Novel Approach to Overcome Limitations Associated With Immediate Implant Placement: Osteotome Technique
Gabriel Strauss, DMD; Sonali Marfatia, BDS; Howard J. Drew, DMD; and Emil Cappetta, DMD
Abstract
This case series introduces a novel osteotome technique as an alternative to conventional drilling protocols for immediate fixtures. Immediate implant placement is associated with significantly less bone-to-implant contact, and navigating the anatomy of the socket can be difficult. Osteotomy drills remove already-limited bone following atraumatic extractions. The osteotome technique has been introduced as an alternative approach to prepare the osteotomy in the appropriate position relative to the socket apex and surrounding alveolar walls. The surgical technique and case reports demonstrating it are presented, highlighting the technique's benefits.
Since its introduction in 1978, immediate implant placement has become increasingly commonplace.1 Advantages of this approach include reduced treatment time, less surgeries, and prosthetically driven placement.2,3 The limitations of the use of immediate implants are insufficient bone volume, soft-tissue deficiency, incorrect angulation, and an improperly positioned implant platform.4-6 Early articles on immediate implant placement stated that the extraction site is a guide for the osteotomy7 and that the immediately placed implant will preserve the alveolar ridge.8 These assumptions may be questionable and will be further discussed in this article.
Many factors must be considered when attempting immediate implant placement, including the prosthetic plan, tissue biotype, width of the buccal plate, root angulation, residual ridge width, adjacent anatomical structures, and bone quality.5,9 Maxillary anterior buccal plates have been shown to have an average thickness of less than 1 mm, although buccal plates increase in width toward the posterior.10
Use of traditional drill sequencing for preparation of an osteotomy in a fresh extraction socket removes already-limited bone and does not improve bone quality.11 Additionally, the osteotomy drill tends to follow the original socket anatomy, and the length of the drill may limit the operator's vision, thus hampering parallelism.
The use of osteotomes was introduced to help achieve osseointegration in soft bone and aid in sinus membrane elevation. In the mid 1990s the advantages of the technique were maintaining present bone, expanding narrow alveolar ridges, and increasing bone density.12 More recently, advantages have been found to include increased peri-implant bone volume, higher bone-to-implant contact, and increased primary stability.13-15
The following case reports detail the use of osteotomes to prepare the osteotomy in immediate extraction sockets to overcome the limitations of immediate implant placement using a traditional drill sequence.
Surgical Technique
The surgical procedure may be completed under local anesthesia. Single-rooted teeth are removed by creating a trough in the periodontal ligament (PDL) space using a thin tapered diamond bur followed by a periotome. Multi-rooted teeth are typically sectioned prior to removal. Complete degranulation of the socket is then performed.
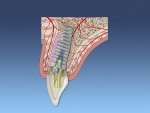
The palatal or lingual wall is scored with a round diamond bur along the palatal wall, away from the apex of the extraction site, to reduce the chance of buccal apical perforation of the implant (Figure 1). If the bone is soft, often this step can be skipped and the clinician can begin the osteotomy with the osteotomes.
The smallest size osteotome is then initially used to prepare the osteotomy. The osteotome instrument can be visualized emerging from the socket, which can ensure parallelism with the adjacent crowns. Larger osteotomes are used to increase the width of the osteotomy based on the implant diameter and condense the apical and lateral bone (Figure 2). The angulation of the osteotome can easily be changed depending on the desired prosthesis (ie, screw- or cement-retained). In cases of type II bone it is recommended that the assistant hold the patient's forehead to minimize any discomfort from the mallet. The final shaping drill may be used if more than 5 mm of apical bone is present past the extraction apex.
The dental implant can then be placed for the desired prosthetic restoration (Figure 3 through Figure 5). The authors recommend placing a bone graft between the implant and surrounding walls. With routine postoperative care, increased risk of complications is minimized.
Case 1
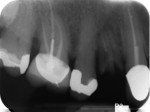
A 68-year-old man was referred to the Department of Periodontology at Rutgers School of Dental Medicine (RSDM) in Newark, New Jersey. The patient's medical history revealed no systemic contraindications for dental treatment. Clinical examination revealed remaining root tips in the maxillary right first premolar (Figure 6). The root tips were extracted using periotomes and luxators without elevating a flap.
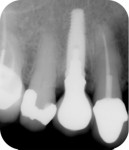
The osteotomy was initiated with a high-speed handpiece and round diamond bur. Osteotomes were then used sequentially to prepare the osteotomy (Figure 7). During the procedure the osteotomes were placed through the occlusal surface of the surgical guide to ensure ideal placement for a screw-retained prosthesis. A 4/3 x 13 mm platform-switched implant was placed. The insertion torque of the implant was greater than 45 Ncm, with an implant stability quotient (ISQ) reading of 72. It was decided to fabricate an immediate temporary crown with no occlusal interferences.
A cover screw was placed and the buccal gap was grafted with bone allograft (Figure 8). The temporary crown was torqued to the recommended 20 Ncm; it acted as a seal for the bone graft material.
Postoperative medications included amoxicillin 500 mg three times a day for 7 days and ibuprofen 600 mg 20 tablets every 6 hours as needed for pain. The patient was instructed not to function on the temporary crown during the healing phase.
The patient was seen for a 2-week follow-up and every 4 weeks after for supragingival debridement and oral hygiene reinforcement. After 4 months the final screw-retained prosthesis was delivered (Figure 9 through Figure 11).
Case 2
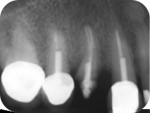
A 42-year-old woman with a noncontributory medical history was referred to the Department of Periodontology at RSDM. The patient's maxillary right first premolar was deemed nonrestorable due to a palatal vertical fracture (Figure 12). With no flap reflection, a long tapered diamond bur was placed in the PDL space and a trough was created on the proximal surfaces. Luxators were then used to remove the roots. After degranulation of the socket, the palatodistal wall was scored using a round diamond bur (Figure 13). An osteotome was then positioned to direct the fixture toward the distal wall to ensure parallelism with the adjacent roots and not follow the original socket anatomy (Figure 14).
A 4/3 x 13 mm fixture was placed at the crestal level (Figure 15 and Figure 16), and the buccal gap was grafted with bone allograft. A collagen sponge was placed over the site and two single interrupted sutures were used to contain the contents.
Postoperative medications included amoxicillin and ibuprofen and similar instructions were provided as in case 1. The final screw-retained prosthesis was delivered 5 months after tooth extraction (Figure 17 and Figure 18).
Discussion
This case series aimed to present an alternative technique for osteotomy preparation of an extraction socket. The placement of immediate post-extraction implants in conjunction with bone grafting is becoming increasingly routine. Dimensional changes of the alveolar ridge may be close to 50% following tooth extraction.16 Placement of immediate implants has been proposed to preserve the alveolar ridge.8,17 Other reports have disproven this assertion and recommend ridge preservation procedures even with the placement of an immediate implant.4,18
The exact direction of placement of the immediate implant has also evolved over the past 30 years. In 1989, Lazzara initially reported penetrating the apex of the socket to achieve the necessary primary stability.7 A recent cross-sectional cone-beam computed tomography (CBCT) analysis showed a greater likelihood of fenestration or dehiscence of the root apex of maxillary anterior and premolar teeth.10 A classification system of root position, based on CBCT, showed 78.8% of central incisiors were positioned more buccally in the alveolar housing.19 Another proposed classification system that investigated the ideal location for immediate implant placement determined that the socket was considered not to be an optimum channel for implant placement.20The placement of the immediate implant toward the palatal aspect of the socket is recommended to minimize esthetic complications of gingival recession.21 The proposed technique recommends scoring of the palatal bone with a round bur to create a new channel that will direct the osteotomes and eventual implant into the ideal position.
A major concern with immediate implant placement is the amount of bone remodeling that will occur following tooth extraction. Vignoletti and Sanz in 2014 noted a wide range of buccal bone resorption, from 0 mm to 3.14 mm, with immediate implant placement.18 They hypothesized that this heterogeneity was due to the thickness of the buccal bone after tooth extraction or to the amount of cortical bone present on the buccal. The implant position relative to the buccal bone may also be a factor in the amount of bone resorption. Araújo et al published multiple studies that showed the placement of immediate implants did not preserve the alveolar ridge dimensions. They concluded that placement of the implant close to thinner walls results in higher risk of compromised healing and possible loss of alveolar bone.22-24 Unlike a conventional osteotomy drill, which has a tendency to skip and follow the socket anatomy, the osteotome instrument can be visualized in the desired position throughout the site preparation and can ensure parallelism with the adjacent crowns.
Qahash et al reported that if the buccal bone is 2 mm or greater, it will remain after immediate implant placement.25 The dilemma is that other authors have reported that the anterior buccal bone thickness may be less than or equal to 1 mm in up to 90% of cases.26,27
Primary implant stability is directly related to insertion torque at the time of implant placement. Higher insertion torque values (ie, 25 Ncm to 45 Ncm) could resist micromovements, resulting in improved osseointegration and implant healing.28 However, excessively high implant insertion torque (ie, 50 Ncm to 100 Ncm) can accelerate the rate of bone resorption during implant integration.29 A recent in vitro study measured the insertion torque and resonance frequency analysis of implants placed with conventional drilling versus the osteotome technique.15 Implants placed with the osteotome technique showed a significantly greater insertion torque (45 Ncm) compared to conventional drilling (22 Ncm). The advantage of tapered osteotomes with concave tips is that they condense the lateral and apical bone, thus minimizing the removal of remaining bone. Histological studies have shown the densification of trabecular bone at the apex of implants inserted with the osteotome approach.13 Compression necrosis during osteotomy preparation with tapered osteotomes is minimized due to the slow incremental increase in the osteotomy site.
Conclusion
The osteotome technique allows more precise control and positioning by the clinician than conventional drilling protocols, because the concave tip of the instrument can engage and ensure proper buccopalatal placement of the implant for the desired prosthesis. The technique also improves the quality of the bone, thus increasing the stability of the immediate implant.
About the Authors
Gabriel Strauss, DMD
PGY-3, Department of Periodontics, Rutgers School of Dental Medicine, Newark, New Jersey
Sonali Marfatia, BDS
PGY-3, Department of Periodontics, Rutgers School of Dental Medicine, Newark, New Jersey
Howard J. Drew, DMD
Clinical Professor and Vice Chairman, Department of Periodontics, Rutgers School of Dental Medicine, Newark, New Jersey
Emil Cappetta, DMD
Assistant Professor and Postgraduate Director, Department of Periodontics, Rutgers School of Dental Medicine, Newark, New Jersey
References
1. Schulte W, Kleineikenscheidt H, Lindner K, Schareyka R. The Tübingen immediate implant in clinical studies. Dtsch Zahnarztl. 1978;33(5):348-359.
2. Rosenquist B, Grenthe B. Immediate placement of implants into extraction sockets: implant survival. Int J Oral Maxillofac Implants. 1996;11(2):205-209.
3. Schwartz-Arad D, Chaushu G. The ways and wherefores of immediate placement of implants into fresh extraction sites: a literature review. J Periodontol. 1997;68(10):915-923.
4. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31(10):820-828.
5. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(suppl):43-61.
6. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113-119.
7. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5):332-343.
8. Watzek G, Haider R, Mensdorff-Pouilly N, Haas R. Immediate and delayed implantation for complete restoration of the jaw following extraction of all residual teeth: a retrospective study comparing different types of serial immediate implantation. Int J Oral Maxillofac Implants. 1995;10(5):561-567.
9. Ferrus J, Cecchinato D, Pjetursson EB, et al. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010;21(1):22-29.
10. Vera C, De Kok IJ, Reinhold D, et al. Evaluation of buccal alveolar bone dimension of maxillary anterior and premolar teeth: a cone beam computed tomography investigation. Int J Oral Maxillofac Implants. 2012;27(6):1514-1519.
11. da Rosa JCM, Pertile de Oliveira Rosa AC, Huwais S. Use of the immediate dentoalveolar restoration technique combined with osseodensification in periodontally compromised extraction sites. Int J Periodontics Restorative Dent. 2019;39(4):527-534.
12. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15(2):152-158.
13. Shalabi MM, Wolke JG, Jansen JA. The effects of implant surface roughness and surgical technique on implant fixation in an in vitromodel. Clin Oral Implants Res. 2006;17(2):172-178.
14. Xing Y, Khandelwal N, Petrov S, et al. Resonance frequency analysis (RFA) and insertional torque (IT) stability comparisons of implants placed using osteotomes versus drilling techniques: a preliminary case study. Quintessence Int. 2015;46(9):789-798.
15. Tsolaki I, Tonsekar PP, Najafi B, et al. Comparison of osteotome and conventional drilling techniques for primary implant stability: an in vitro study. J Oral Implantol. 2016;42(4):321-325.
16. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-323.
17. Wilson TG Jr, Schenk R, Buser D, Cochran D. Implants placed in immediate extraction sites: a report of histologic and histometric analyses of human biopsies. Int J Oral Maxillofac Implants. 1998;13(3):333-341.
18. Vignoletti F, Sanz M. Immediate implants at fresh extraction sockets: from myth to reality Periodontol 2000. 2014;66(1):132-152.
19. Lau SL, Chow J, Li W, Chow LK. Classification of maxillary central incisors-implications for immediate implant in the esthetic zone. J Oral Maxillofac Implants. 2011;69(1):142-153.
20. Kan JY, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
21. Kahnberg KE. Immediate implant placement in fresh extraction sockets: a clinical report. Int J Oral Maxillofac Implants. 2009;24(2):282-288.
22. Araújo MG, Sukekava F, Wennström JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005;32(6):645-652.
23. Araújo MG, Wennström JL, Lindhe J. Modeling of the buccal and lingual bone walls of fresh extraction sites following implant installation. Clin Oral Implants Res. 2006;17(6):606-614.
24. Araújo MG, Lindhe J. Ridge preservation with the use of Bio-Oss collagen: a 6-month study in the dog. Clin Oral Implants Res. 2009;20(5):433-440.
25. Qahash M, Susin C, Polimeni G, et al. Bone healing dynamics at buccal peri-implant sites. Clin Oral Implants Res. 2008;19(2):166-172.
26. Huynh-Ba G, Pjetursson BE, Sanz M, et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res. 2010;21(1):37-42.
27. Braut V, Bornstein MM, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent. 2011;31(2):125-131.
28. Trisi P, Perfetti G, Baldoni E, et al. Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res. 2009;20(5):467-471.
29. Barone A, Alfonsi F, Derchi G, et al. The effect of insertion torque on the clinical outcome of single implants: a randomized clinical trial. Clin Implant Dent Relat Res. 2016;18(3):588-600.