composite graft consisting of 1:1 ratio of ABBM and autogenous bone for the vertical ridge augmentation. They observed the composite bone graft underwent slower resorption and substitution by new bone. Schlegel et al38 compared the resorption rate of autogenous bone and ABBM during sinus-floor elevation procedures. The loss of bone volume after a 6-month period was 15% and 40% for ABBM and autogenous bone, respectively. Therefore, bone substitutes with less postoperative resorption than autogenous bone have become an option for grafting procedures. Furthermore, in addition to restoring the hard-tissue defect, the particulate bone supported and augmented the soft-tissue architecture. This allowed for proper implant placement and improved the esthetic result.
The primary advantages of using the procedure described in the present case report is the excellent volume of vertical augmentation achieved, diminished treatment time, correct position and angulation of the final implant, and preexisting natural bone anchorage. Buser et al4 reported bone formation using a nonresorbable membrane after healing for 7 to 13 months, prior to implant placement. When placed simultaneously with GBR and a nonresorbable membrane, implants positioned into grafted bone have been shown to require a healing period of 8.5 months. In the current case, the NDI was used as a tent pole and the membrane was kept in place at the time of implant placement to maintain its biologic function. The nonresorbable titanium-reinforced membrane used in this procedure also prevented perforation of the NDI. In this case report, a conventional implant was placed while the bone material was maturing. This allowed the clinician to place the final implant not only in optimal position and angulation but also in the patient’s preexisting natural bone. All these advantages are achieved by placing the final implant following the same 3-dimensional path used to insert the NDI. Stage II surgery 4 months post implant placement revealed successful osseointegration of the definitive implant, which then allowed the removal of the nonresorbable membrane.39
Based on the previously cited study, which showed histologic results in humans, the ABBM particles showed little, if any, resorption at 14 to 80 months post placement.35 In another study on sinus augmentation, ABBM was compared with autogenous bone (AB) only and an 80:20 mixture of ABBM and AB. Up to 10 years, the ABBM showed significantly less resorption than the other 2 graft materials.40 Therefore, in the present case, minimal, if any, resorption would be expected after membrane removal. The literature has shown nonresorbable membranes have high degrees of success in GBR procedures. However, a statistically significant number of cases have shown soft-tissue dehiscences,7,41 which can occur at 2 different stages of the healing process. During the early stages, they are usually caused by a lack of tension-free primary closure. This may compromise the entire graft. Conservative treatment is appropriate, including oral hygiene maintenance and oral rinsing, for the remainder of the healing period. In the current case, proper fixation of the membrane and tension-free primary closure played key roles in avoiding these soft-tissue complications. Primary stability of the NDI was achieved by inserting it in 5.8 mm of native bone. In a study that included 3 human case reports, tenting screws positioned in 3 mm of native bone remained in place with enough stability for sufficient time to form new bone using GBR treatment.42
Another major complication that could affect the success rate of the tent-pole technique is infection at the surgical site.7 Although the risk for developing an infection of the grafted area is low, caution is advised. Depending on the stage that the infection occurs, the final outcome of the surgical procedure may be compromised. Wound dehiscence and infection of the site are 2 highly related complications in augmentation procedures. These were avoided in the current case with judicious use of antibiotics and complete flap coverage of the grafted defect.
Conclusion
The present case report demonstrated the use of an NDI as a tent-pole/implant guide for ridge augmentation. This technique resulted in successful reconstruction of a large-volume defect, permanent implant placement in the proper position and angulation, and anchorage of the implant in the patient’s own natural bone. However, more studies with long-term follow-up are needed to evaluate the stability of the graft and implants after implant loading. In addition, more cases using the present protocol with NDIs as tent poles in GBR augmentation procedures are necessary to determine the predictability of this new procedure.
Disclosure
Dr. Cho is a consultant for EBI North America.
About the Authors
Takanori Suzuki, DDS, PhD
Clinical Assistant Professor
Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York City, New York
Ismael Khouly, DDS, MS, PhD
Clinical Assistant Professor
Department of Oral and Maxillofacial Surgery, and Associate Director
Bluestone Center for Clinical Research
New York University College of Dentistry
New York City, New York
Sang-Choon Cho, DDS
Clinical Assistant Professor and Director of Advanced Program in Implant Dentistry
Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York City, New York
Stuart Froum, DDS
Clinical Professor and Director of Clinical Research
Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York
Private Practice
New York City, New York
References
1. Buser D, Mericske-Stern R, Bernard JP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997;8(3):161-172.
2. Bornstein MM, Schmid B, Belser UC, et al. Early loading of non-submerged titanium implants with a sandblasted and acid-etched surface. 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res. 2005;16(6):631-638.
3. Buser D, Dula K, Belser UC, et al. Localized ridge augmentation using guided bone regeneration. II. Surgical procedure in the mandible. Int J Periodontics Restorative Dent. 1995;15(1):10-29.
4. Buser D, Dula K, Hirt HP, Schenk RK. Lateral ridge augmentation using autografts and barrier membranes: A clinical study with 40 partially edentulous patients. J Oral Maxillofac Surg. 1996;54(4):420-432.
5. Buser D, Dula K, Hess D, et al. Localized ridge augmentation with autografts and barrier membranes. Periodontol. 2000;19:151-163.
6. Simon BI, Von Hagen S, Deasy MJ, et al. Changes in alveolar bone height and width following ridge augmentation using bone graft and membranes. J Periodontol. 2000;71(11):1774-1791.
7. Fontana F, Grossi GB, Fimanò M, Maiorana C. Osseointegrated implants in vertical ridge augmentation with a nonresorbable membrane: a retrospective study of 75 implants with 1 to 6 years of follow-up. Int J Periodontics Restorative Dent. 2015;35(1):29-39.
8. Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12(6):767-776.
9. Rasmusson L, Meredith N, Kahnberg KE, Sennerby L. Effects of barrier membranes on bone resorption and implant stability in onlay bone grafts. An experimental study. Clin Oral Implants Res. 1999;10(4):267-277.
10. Proussaefs P, Lozada J, Rohrer MD. A clinical and histologic evaluation of a block onlay graft in conjunction with autogenous particulate and inorganic bovine mineral (Bio-Oss): a case report. Int J Periodontics Restorative Dent. 2002;22(6):567-573.
11. Keller EE, Tolman DE, Eckert S. Surgical-prosthodontic reconstruction of advanced maxillary bone compromise with autogenous onlay block bone grafts and osseointegrated endosseous implants: a 12 year study of 32 consecutive patients. Int J Oral Maxillofac Implants. 1999;14(2):197-209.
12. Louis PJ, Gutta R, Said-Al-Naief N, Bartolucci A. Reconstruction of the maxilla and mandible with particulate bone graft and titanium mesh for implant placement. J Oral Maxillofac Surg. 2008;66(2):235-245.
13. Boyne PJ. Maxillofacial surgery. In Habal MB, Reddi AH, eds. Bone Grafts and Bone Graft Substitutes. Philadelphia, PA: W.B. Saunders; 1992: 291.
14. Jensen OT, Cockrell R, Kuhike L, Reed C. Anterior maxillary alveolar distraction osteogenesis: a prospective 5- year clinical study. Int J Oral Maxillofac Implants. 2002;17(1):52-68.
15. Thor A. Reconstruction of the anterior maxilla with platelet gel, autogenous bone, and titanium mesh: a case report. Clin Implant Dent Relat Res. 2002;4(3):150-155.
16. Simion M, Jovanovic SA, Tinti C, Benfenati SP. Long-term evaluation of osseointegrated implants inserted at the same time or after vertical ridge augmentation. A retrospective study on 123 implants with 1-5 year follow-up. Clin Oral Implants Res. 2001;12(1):35-45.
17. Fugazzotto PA. Report of 302 consecutive ridge augmentation procedures: technical consideration sand clinical results. Int J Oral Maxillofac Implants.1998;13(3):358-368.
18. Marx RE, Shellenberger T, Wimsatt J, Correa P. Severely resorbed mandible: predictable reconstruction with soft tissue matrix expansion (tent pole) grafts. J Oral Maxillofac Surg. 2002;60(8):878-888.
19. Le B, Rohrer MD, Prasad HS. Screw “tent-pole” grafting technique for reconstruction of large vertical alveolar ridge defects using human mineralized allograft for implant site preparation.,i. 2010;68(2):428-435.
20. Klein MO, Schiegnitz E, Al-Nawas B. Systematic review on success of narrow-diameter dental implants. Int J Oral Maxillofac Implants. 2014;29 (suppl):43-54.
21. Petrungaro PS: Fixed temporization and bone-augmented ridge stabilization with transitional implants. Pract Periodontics Aesthet Dent. 1997;9(9):1071-1078.
22. Altar MS, el Shazly D, Osman S, et al. Study of the effect of using mini-transitional implants as temporary abutments in implant overdenture cases. Implant Dent. 1999;8(2):152-158.
23. Bohsali K, Simon H, Kan JY, Redd M. Modular transitional implants to support the interim maxillary overdenture. Compend Cont Educ Dent. 1999;20(10):975-983.
24. Petrungaro PS. Reconstruction of severely resorbed atrophic maxillae and management with transitional implants. Implant Dent. 2000;9(3):271-277.
25. Bichacho N, Landsberg CJ, Roher M, Davidovich Y. Immediate fixed transitional restoration in implant therapy. Pract Periodontics Aesthet Dent. 1999;11(1):45-51.
26. Zubery Y, Bichacho N, Moses O, Tal H. Immediate loading of modular transitional implants: a histology and histomorphometric study in dogs. Int J Periodontics Restorative Dent. 1999;19(4):434-453.
27. Froum SJ, Simon HH, Cho SC, et al. Histological evaluation of bone implant contact of immediately loaded transitional implants after 6 to 27 months. Int J Oral Maxillofac Implants. 2005;20(1):54-60.
28. Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part II. Prosthetic/periodontal interrelationships. Compend Contin Educ Dent. 1983;4(6):549-562.
29. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005;32(2):212-218.
30. Cardaropoli G, Araújo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 2003;30(9):809-818.
31. Proussaefs P, Lozada J, Rohrer MD. A clinical and histologic evaluation of a block onlay graft in conjunction with autogenous particulate and inorganic bovine material (Bio-Oss): a case report. Int J Periodont Restor Dent. 2002;22(6):567-573.
32. Romanos GE, Delgado-Ruiz RA, Gómez-Moreno G, et al. Role of mechanical compression on bone regeneration around a particulate bone graft material: an experimental study in rabbit calvaria [published online ahead of print April 12, 2015]. Clin Oral Implants Res. doi: 10.1111/clr.12592.
33. Delgado-Ruiz R, Romanos GE, Alexandre Gerhke S, et al. Biological effects of compressive forces exerted on particulate bone grafts during socket preservation: animal study [published online ahead of print August 2, 2016]. Clin Oral Implants Res. doi: 10.1111/clr.12942.
34. Urban IA, Lozada JL, Jovanovic SA, et al. Vertical ridge augmentation with titanium-reinforced, dense-PTFE membranes and a combination of particulated autogenous bone and anorganic bovine bone-derived mineral: a prospective case series in 19 patients. Int J Oral Maxillofac Implants. 2014;29(1):185-193.
35. Jensen SS, Bosshardt DD, Gruber R, Buser D. Long-term stability of contour augmentation in the esthetic zone: histologic and histomorphometric evaluation of 12 human biopsies 14 to 80 months after augmentation. J Periodontol. 2014;85(11):1549-1556.
36. Berglundh T, Lindhe J. Healing around implants placed in bone defects treated with Bio-Oss. An experimental study in the dog. Clin Oral Implants Res. 1997;8(2):117-124.
37. Simion M, Fontana F, Rasperini G, Maiorana C. Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (Bio Oss). Clin Oral Implants Res. 2007;18(5):620-629.
38. Schlegel KA, Fichtner G, Schultze-Mosgau S, Wiltfang J. Histologic findings in sinus augmentation with autogenous bone chips versus a bovine bone substitute. Int J Oral Maxillofac Implants. 2003;18(1):53-58.
39. Blanco J, Alonso A, Sanz M. Long-term results and survival rate of implants treated with guided bone regeneration: a 5-year case series prospective study. Clin Oral Implants Res. 2005;16(3):294-301.
40. Mardinger O, Chaushu G, Sigalov S, et al. Factors affecting changes in sinus graft height between and above the placed implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(1):e6-e11.
41. Fontana F, Maschera E, Rocchietta I, Simion M. Clinical classification of complications in guided bone regeneration procedures by means of a nonresorbable membrane. Int J Periodontics Restorative Dent. 2011;31 (3):265-273.
42. Chasioti E, Chiang TF, Drew HJ. Maintaining space in localized ridge augmentation using guided bone regeneration with tenting screw technology. Quintessence Int. 2013;44(10):763-771.