Digital Mandibular Arch Restoration at an Increased Occlusal Vertical Dimension in One Visit
Nancy E. Hartrick, DDS; and Steven R. Acker, MS, DDS
ABSTRACT
This case demonstrates how a fully digital technique was used to restore the mandibular arch to proper function and improved esthetics. The initial treatment plan to restore implants replacing the lower right molars had to be altered due to space limitations. A direct deprogrammer was utilized to determine the proper jaw relationship at an acceptable occlusal vertical dimension. A computer-aided design system was employed to digitally create and fabricate implant/abutment-supported cement-retained lithium-disilicate crowns, tooth-supported lithium-disilicate crowns, and screw-retained hybrid abutment lithium-disilicate crowns in one visit.
This case demonstrates how preoperative diagnosis and planning strategies were used to achieve a predictable restorative result in one visit for a patient who traveled several hundred miles for her care. Prior to her visit and treatment, a review of her dental records revealed a condition of minimal interocclusal space so a treatment plan for two screw-retained implant-supported hybrid abutment/crowns was developed. During digital scanning, it became apparent an alternative, more comprehensive treatment plan was needed to provide the final treatment in one visit. Utilizing digital technology, a chairside-fabricated anterior deprogramming jig, and sound functional concepts, a team of three—one dentist (NH) who did the treatment planning and provided chairside and digital treatment, another dentist (SA) who aided in the digital workflow, and a Patterson Dental specialist who assisted in digital design and laboratory support—worked together to increase the patient’s occlusal vertical dimension (OVD) and thereby gain sufficient clearance to successfully restore the patient’s posterior mandibular occlusion and tooth No. 22.
Clinical Case Overview
A 59-year-old recently retired patient (Figure 1) asked the treating dentist for care and would be traveling nearly 360 miles for her clinical evaluation and treatment. Previous to this request, her maxillary arch had been restored in 2012. The patient was functioning with an acrylic screw-retained provisional on implant Nos. 30 and 31 (5.0 NobelReplace Select™, Nobel Biocare, nobelbiocare.com) and was “tired of chewing on plastic,” she said. Given that the patient lived far away, the dental team planned to use digital scanning and in-office milling to create and deliver restorations for implant Nos. 30 and 31 in one visit.
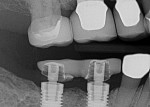
Records from her local surgeon and dentist were requested. Radiographic review (Figure 2) and emails from her regular dentist prompted concern about a lack of adequate interocclusal space for final restorations. Due to limited space, screw-retained hybrid abutment/crowns were planned.
Diagnosis
Medical History
The patient was a healthy 59-year-old female, who reported successful hip replacement surgery in 2011 and a history of annual physicals. Her current medications were Synthroid (levothyroxine sodium tablets) and estradiol, a form of estrogen. Her American Society of Anesthesiology classification was 2, due to hypothyroidism. This indicated she had mild systemic disease with no functional limitation.
Dental History
The patient listed her oral health as good, and she had been receiving regular care by her local dentist for the past 4 years with no reported dental anxiety. Slight gingival recession was present, and she reported a family history of periodontal disease. The patient frequently had food catch between her teeth and had a history of broken teeth. She stated that her lower anterior teeth had become more worn in the past 5 years. She was a gum chewer and had been given a nightguard more than 6 years ago because her dentist thought she had nighttime bruxism. She had worn the appliance briefly, but ceased. She was pleased with her smile from the 2012 maxillary restoration and was aware of the darker shade of the lower teeth and crowns. Improving this appearance was not her immediate priority.
Diagnosis, Risk Assessment, and Prognosis
Periodontal: Generalized horizontal bone loss less than 3 mm was noted, except for teeth Nos. 14 and 15, which had isolated infrabony defects and 5-mm probing depths. She had minimal bleeding on probing. Her periodontal diagnosis was generalized type AAP II, localized AAP III.
Risk: Medium
Prognosis: Generalized good with a fair prognosis for the upper left molars
Biomechanical: The patient had an extensive history of restorative dentistry and a period of high caries susceptibility as a young adult (Figure 3). Except for teeth Nos. 23 to 26, all remaining teeth were structurally compromised. Tooth loss, except for the third molars and first bicuspids, was from biomechanical causes. The maxillary arch had been restored in 2012, and a healing abutment was in place on implant No. 13. On the mandibular arch, a screw-retained acrylic provisional on implant Nos. 30 and 31 (Figure 4), cemented crowns over implant abutments on implant Nos. 18, 19, and 20, and porcelain-fused-to-metal crowns on teeth Nos. 22 and 29 were present. The restorations on Nos. 18, 22, and 29 were defective, and those on teeth Nos. 25 and 27 were questionable. Erosion was noted on tooth No. 24.
Risk: High
Prognosis: Poor for Nos. 2, 14, 15, 18, 22, 27, and 29. Fair for teeth Nos. 23 to 26.
Functional: The patient said she had perceived her lower anterior teeth had changed in the past 5 years, but a photograph from 2008 showed minimal alteration (Figure 5). Minimal incisal tooth structure loss on teeth Nos. 23 to 27 was suspected to be initially from extrinsic erosion and secondarily from normal attrition. The acrylic screw-retained provisional restoration on implant Nos. 30 and 31 was thin; no information was available on the original design and contour. She reported no difficulties in chewing and had no temporomandibular dysfunction. The load and immobilization test findings were negative, and she had a normal range of motion. The functional diagnosis was acceptable function.
Risk: Low
Prognosis: Generalized good with poor prognosis for the provisional restoration
Dentofacial: The patient exhibited high maxillary lip dynamics. The mandibular lip dynamics were medium, and dark lower teeth and restorations were present. The vertical height of the posterior mandibular occlusal plane was lower than that of the mandibular anterior teeth (Figure 6). If additional interocclusal space was needed to functionally restore the lower right implants, increasing the OVD by increasing the height of the mandibular posterior teeth would be acceptable esthetically.
Risk: Maxillary high, mandibular medium
Prognosis: Maxillary good, mandibular poor due to darker shade
Treatment Plan
The plan was to remove the provisional restoration on implant Nos. 30 and 31, and then design and fabricate two restorations. Next the dental team would deliver the fabricated screw-retained hybrid abutment/crowns on implant Nos. 30 and 31 at the current OVD in one visit. If a change in OVD was necessary, the team would utilize a chairside anterior deprogramming jig to locate the jaw relation position and OVD.1 The jig would remain in place throughout almost the entire appointment, ensuring the correct OVD and jaw-relation position were maintained.2
If the OVD needed to be changed, milled e.max® (Ivoclar Vivadent, ivoclarvivadent.com) porcelain crowns for implant Nos. 18 to 20 and teeth Nos. 22 and 29 would be required. For an efficient workflow, implant Nos. 18 to 20 would be restored first because completing the cemented restorations would require fewer steps than the screw-retained hybrid abutment crowns on implant Nos. 30 and 31.3
Treatment Sequence
Stage 1
The treatment began with taking preoperative photographs and performing a clinical examination. Following removal of the lower right provisional and placement of the ScanPosts (Dentsply Sirona, sironausa.com) and ScanBodies (Dentsply Sirona) (Figure 7), a digital impression was taken of each arch and a buccal bite registration. During the CEREC™ (Dentsply Sirona) computer-aided design process, the team realized insufficient interocclusal space existed to create hybrid abutment crowns (Figure 8) at the current OVD. Removal of porcelain from the opposing arch was not an option. The decision was made to gain space by increasing the OVD, employing the revised treatment plan. The implant-supported provisional was then hand torqued back onto implant Nos. 30 and 31 to prevent tissue collapse during treatment.
An anterior deprogramming jig was fabricated between incisal edges of the lower central incisors to function as a direct deprogrammer. The jig design incorporated the principles of an indirect Kois deprogrammer, with a flat 3-mm-wide platform to determine the orthopedic position of the mandible at the desired new OVD. IPS Empress® Direct composite (Ivoclar Vivadent) was used chairside to create the jig utilizing traditional bonding protocol. On closing, the patient quickly established a single, reproducible point of contact on the platform, with no slide or deviation. This position remained comfortable throughout the procedure with no tenderness in her jaw muscles or joint.
Stage 2
Stage 2 was creation of the implant abutment-supported cemented crowns for implant Nos. 18 to 20.4 The existing crowns were removed, using an electric handpiece, and the tissue was retracted with No. 2 retraction cord to access and take images of the existing abutment margins (Figure 9). The CEREC Omnicam (Dentsply Sirona) was used for digital impressions of the upper and lower left quadrants and a buccal bite registration while the jig provided a stable stop at the desired OVD.
Crowns were designed using the CEREC acquisition unit and e.max crowns milled with the CEREC MC XL (Dentsply Sirona) in office milling machine. The milled crowns (Figure 10) in the noncrystallized blue state were tried in; contacts and occlusion were checked and adjusted as needed. Next, appropriate stains were applied to the noncrystallized crowns to match existing restorations, followed by an even covering layer of spray glaze prior to crystallization in the Programat oven (Ivoclar Vivadent), which allowed glazing and crystallization to occur simultaneously. The 15-minute process in the oven induces the proper shade and significantly increases the restoration’s flexural strength5 to 400 MPa. Compared with other monolithic glass ceramics used for chairside computer-aided design and computer-aided manufacturing fabricated restorations, this is over 2.5 times the flexural strength.6
Following 5 minutes of cooling, the crowns were steam cleaned; tried in to confirm proper fit, function, and esthetics; and cemented onto the existing implant abutments with Premier® Implant Cement™ (Premier, premusa.com) providing for retrievability. Removal of excess cement and occlusal evaluation with thin articulating paper was done to verify equal-intensity contact of restorations on Nos. 18 to 20 coincident with contact on the anterior deprogramming jig. Proper, stable occlusion at the correct OVD was now established on the left side.
Stage 3
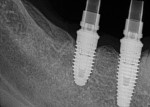
Stage 3 involved screw-retained hybrid abutment crowns on implant Nos. 30 and 31 with an e.max crown on tooth No. 29.7 The provisional restoration on implant Nos. 30 and 31 was removed and images of the soft tissue coronal to the implants were taken to capture the contours for designing the proper emergence profile of the final restorations. Two ScanPosts were placed into the implants, and full seating was confirmed radiographically (Figure 11). An appropriate ScanBody was seated over the ScanPost specific to the implant system and diameter, to digitally transfer the exact position of the hex on the integrated implant. Tooth No. 29 was prepared according to biomechanical principles and tissue packed with No. 00 and No. 2 retraction cords.
Similarly to the left side, an upper- and lower-right quadrant digital impression and a buccal bite registration were taken. E.max restorations for Nos. 29 to 31 were digitally designed. The emergence profile for the implant abutments was designed with the soft-tissue scan taken prior to the placement of ScanBodies.
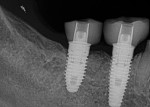
Once milled, the fit of the two implant-supported restorations onto their TiBases (Dentsply Sirona) was confirmed. After oven crystallization and cooling, the implant-supported crowns were adhered to their TiBases with Multilink® Cement (Ivoclar Vivadent) to fabricate the screw-retained hybrid crowns for implant Nos. 30 and 31. They were hand torqued into implant Nos. 30 and 31; seating was confirmed radiographically (Figure 12). The hybrid abutment crowns were then torqued into place to 35 Ncm. Following a 10-minute wait, the screws were torqued again to 35 Ncm, with an awareness of the stretch of screw mechanics.8 Teflon tape was placed over the screw heads for protection and hybrid abutment crown access openings were sealed with shade A1 dentin Empress composite.
The e.max crown for tooth No. 29 was tried in, following standard treatment of using steam cleaning, hydrofluoric acid, and silane. The tooth surface was microabraded with PrepStart (Danville Materials, danvillematerials.com). Verification of acceptable fit, function, and esthetics was done prior to cementation with RelyX™ Unicem™ (3M, 3m.com). Occlusion was checked to confirm bilateral, simultaneous, equal-intensity contacts. The deprogramming jig was removed.
Stage 4
The final step was replacing the defective crown on tooth No. 22. After removal of the restoration and preparation following biomechanical guidelines, tissue packing was performed with No. 000 and No. 00 retraction cords. The restoration design, fabrication, and delivery were done by the treating dentist (NH), as previously described.
A final evaluation of occlusion and marginal integrity was performed. Stable occlusion was confirmed using thin articulating paper with the patient seated at a 45-degree angle. The occlusal goal of bilateral, equal intensity, simultaneous contacts was verified. The chewing envelope was evaluated with the patient seated upright, chewing on 200-µm-thick blue articulating paper. Minor adjustments of interferences on inclines were made, and the porcelain was polished. After the anesthetic had worn off, the patient was able to feel her bite and could chew comfortably. The patient said she was pleased with the results both functionally and esthetically (Figure 13 through Figure 15).
Conclusion
When treatment plans need to be developed prior to clinical examination, the clinical team must be prepared to adapt to unexpected clinical findings to avoid disappointing the patient during treatment. By combining sound principles of diagnosis and treatment planning,9 with computer-aided design and computer-aided manufacturing technology, a systematic workflow can be developed that provides a predictable approach and successful result. In this case, the outcome exceeded the patient’s expectations and provided satisfaction for all involved. In one visit, her mandibular posterior occlusion and tooth No. 22 were properly restored at an increased vertical dimension that was comfortable, functional, and esthetic. The total treatment took close to 6 hours with much of the time waiting for milling and crystallization of the material in the oven. Her periodontal and functional risks were not adversely impacted, while her functional and dentofacial prognosis and biomechanical risks and prognoses were improved by the treatment provided. The patient has been successfully functioning for 19 months. Her local dentist delivered the restoration for implant No. 13 in May 2015.
ACKNOWLEDGMENTS
The authors (NH) and (SA) wish to thank the Kois Center in Seattle, Washington, as well as the staff and volunteers for their guidance and support. Appreciation also is extended to Kayleigh Bedell, Office Manager at Hartrick Dentistry, for assistance in preparation of the article. Additionally sincere appreciation is extended to Jonathan Acker, Patterson Cerec™ Specialist, who enthusiastically and diligently participated in accomplishing the successful result.
ABOUT THE AUTHORS
Nancy E. Hartrick, DDS
Private Practice, Royal Oak, Michigan; Clinical Instructor, Kois Center, Seattle, Washington
Steven R. Acker, MS, DDS
Private Practice, Staten Island, New York; Attending Brookdale Hospital and Medical Center, Brooklyn, New York; Clinical Instructor, Kois Center, Seattle, Washington
References
1. Jayne D. A deprogrammer for occlusal analysis and simplified accurate case mounting. The Journal of Cosmetic Dentistry. 2006;21(4):96-102.
2. Kois JC, Phillips KM. Occlusal vertical dimension: alteration concerns. Compend Contin Educ Dent. 1997;18(12):1169-1174, 1176-1177; quiz 1180.
3. Bynum JH. Clinical case report: testing occlusal management, previewing anterior esthetics, and staging rehabilitation with direct composite and Kois deprogrammer. Compend Contin Educ Dent. 2010;31(4):298-302, 304, 306.
4. de Kok P, Kleverlaan CJ, de Jager N, et al. Mechanical performance of implant-supported posterior crowns. J Prosthet Dent. 2015;114(1):59-66.
5. Shenoy A, Shenoy N. Dental ceramics: an update. J Conserv Dent. 2010;13(4):195-203.
6. Fasbinder DJ, Dennison JB, Heys D, Neiva G. A clinical evaluation of chairside lithium disilicate CAD/CAM crowns. J Am Dent Assoc. 2010;141 (suppl 2):10S-14S.
7. Kurbad A, Kurbad S. CAD/CAM-based implant abutments. Int J Comput Dent. 2013;16(2):125-141.
8. Siamos G, Winkler S, Boberick KG. Relationship between implant preload and screw loosening on implant-supported prosthesis. J Oral Implantol. 2002;28(2):67-73.
9. Kois DE, Kois JC. Comprehensive risk-based diagnostically driven treatment planning: developing sequentially generated treatment. Dent Clin North Am. 2015;59(3):593-608.