Dental Implantology: Numbers Clinicians Need to Know
Gary Greenstein, DDS, MS; John Cavallaro, DDS; and Dennis Tarnow, DDS
Abstract
Dental implantology is a discipline that merges knowledge regarding treatment planning, surgical procedures, and prosthetic endeavors. To attain optimal results many numbers pertaining to different facets of therapy are integrated into treating patients. This article outlines a wide range of digits that may assist clinicians in enhancing the performance of implant dentistry. Important integers are presented in three segments related to the sequence of therapy: pre-procedural assessments, surgical therapy, and postsurgical patient management.
Numerous dental implant procedures can be facilitated by knowing numbers related to characteristics of biological structures, biomechanical relationships, and research data. Integers are like letters; alone they are meaningless, but when integrated into therapeutic endeavors they provide a relevant basis for procedural planning and execution of therapy. This article provides lists of digits that clinicians should be acquainted with when performing implant dentistry. Pertinent facts related to many presented integers are described. When several studies assessed a specific subject, important digits were selected to represent essential information. Some of the discussed numbers are means and are not intended to represent all responses that clinicians may experience when treating patients. Data are organized into three sections and discussed with respect to chronology of treatment: numbers related to pre-procedural assessments and treatment planning, integers to be used during surgical therapy, and digits related to postsurgical patient management.
SECTION I: NUMBERS RELATED TO PRE-PROCEDURAL ASSESSMENTS AND TREATMENT PLANNING
Periodontal and Peri-Implant Diagnostic Considerations
A. Probing Depth Evaluations
When interpreting probing measurements around teeth and implants, the following explanations should be considered:
1. Teeth: Probing depths of 1 mm to 3 mm are normal; 4 mm determinations reflect the gray zone; at 5 mm, there is concern, but not overly if tissues are pink, there is no bleeding on probing, and the probing depths are not getting deeper. At ≥6 mm probing depth, surgical intervention may be necessary if a patient persistently manifests inflammation or increased pocketing, despite conservative therapy.1
2. Implants: Desirable probing depths around dental implants are 2.5 mm to 4 mm, but deeper assessments can be associated with healthy peri-implant mucosa.2 In general, probing evaluations may be greater around implants than teeth, because there are no connective tissue fibers inserting into implants and connective tissue adhesions adjacent to implants do not impede probe penetration similarly to the connective tissue attachment to teeth.3
3. A gentle periodontal probing force of 25 grams or 0.25 Newtons (one Newton = approximately 100 gm forces) should be used to evaluate bleeding on probing.4 This force is roughly the pressure needed for a periodontal probe to blanch a fingernail.
B. Prognosticating Tooth and Implant Survival Based on the Amount of Alveolar Bone
1. Teeth: Despite periodontitis, teeth with 50% bone loss are not a clinical challenge to treat and retain.5 This contention is supported by numerous studies that addressed long-term retention of teeth with advanced bone resorption that were successfully treated.5-7 Ultimately, it is a judgment call as to the magnitude of bone loss and concurrent issues that condemns a tooth to extraction.
2. Implants: It has been suggested that if an implant manifests ≥50% bone loss it should be removed before additional bone resorption occurs.8 However, this threshold is not sacrosanct and therapy may be considered even if there is >50% bone diminishment around an implant.9
Furcation Locations: Maxillary and Mandibular Molars
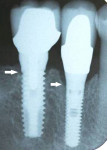
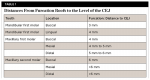
Knowing the depth and location of furcations aids in sectioning a tooth prior to extraction and helps avoid unnecessary loss of interradicular bone. The mesial maxillary molar furcation is located one-third of the way from the palate to the buccal side of a tooth, and the distal furcation is found half the span from the palate to the buccal (Figure 1). It is easier to probe maxillary furcations from the palatal aspect of teeth. Table 1 lists distances from furcation roofs to the level of the cementoenamel junction (CEJ).10
Endodontics
Non-vital teeth that have not undergone root canal therapy but are associated with other issues (eg, periodontitis, large apical pathosis) may be candidates for extraction and implant replacement or endodontic and periodontal treatment.
A. Incidence of Tooth Non-vitality After Crowns Are Prepared or Post Periodontal Surgery
During a 3- to 30-year period, 13.3% of teeth restored with crowns can become non-vital.11 Among patients with advanced periodontal disease, 9% of crowned and 2% of uncrowned teeth may develop non-vitality after periodontal surgery.12
B. Apicoectomies
Though the success and survival rates of teeth treated with apicoectomies may vary depending on different studies, apicoectomies have a success rate of around 74% and a survival rate of approximately 91%.13 Survival rates are higher because they denote retention of teeth that are non-symptomatic and may have residual apical radiolucencies. In contrast, success rates indicate that surgeries achieved complete apical radiographic bone fill. Another article reported that the success rate after retreatment of a failed apicoectomy is 36%.14 Currently, with use of mineral trioxide aggregate and microsurgical procedures the success rate of apicoectomies has significantly increased (88%).15
Esthetics
Assessing the clinical smile line and its relationship to papillary display is critical when planning anterior restorations.
A. Age Population: 20 to 30 Years Old
1. Average smile line: 75% to 100% of maxillary incisors are visible. 69% of patients have an average smile line.16
2. High smile line: Additional exposure of gingiva is noted. 11% of individuals have a high smile line, and this occurs two times more often among women than men.16
3. Low smile line: <75% of teeth are exposed. 20% of people have a low smile line.16
B. Age Population: 10 to 89 Years Old
In an older population, when patients are maximally smiling, display of midfacial gingival tissues and interdental papillae are seen as follows:
1. 72% of individuals have a low smile line (do not reveal midfacial gingival tissues) and 28% have a high smile line (demonstrate midfacial gingiva).17
2. 91% of all patients show their papillae when smiling.17
3. 87% of people with a low smile line reveal their papillae when they grin.17
4. In the group with high smile lines (28% of all patients), women show midfacial gingiva more often than men (76% vs 24%).17
Dimensions of Gingiva and Bone in the Esthetic Zone
A. Recognizing Differences Between Normal and Deficient Dimensions of Anatomic Structures Helps Treatment Planning
1. Buccal and lingual osseous crests are usually located 2 mm to 3 mm apical to gingival margins.18
2. Interproximally, maxillary anterior interdental bony crests are around 3 mm (range 2.1 mm to 4.1 mm) coronal to facial bone heights (Figure 2).19
3. Interproximally, between maxillary central incisors, the interdental papilla is 4.5 mm to 5 mm coronal to the osseous crest.20 This large papilla is due to papillary hypertrophy. Thus, maintaining supragingival fibers helps reduce or eliminate postsurgical papillary shrinkage.
4. In general, papillary size is around 40% of crown height.21
5. For maxillary anterior teeth, the mean gingival zenith position (GZP) distal to a vertically bisected midline is as follows: central incisors, 1 mm; lateral incisors, 0.4 mm; and canine GZP is at the midline.22
B. Dimensions of Teeth in Esthetic Zone
1. The length of a maxillary central incisor is usually 10 mm to 12 mm.23 Women's incisors are typically shorter than men's by 1 mm.23 Maxillary lateral incisors are 1 mm shorter cervically and incisally than central incisors. Canines are at the same level as central incisors cervically and incisally.24
2. Among the maxillary anterior dentition, the width of central incisors ranges from 7 mm to 10 mm (mean 8.5 mm), lateral incisors vary from 5.5 mm to 8 mm (mean 6.5 mm), and canines range from 6.5 mm to 9 mm (mean 7.5 mm).25
3. The three types of front teeth (central and lateral incisors, canine) manifest the "golden ratio" with respect to their height and width. The width of maxillary anterior teeth is about 81% of their height.23
4. Mean dimensions of proximal contact areas between maxillary anterior teeth are as follows: central incisors, 4.2 mm; central and lateral incisors, 2.9 mm; lateral incisors and canines, 2 mm; and canines and first premolars, 1.5 mm.26
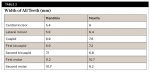
The widths of all teeth are listed in Table 2.27,28
Presurgical Medical Considerations
A. Platelet Count
Normal platelet count is 200,000 to 300,000 platelets per microliter of blood. Clinical problems can arise if the count is under 100,000. If it is less than 25,000 platelets per microliter, spontaneous bleeding can occur. Surgery should not be done until the platelet count is at least 60,000 or bleeding that is difficult to control may ensue.29
B. Medications That May Need to Be Suspended Prior to Implant Surgery
Patients should refrain from taking the following medications at certain times to exclude their effects on bleeding:
1. Though aspirin irreversibly affects platelets, it is usually unnecessary to avoid taking aspirin before dental surgery.30 However, for a procedure such as a sinus lift, it may be prudent to have a patient stop aspirin ingestion 5 to 7 days prior to surgery.
2. Plavix® irrevocably alters platelets but typically does not need to be suspended 5 to 7 days before dental surgery.30 However, the same precaution noted above applies to Plavix ingestion.
3. With a physician's permission, Coumadin® may or may be not be stopped or decreased 3 days prior to surgery.30
4. Pradaxa®, Xerelto®, and Eliquis®. These drugs must be abstained from for 2 days for them to have no effect. These medications sometimes are stopped for 1 day prior to surgery or not stopped. Refrain from these medications is done in accordance with a physician's recommendations. Half-life of these drugs are 13 hours; therefore, after 13 hours 50% of the drug remains, after 26 hours 75% is gone, after 39 hours 87.5% has been eliminated, and subsequent to 52 hours 93.75% of the drug has been removed.31
C. Steroid Utilization to Inhibit Edema
If it is anticipated that a surgical procedure will induce significant edema, steroid therapy may be initiated, unless medically contraindicated, a day prior to surgery to ensure there is an effective drug blood and tissue level. Several examples of steroid protocols are enumerated:
1. Medrol® Dosepak consists of 21 tablets, 4 mg, methylprednisolone; six are taken 1 day before surgery. Then, for the next 5 days, one less tablet is taken each day (5-4-3-2-1).32
2. Other techniques to prescribe steroids include: 40 mg of prednisone for 5 days; sequentially 50, 40, 30, 20, and 10 mg over 5 days; and 10 mg three times a day for 7 days.32,33 In general, titrating down steroids is unnecessary if the medication is taken less than 10 days.32
D. Pre-procedural Rinsing to Reduce Bacteria in Saliva and Aerosols
Microbes in saliva and bacterial aerosols caused by a handpiece or an ultrasonic tip can be reduced more than 90% by rinsing with chlorhexidine (0.12%)34 or Listerine® for 30 seconds before initiating therapy.35
Radiographs
A. X-ray Interpretations
1. A radiograph is a snapshot of one moment in time. Multiple films are required to demonstrate ongoing disease activity, and past bone resorption is not a sensitive indicator of future bone loss.36-38
2. Radiographs underestimate the magnitude of bone resorption 9% to 20%.36
3. Four mm of clinical attachment loss occurs before bone deterioration is detected around teeth on radiographs.37
4. A 30% to 40% decrease in bone mineralization occurs before alterations in bone density are detected on an x-ray.38
B. Radiographic Measurement Error
1. Bone level assessments using x-ray paralleling technique has a precision of around 0.5 mm.39 Thus, when radiographs taken with a Rinn holder are referred to as standardized, they actually are non-standardized and prone to error.
2. If a film holder allows 1 degree of vertical angular variation among serial films, this can result in a 0.17-mm error with respect to alveolar bone height.40
3. When the horizontal radiographic angulation is correct, the threads on an x-ray are clear on both sides of an implant. An incorrect radiographic angle of 10 degrees causes one side of an implant's threads to be blurry, and a 20-degree error results in no clearly visible threads.41
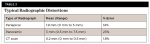
4. Radiographic distortions occur with different x-ray techniques. Typical distortions are listed in Table 3.42
Vertical Restorative Space Required for Different Types of Implant Prostheses
There is a 3-dimensional hierarchy of space required for different types of implant prostheses. Knowing restorative space requirements for each type of construct facilitates treatment planning. The minimum amount of vertical space needed from implant platform to the opposing dentition for components of different types of prostheses are as follows43,44: fixed screw-retained (implant level), 4 mm to 5 mm; fixed screw-retained (abutment level), 7.5 mm; fixed cement-retained, 7 mm to 8 mm; unsplinted overdenture, 7 mm; bar overdenture, 11 mm; fixed screw-retained hybrid, 15 mm.
Minimum Number of Implants Required for Mandibular and Maxillary Reconstructions of Edentate Arches
The treatment planning of implant prostheses is dependent on the number of missing teeth, availability of bone, and patient preferences.
Mandibular overdenture: Two implants for an implant-retained overdenture and four for an implant-retained and -supported overdenture.45 One implant can also provide some benefits.46
Mandibular fixed prosthesis: Four implants, but many clinicians prefer five or more implants.47
Maxillary overdenture: Four implants.48
Maxillary arch fixed prosthesis: Four implants, though many therapists advocate more.47
Anterior-posterior (A-P) spread: This is the distance from the center of the two most anterior implants to the distal aspect of the most posterior implants in the arch. Cantilever length that can be created distal to the implants bilaterally is determined by assessing the A-P spread and multiplying it by 1.5.49
Diameter of Implants
Increasing the diameter of an implant one size (eg, from 3.3 mm diameter to 4.1 mm diameter) increases the implant's surface area approximately 30%; this is equivalent to extending the implant's length by 3 mm.50
Length of Implants
Short textured implants can reliably support posterior prostheses. Nevertheless, implants with length less than 8 mm (4 mm to 7 mm) should be used cautiously, because they demonstrate greater failure risks compared to standard implants.51
SECTION II: INTEGERS THAT CAN BE USED DURING SURGICAL THERAPY
Anatomy
Awareness of anatomical dimensions is critically important for executing procedures in a safe and efficient manner. The following subsections provide important numbers related to anatomical structures.
A. Maxillary Sinus
1. The maxillary sinus is the largest of the paranasal sinuses. Typical dimensions are: height 36 mm to 45 mm, width mesio-distally 25 mm to 35 mm, and depth 38 mm to 45 mm (laterally-medially).52
2. The ostium's mean width is 2.4 mm.53 This is the opening between the maxillary sinus and the middle meatus of the nose.53 The mean distance from the antral floor to the ostium is 28.5 mm and the minimal extent is 20 mm.54 Thus, when a sinus lift is being performed, the Schneiderian membrane should not be elevated to a height that could occlude the ostium.
3. The quantity of pneumatization (internal sinus bone loss) that occurs under the sinus after an extraction is greater if multiple extractions are performed versus single extractions (2.22 mm vs 0.54 mm). Pneumatization usually happens within 6 months of an extraction.55
B. Intraosseous Artery Adjacent to the Maxillary Sinus
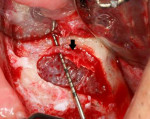
The artery in the lateral wall of the maxillary sinus is located within 16 mm of the osseous crest 20% of the time (Figure 3).56 This blood vessel is created by an anastomosis of the infraorbital and the posterior superior arteries. Thus, in 80% of patients, the artery's position is not a concern when performing a sinus lift. An anatomic study on cadavers identified this vessel in 100% of specimens; however, it could only be visualized in 53% of computed tomography (CT) scans.56
C. Mandibular Foramen and Canal
1. When administering a mandibular block injection, it is advisable to insert the needle into the pterygotemporal groove 6 mm to 10 mm above the occlusal plane,57 because the mandibular foramen is coronal to the occlusal plane 2.5% to 25% of the time.58,59
2. The mandibular canal is approximately 3.4 mm wide, and the inferior alveolar nerve is about 2.2 mm thick.60
3. The mandibular anterior loop is present in 71% of patients, and 5% of the time it is ≥5 mm long.61
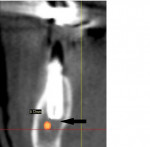
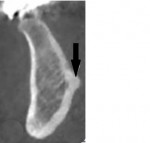
4. For safety, an osteotomy created over the inferior alveolar nerve should stop at least 2 mm from the nerve (Figure 4).62
5. One percent of mandibular canals bifurcate, inferior superiorly or medial-laterally, and this may not be seen on panoramic or periapical films.63
D. Size, Shape, Location of Mental Foramen
1. The shape of the mental foramen is round 34% to 45% of the time and oval 56% to 65% of the time. Its size (mm height/width) is: mean 3.47 mm, range 2 mm to 5.5 mm.64
2. The location of the mental foramen in the vertical plane with respect to the mandibular first bicuspid's apex is as follows (% of time at a location)65: apical to the apex, 46%; at the apex, 15.4%; coronal to level of the apex, 38.6%. For the second bicuspid the mental foramen is coronal to the apex 61.6% of the time. The finding that the foramen at the first and second bicuspid is often coronal to the apex dictates that caution must be exercised when placing an immediate implant in this location. It is prudent to assess a CBCT scan prior to implantation. Alternately, a delayed approach can be utilized for implant placement.
3. The mental foramen's horizontal locations differ among ethnic groups. In Caucasians, 70% of the time they are located between bicuspids, and among Asian Americans they are found above the second bicuspid in 59% of patients.62
4. The mean distance from alveolar crest to the mental foramen is 14 mm (non-resorbed ridge),66 and from mental foramen to the symphysis it is 25 mm.67
E. Hourglass-Shaped Mandibles
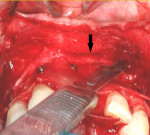
It is estimated that 3.9% of mandibles have an hourglass configuration (Figure 5).68 A cone-beam scan is necessary to detect this structure.
F. Submandibular Fossa
Submandibular concavities with a horizontal depth of 6 mm occur in 2.4% of assessed jaws.69 Approximately 52% of patients manifest lingual fossae that are 2 mm to 3 mm horizontally deep, and 28% demonstrate concavities >3 mm.70 If a large undercut is present, it may be prudent to place an instrument (eg, periosteal elevator) into and parallel to the concavity to facilitate drilling an osteotomy that avoids lingual plate perforation and entering the submandibular fossa.
G. Genial Tubercle
There is a superior and an inferior genial tubercle. Height of the superior genial tubercle is 6.17 mm and its width is 7.01 mm (Figure 6).71 Distance from apices of the lower central incisors to the superior tubercle is 15.4 mm.72 The genioglossus muscle attaches to the superior tubercle and should not be elevated off the tubercle when exposing the mandible to place an implant in a severely resorbed ridge.
H. Gingival and Palatal Tissue Thickness
1. Epithelium is 0.3 mm thick.73 In this regard, if a flap dehisces and the wound's edges have been apart for several days, epithelium should be scraped off the flap margins until bleeding points are detected (exposed connective tissue) before flaps are resutured.
2. Gingival thickness ranges from 0.53 mm to 2.62 mm (mean 1.56 mm).74
3. Palatal tissue thickness varies from 2 mm to 3.7 mm (mean 2.8 mm).75 The best location for harvesting a connective tissue graft is the maxillary premolar region or posterior tuberosity.
I. Nasopalatine (Incisive) Foramen
The nasopalatine foramen is located lingual to the central incisors and has a mean length of 8.1 mm. The nasopalatine nerve and descending palatine blood vessels exit the foramen (Figure 7). Within this structure, two incisive canals often are observed, however one to four may be seen. The mean width of the canal is 4.9 mm and the foramen is usually about 7.4 mm palatal to the buccal bony plate.
J. Distances to the Lingual Nerve From the Lingual Plate and Osseous Crest of the Mandible (Third Molar Region)
The horizontal distance is 2.06 mm, with a range of 0 mm to 3.2 mm; the vertical distance is 3.01 mm with a range of 1.7 mm to 4 mm.76 The lingual nerve is above the crest 14% of the time, and in 22% of patients it directly contacts the lingual plate.76
K. Other Key Anatomical Structures
1. The greater palatine foramen is usually located opposite the maxillary third molar (86% of the time) and is found between the second and third maxillary molars in 13% of patients.77
2. The infraorbital canal is located about 5 mm below the infraorbital notch.78
3. The Schneiderian membrane is around 0.8 mm thick.79
4. The width of the sublingual artery is approximately 2 mm.80
5. The width of the periodontal ligament averages 0.25 mm.81
6. Septa are found in 28.4% of all sinuses, and complete septa (horizontal and vertical) occur 0.3% of the time (Figure 8).82
Surgical Orthodontic Extrusion of Teeth
Sometimes a hopeless tooth with advanced recession and bone loss is not a useless tooth. With extrusion, reduced gingival and osseous levels can be restored to normal or improved prior to implant procedures. A tooth can be extruded about 1 mm to 2 mm per month, and its incisal edge should be equilibrated every 2 weeks.83 As the tooth is extruded, the sulcular epithelium everts and remains present for 28 to 42 days and then a new sulcus forms. After desired results are attained, the bone should be allowed to mineralize for 3 to 6 months before tooth extraction and implantation.83 The amount of needed tooth extrusion should be over-corrected by 25% to compensate for post-extraction bone resorption.83
Calculating Contents in Anesthetic Carpules
It is important to be able to compute the quantity of lidocaine and epinephrine in each carpule so dental anesthesia can be administered safely.
A. Lidocaine 2% in a Carpule
100 gm/100 ml is a 100% solution. 1 gm/100 ml = 1% solution = 10 mg/ml. A cartridge with 1.8 ml of 2% lidocaine contains 36 mg of lidocaine. A toxic dose of lidocaine is 500 mg.84 The recommended dose of lidocaine should not exceed 300 mg. Thus, eight carpules is a safe dose of 2% lidocaine. Anesthesia with lidocaine plus epinephrine usually lasts 2 to 3 hours.84
B. A Carpule With 1/100,000 Epinephrine
1 gm/100,000 ml = 1000 mg/100,000 ml = .01 mg/ml.84 A cartridge with 1.8 ml contains .018 mg of epinephrine. A therapeutic dose of epinephrine of 0.3 mg is given to cardiac arrest patients to stimulate their hearts. During dental procedures, the recommended level of epinephrine should not exceed 0.2 mg or approximately 10 carpules. Individuals who are sensitive to epinephrine should receive anesthetics that do not contain it (eg, Carbocaine®).84
C. 1/50,000 Epinephrine in a Carpule
A 1/50,000 epinephrine solution contains .02 mg/ml, which translates into .036 mg per 1.8 ml carpule.84 Therefore, 5.5 carpules containing 1/50,000 epinephrine (0.198 mg) is safe to administer to a patient who does not have cardiac issues. Note, the above maximal dosages addressing 2% lidocaine and epinephrine can be increased if procedures are prolonged.
D. Quantity of Anesthetic Solution Usually Needed to Achieve Dental Anesthesia
Infiltration: 1 ml; regional block: 1.5 ml; palatal block: 0.2 ml to 0.5 ml; long buccal block: 0.2 ml to 0.5 ml.85
Surgical Aids for Measuring Incision Depths
A. Blade Length
A #15 or #15c blade is 10 mm in length and can be used as a measuring device when harvesting a palatal connective tissue graft. For safety, when garnering a connective tissue graft, a distance of 2 mm should be left between the dissection's end and the greater palatine groove, which contains the greater palatine artery. Vault heights (CEJ to greater palatine groove) are: shallow vault (flat), 7 mm; average palate, 12 mm; and high vault (u-shaped), 17 mm.86
B. Blade Bevel
The periosteum is about 0.36 mm thick87; therefore, the bevel of a #15 or #15c blade that is 1 mm wide can be used as a depth guide when performing a periosteal fenestration to aid flap advancement (Figure 9).
Tooth Extraction Issues
A. Management of Perforations Into the Maxillary Sinus When Extracting Teeth
After an extraction, if a small hole into the sinus (≤2 mm) is present at the apical or lateral end of the socket, it can be ignored, because a clot will usually form and heal uneventfully. If a perforation is >2 mm, a piece of a resorbable barrier (eg, BioGide®, Geistlich, geistlich-na.com) should be placed over the puncture before bone grafting over it.88
B. Bone Resorption After Extractions
Six months after tooth removal that includes flap elevation, sockets manifest a mean 1.24 mm vertical bone loss (range 0.9 mm to 3.6 mm) and there is approximately 3.79 mm less horizontal bone (range 2.46 mm to 4.56 mm).89 In contrast, after a flapless extraction, there is approximately 1 mm vertical and horizontal bone loss.90
C. Dry Sockets
A small percentage of extraction sites (3.2%) develop a local osteitis after tooth removal, and this occurs most often in mandibular molar areas.91 Pain frequently manifests 3 days after an extraction.92 Patients may need to be medicated for 3 to 10 days to eliminate discomfort (eg, dry socket paste).
Resorption Time (in Months) for Submerged Collagen Barriers
Barriers are routinely used during guided bone regeneration procedures. Their degradation times vary: BioMend® (Zimmer Biomet, zimmerbiometdental.com), 2 months; BioMend® Extend™ (Zimmer Biomet), 4.5 months; BioGide® (Geistlich), 3 to 4 months; Ossix® (OraPharma, orapharma.com), 6 months; Resolute® (W.L. Gore & Associates, goremedical.com), 4 to 6 months; NeoMend (NeoMend Inc), 6 to 9 months.93 Other types of barriers are commercially available.93 Clinicians should note that if a resorbable barrier is left exposed to saliva, it deteriorates within several weeks.94
Degradation Time for Resorbable Sutures
After mucoperiosteal flap procedures, resorbable sutures usually are selected based on their duration of tensile strength: gut (5 to 7 days) or chromic gut (7 to 10 days). When it is desirable to retain stitches for 21 days (eg, guided bone regeneration procedures) vicryl sutures are often used.95 Other types of sutures are commercially available.95
Alveolar Bone
A. Unique Features of Bone
Several characteristics of bone need to be considered when treating patients. In cortical bone the percentage of bone porosities ranges from 5% to 10%; in trabecular bone the range spans from 75% to 95%.96 Porosity levels affect bone density and, thereby, drilling protocols for osteotomy development. Accordingly, when preparing an osteotomy, if bone does not feel dense, the osteotomy should be undersized to facilitate frictional retention to help achieve primary stability.96
Bone is 30% organic and 70% inorganic.96 It is the organic bone that allows ridges to expand when extracting teeth. Marrow spaces in trabecular bone range from 200 µm to 2000 µm (Figure 10), and when a marrow space is entered a bur may appear to sink without resistance.96
B. Types of Alveolar Bone Found in the Maxilla and Mandible
1. Thickness of cortical bone and feel of trabecular bone compared to innate objects: type I - cortical bone, feels like oak wood; type II - 2.5 mm to 4 mm cortical bone, dense trabecular bone's texture is like plywood; type III - 1.5 mm to 2 mm cortical bone, spongy trabecular bone's consistency is like soft pine wood; type IV - 1 mm or less cortical bone, sparse trabecular bone feels like balsa wood.97
2. Type I bone is not often detected. It is found most frequently in the anterior segment of the mandible (about 6% of the time).97
C. Bone Loss After Implant Placement
1. Bone resorption around non-platform-switched bone-level implants is usually 1.5 mm to 2 mm and occurs due to biologic width formation.98
2. Increased peri-implant bone loss occurs around platform-switched implants when the peri-mucosal tissue is <2 mm thick.99 Bone loss for thin (<2 mm) versus thick gingiva (≥2 mm) after implantation is, respectively, 1.17 mm versus 0.21 mm. This occurs regardless of the microgap's position.99
D. Bone Remodeling
The replacement rate of cortical and cancellous bone annually is, respectively, 7.7% and 17.7%.100 Others reported that 3% of cortical and 24% of cancellous bone remodel yearly.101 The numbers vary, but the trend is apparent. These data provide an explanation as to why medications that alter bone physiologically (eg, bisphosphonates) require extended time to be eliminated from the host.
E. Quantity of Circumferential Bone Desired Around an Implant
When flaps are used to help implant insertion into an intact ridge, if there is <1.8 mm circumferential bone around the implant, vertical bone height is lost.102 After implant placement it is suggested that there be at least 1 mm of bone circumferentially surrounding the implant.103
Biologic Width
Biologic width around teeth is approximately 2 mm and consists of 1 mm connective tissue and 1 mm of junctional epithelium.104 Its length ranges between 1 mm to 4 mm.105 Biologic width is usually supracrestal around healthy teeth and can be subcrestal or supracrestal around implants (1.5 mm to 2 mm height) (Figure 11). With respect to implants, the amount of induced bone resorption associated with biologic width formation depends on where implant collars are placed. Subcrestal collar placement results in more bone loss than supracrestal positioning.98 Upon placement, if an implant is submerged under soft tissue, the biologic width does not form; however, after it is exposed and an abutment is placed, biologic width develops in about 30 days.98
Bleeding Associated With Oral Surgery
A. Ecchymosis
As anesthesia wears off after dental surgery, if epinephrine is contained within the anesthetic there is vasodilation of blood vessels. If postoperative bleeding occurs, blood may advance along facial planes and cause an ecchymosis, whose pattern can vary. Tissue discoloration may appear adjacent to a surgical site or, due to gravity, extend down as far as the pectoral muscles (Figure 12). There is a predictable chronology of color change related to hemoglobin breakdown. Initially, tissue will appear reddish. After several hours, it may be black/blue. By day 6 its color changes to green (hemoglobin converted to biliverdin), and by day 8 to 9 it may be yellowish-brown (bilirubin present). In general, the body resorbs hemoglobin and hemoglobin by-products in 2 to 3 weeks.106
B. Blood Loss After Dental Surgery
An average person has around 5000 ml of blood (5 liters). One pint is 473 ml. After periodontal surgery that lasts less than 2 hours, blood loss is usually <125 ml (maxilla 110 ml, mandible 151 ml).107 Average hemorrhage per sextant is 134 ml (range 16 ml to 592 ml).107 If a patient's blood pressure drops 20 mg or blood loss is >500 ml, or there is an increased heart rate by 20%, intravenous solutions may be required.108
Torque Forces
A. Torque Forces Related to Procedures
The minimum torque that can be employed to attain primary stability is undefined.109 Forces ≥30 Ncm are routinely used to place implants into healed ridges and fresh extraction sockets prior to immediate temporization of implants.109 Increased insertion torque (≥50 Ncm) reduces micromotion, but does not appear to damage bone.109 The force generated by fingers when a screwdriver is used is 10 Ncm to 15 Ncm.109 Torque force used to place prosthetic screws is manufacturer-dependent and screws should be placed using a torque wrench.109
B. Implant Stability Quotient (ISQ)
ISQ ranges from 1 to 100. Investigators often use a threshold 65.5 ISQ to indicate primary stability, and implants that achieve this can be temporized.110
Platform Switching
A systematic review indicated that platform switching (abutment narrower than implant platform) results in less vertical bone loss around implants than implants restored without platform switching, respectively 0.055 mm to 0.99 mm versus 0.19 mm to 1.67 mm.111
Proper Distances Between Teeth and Implants and Between Implants
A. Span Between a Tooth and an Implant
This span should be at least 1.5 mm to 2 mm for non-platform-switched implants.112 Bone loss is inversely proportional to how close an implant is to a tooth.113
B. Minimum Space Between Two Implants
To maintain interproximal bone height for non-platform-switched implants, 3 mm is needed between the implants. If the expanse is ≤3 mm, the mean vertical bone decrease is 1.04 mm, and if the inter-implant space is >3 mm, the expected vertical bone resorption is 0.45 mm.114 Platform-switched implants can be placed slightly closer together. (At a 1 mm distance, the mean vertical bone lessening is 0.43 mm.)115
C. Space Required for a 4-mm Diameter Implant
To place a 4-mm diameter implant, a span of 7 mm mesiodistally is needed between adjacent teeth at the coronal region.116,117
Immediate Implant Placement
A. Maxillary Anterior Teeth
When placing an immediate implant in the maxillary anterior region, an osteotomy should be created that is half to two-thirds up the palatal aspect of the socket or 2 mm to 3 mm from the apex to utilize palatal bone of the socket to attain primary stability.118
B. Sink Depth
Ideally, an implant's platform should be placed 3 mm below the facial zenith of the soft tissue in the esthetic zone.119 This is referred to as the implant's sink depth (surgical term). Prosthetically, this distance is referred to as "running room" and it facilitates creation of an ideal crown emergence profile.
C. Tooth Position
1. A maxillary canine usually tilts 11 degrees distally and the root is distally dilacerated 32% of the time (Figure 13).120 Therefore, when replacing a maxillary first bicuspid with an implant, the implant should be placed parallel to the maxillary canine to avoid contacting the canine's apex.
2. Maxillary central incisors are positioned at about a 110-degree angle with respect to the horizontal plane of the palate.121
3. Mandibular posterior teeth are lingually inclined as follows: second bicuspid, 10 degrees; first molar, 15 degrees; second molar, 20 degrees.121
D. Gap Management (Also Referred to as the "Jumping Distance")
At the time of immediate implant placement, if the jumping distance between an implant and the adjacent bone is ≥2 mm, some clinicians recommend placing a bone graft into the gap.122 However, this is controversial, because others believe that a gap ≥2 mm, if left open, can fill with bone and heal by secondary intention.123
SECTION III: DIGITS RELATED TO POSTSURGICAL MANAGEMENT OF PATIENTS
Cold Therapy After Surgery
A. Customary Temperatures
Normal body temperature is 37°C; typical skin temperature is 33°C; and skin freezes at 25°C.124
B. Therapeutic Threshold Levels
Physiologic responses are attained if temperature is reduced as follows: blood flow decreases at 17°C; nerve conduction diminishes at 13.6°C; metabolism reduces at 10°C to 15°C; and edema is impeded at 12.8°C to 15.6°C.124
C. Duration of Time for Cold Application
Ice applied for 15 minutes on and 15 minutes off in a hand towel is recommended postsurgically for hours (precise number of hours is undetermined).124
D. Effective Distance of Cold Therapy
There is no change in skin temperature 1 cm proximal to ice application.124
Infections
A. Incubation Time for an Infection
An infection usually takes >2 days to manifest signs of redness, pain, etc.125
B. Time to Peak Edema
Edema peaks on the second or third day after surgery and needs to be differentiated from swelling associated with an infection. In general, edema is not painful upon palpation and decreases with time, whereas an infection is painful when touched and worsens if not treated.125
C. Tissue pH
The pH of normal tissue is 7.4 and infected tissue manifests a pH of around 5.5. Bone resorbs quickly in an acidic environment.126
D. Prophylactic Antibiotic Coverage
After implant placement, infections occur infrequently and antibiotic coverage does not reduce the incidence of postoperative infections in healthy patients.127 However, it has been suggested that clinicians prescribe a single dose of 2 gm of prophylactic amoxicillin, 1 hour before placing dental implants. If this protocol is followed for 25 patients, it prevents one person from experiencing an early implant failure.127
E. Time Necessary to Attain Blood and Tissue Levels of Antibiotics
If antibiotics are prescribed for an infection, it takes 24 to 48 hours to achieve a high tissue level; an affective blood level is attained within 1 hour.128
Rate of Healing After Surgical Procedures
A. Healing Time for Soft Tissues
There is a 12-hour lag time before epithelial healing commences after surgery, and then the healing extends at 0.5 mm to 1 mm daily from the wound's edges.129 Connective tissue regenerates approximately 0.5 mm per day.130
B. Time for Flaps to Become Bound Down
After surgery, initially a flap is attached to bone by a blood clot (for 0 to 24 hours). At 1 week, there is granulation tissue. After 2 weeks, a flap is connected to bone via immature collagen fibers. In a dog model, the force required to separate a flap from bone at 2 to 3 days postoperative is 225 grams, at 1 week it is 340 grams, and at 2 weeks a 1700 grams force could not displace the flap.131 In general, flaps are attached in 10 days (dog model). Sigma (healing speed) of dogs versus humans is 1.5 (faster in dogs). Thus, in humans it takes about 2 weeks for a flap to be strongly fastened to bone.
C. Post Extractions: Bone and Soft-Tissue Maturation
The following events occur after tooth removal: blood clot; granulation tissue is present in 96 hours; connective tissue is present by the 28th day; epithelium covers the socket after 5 weeks; woven bone exists at 3 months; and lamellar bone is present by 4 months.132
D. Bone Grafts and Osseointegration: Healing Time
1. Bone calcification advances 50 µm per day (1.5 mm per month).133
2. After a particulate bone graft is placed to regenerate a missing bony wall, 4 to 6 months is needed for graft calcification before an implant should be inserted.134
3. After a cortical block graft is placed, 4 to 5 months is required for bone healing.135
4. In type 4 bone, it is prudent to let an implant osseointegrate for 6 months before loading it.136
5. In dense bone, the clinician can load the implant in 3 months (or less) after its placement.137
6. Six months should be allowed for osseointegration if an implant is a "spinner" or if a transcrestal sinus floor elevation graft is placed in conjunction with an implant.137
7. Native bone below the sinus is composed of 25% bone and 75% marrow.138 Regenerated osseous bone after a lateral wall sinus lift consists of approximately 25% vital bone, 25% graft material, and 50% marrow.139 The regenerated bone does not have a higher percentage of vital bone than the bone adjacent to the graft site.139
8. Lateral window sinus lift bone graft mineralizes 1 mm to 2 mm bone per month from each bony wall.140
E. Contraction of Soft Tissue and Bone Grafts Postsurgically
Soft tissue and osseous grafts routinely diminish in size over time, and this should be factored in when performing therapy. The following are examples of the magnitude of shrinkage that occurs after graft procedures: gingival grafts are reduced 16.5% by 3 months141; connective tissue grafts may shrink 25% to 45% after 1 month142; 4 months subsequent to guided bone regeneration there is non-uniform contraction in bone graft height and width ranging from 39.1% to 76.3%143; and after a transcrestal sinus floor elevation, the sinus graft diminishes by 1.9 mm after 5 years.144
F. Repair After Nerve Damage
Specific terms are used to describe nerve injuries and the time necessary for their repair145:
1. Neurapraxia-This term denotes that there is no loss of nerve continuity; the nerve has been stretched, or underwent blunt trauma. Resultant paresthesia will subside and feeling will return in days to weeks.
2. Axonotmesis-The nerve is damaged, but not severed. Feeling usually returns within 2 to 6 months.
3. Neurotmesis-The nerve is severed. There is a poor prognosis for resolution of the induced paresthesia.
G. Reduction of Tooth Hypermobility After Therapy
When placing implants, there are occasions when teeth with periodontal issues adjacent to implant sites are treated concurrently. After scaling and root planing, a reduction of tooth mobility is usually noted after 2 weeks.146 After periodontal flap surgery the following events often occur: at 1 week, the level of tooth hypermobility may be increased; at 6 weeks postoperatively, tooth looseness may return to the preoperative level; and at 6 months, hypermobility may be decreased compared to immediately after surgery.147
Numbers Associated With Prosthetic Issues
A. Abutment Height
A 5-mm tall abutment is desired for retention of a cementable implant crown.148 The minimum abutment heights necessary to provide adequate retention for narrow-platform (3.5 mm) and wide-platform (5 mm) implants restored with single cement-retained restorations (cemented with Temp-BondTM, Kerr, kerrdental.com) are respectively, 3 mm and 4 mm.149 A 2 mm increase in abutment height amplifies retention by 40%.148
B. Occlusal Clearance Necessary for Different Restorative Materials
At least 2 mm of space is required to provide room for porcelain-fused-to-metal (PFM) occlusal materials (opaque, 0.3 mm; metal, 0.5 mm; and porcelain, 1 mm).150 Monolithic zirconia or lithium-disilicate crowns (press or CAD/CAM) require less vertical space than PFM crowns. This is due to the fact that restorations made with these materials need as little as 1 mm occlusal clearance, because no space is required for metal understructures.151
C. Crown Margin Placement
It is difficult to remove subgingival cement entirely around a crown placed deeper than 1 mm into the sulcus.152 Therefore, implant margins of cementable crowns should not be placed more than 1 mm subgingivally. Ideally, margins should be placed as follows: posterior implants, 0.5 mm subgingivally on the mid-buccal, mesio-buccal, and mesio-lingual, 0 mm at other locations; anterior implants, 1 mm subgingivally mid-bucally, 0.5 mm subgingivally mesio and disto-buccally, and 0 mm lingually.152
Papillae
A. Return of Papillary Height After Crown Placement on an Implant
After a transitional partial restoration is worn and a crown is initially placed, 90% of the time there is an open area under the contact point between the crown and adjacent tooth.153 Within 1 year, about 80% of papillae rebound and fill the interproximal space.153 This is due to reformation of the gingival col under the contact area.
B. Papillary Tallness Between Implants
Average height of a papilla between two implants is 3.4 mm, and >50% of papillae between implants are ≤3 mm high.154
C. Papillary Size Between an Implant and a Tooth
The mean distance from osseous bony crest to the papilla tip is 3.85 mm to 4.2 mm.155,156
D. Interproximal Papillary Recession After Implant Surgery
When thick and thin periodontal phenotypes are compared with respect to alterations of papillary and facial tissue height after single-tooth implant placement that included flap surgery, the thin phenotype demonstrates shorter papillae by approximately 0.7 mm.157 Facial tissue height is also about 0.4 mm less than tissues associated with a thick phenotype.157
Angled Abutments
Fifteen-degree and 25-degree angulated abutments can be used to correct occlusal relationships 1.5 mm and 2.5 mm, respectively.158
Crown-to-Implant Ratio
Unsplinted dental implants with a crown/root ratio of 2:1 (Figure 14) can successfully be restored, despite increased stress on the prosthesis.159
Cantilevered Pontic Off Two Implants
The success rate of prostheses with one cantilevered pontic off two implants after 10 years is 88.9%, and the success rate of implant-supported prostheses after 10 years is 86.7%.160 The size of a cantilevered pontic off two implants should be approximately 8 mm.160
Oral Hygiene
Oral hygiene is essential to maintaining periodontal and peri-implant health. Different hygiene devices penetrate to diverse depths subgingivally to reduce biofilms:
1. Toothbrush penetration under the gingiva is approximately 0.9 mm.161 Sonicare (Philips, philips.com) removes plaque subgingivally 1 mm to 3 mm.162,163
2. Oral rinses enter the sulcus <2 mm depth.164
3. Interproximally, flossing reaches subgingivally about 3 mm.165
4. Standard irrigation tips project fluid roughly 44% of depth in 4 mm to 7 mm probing depths.166
Open Contact Between Teeth and Dental Implants
After an implant restoration is inserted next to a natural tooth, an interproximal gap develops 34% to 66% of the time.167-169 This event often occurs on the mesial aspect of an implant restoration due to mesial migration of teeth, and this happens as early as 3 months after prosthetic rehabilitation.
Peri-implantitis
A systematic review indicated that 18.8% of patients (9.6% of the implants) develop peri-implantitis.170 However, this number varies in the literature, because it depends on the quantity of bone loss used to define peri-implantitis.
Implant Failure Rates
About 2% to 3% of implants are lost prior to prosthetic loading, and another 2% to 3% that supported fixed partial dentures failed within 5 years.171 A systematic review retrospectively evaluated 10 long-term studies (>15 years), and it was noted that implant survival rates among studies ranged from 70% to 100%. Nevertheless, eight of the 10 studies indicated implant survival rates were >90%.172
Conclusion
The objective of this article was to enumerate and share clinical numbers needed to treat dental implant patients. It presented digits that may be helpful during surgical and postsurgical therapy. Clinicians should bear in mind that many of the presented integers reflect mean data and the range of results may vary when managing different patients. In conclusion, when applying numbers addressed in this primer, the following axioms should be observed: always adhere to sound biologic principles, keep the therapeutic plan as simple as possible, be prepared to improvise, maintain a standard of excellence, and, finally, treat patients the way you would like to be treated.
About the Authors
Gary Greenstein, DDS, MS
Clinical Professor, Department of Periodontics, College of Dental Medicine, Columbia University; Private Practice, Surgical Implantology and Periodontics, Freehold, New Jersey
John Cavallaro, DDS
Clinical Professor, Department of Prosthodontics, College of Dental Medicine, Columbia University; Private Practice, Surgical Implantology and Prosthodontics, Brooklyn, New York
Dennis Tarnow, DDS
Clinical Professor, Department of Periodontics, Director of Implant Education, College of Dental Medicine, Columbia University; Private Practice, Surgical Implantology and Periodontics, New York, New York
References
1. Greenstein G. Diagnostic and therapeutic implications of increased probing depths: current interpretations. Compend Contin Educ Dent. 2005;26(6):381-390.
2. Dhir S, Mahesh L, Kurtzman GM, Vandana KL. Peri-implant and periodontal tissues: a review of differences and similarities. Compend Contin Educ Dent. 2013;34(7):e69-e75.
3. Berglundh T, Lindhe J, Ericsson I, et al. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2(2):81-90.
4. Karayiannis A, Lang NP, Joss A, Nyman S. Bleeding on probing as it relates to probing pressure and gingival health in patients with a reduced but healthy periodontium. A clinical study. J Clin Periodontol. 1992;19(7):471-475.
5. McGuire MK. Prognosis versus actual outcome: a long-term survey of 100 treated periodontal patients under maintenance care. J Periodontol. 1991;62(1):51-58.
6. Chace R Sr, Low SB. Survival characteristics of periodontally involved teeth: a 40-year study. J Periodontol. 1993;64(8):701-705.
7. Checchi L, Montevecchi M, Gatto MR, Trombelli L. Retrospective study of tooth loss in 92 treated periodontal patients. J Clin Periodontol. 2002;29(7):651-656.
8. Misch CE, Perel ML, Wang HL, et al. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008;17(1):5-15.
9. Froum SJ, Froum SH, Rosen PS. Successful management of peri-implantitis with a regenerative approach: a consecutive series of 51 treated implants with 3- to 7.5-year follow-up. Int J Periodontics Restorative Dent. 2012;32(1):11-20.
10. Wheeler RC. A Textbook of Dental and Physiology. 4th ed. Philadelphia, PA: WB Saunders; 1968:228-276.
11. Ettinger RL, Qian F. Postprocedural problems in an overdenture population: a longitudinal study. J Endod. 2004;30(5):310-314.
12. Bergenholtz G, Nyman S. Endodontic complications following periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol. 1984;55(2):63-68.
13. Wang N, Knight K, Dao T, Friedman S. Treatment outcome in endodontics-the Toronto Study. Phases I and II: apical surgery. J Endod. 2004;30(11):751-761.
14. Peterson J, Gutmann JL. The outcome of endodontic resurgery: a systematic review. Int Endod J. 2001;34(3):169-175.
15. Saunders WP. A prospective clinical study of periradicular surgery using mineral trioxide aggregate as a root-end filling. J Endod. 2008;34(6):660-665.
16. Tjan AH, Miller GD, The JG. Some esthetic factors in a smile. J Prosthet Dent. 1984;51(1):24-28.
17. Hochman MN, Chu SJ, Tarnow DP. Maxillary anterior papilla display during smiling: a clinical study of the interdental smile line. Int J Periodontics Restorative Dent. 2012;32(4):375-383.
18. Sardana V, Balappanavar AY, Deshpande S, et al. Evaluation of marginal alveolar bone height for early detection of periodontal disease in pediatric population: clinical and radiographic study. J Contemp Dent Pract. 2014;1;15(1):37-45.
19. Becker W, Ochsenbein C, Tibbetts L, Becker BE. Alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J Clin Periodontol. 1997;24(10):727-731.
20. Spear F. The esthetic management of multiple missing teeth. Inside Dentistry. 2007;3(1):72-76.
21. Chu SJ, Tarnow DP, Tan JH, Stappert CF. Papilla proportions in the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2009;29(4):385-393.
22. Chu SJ, Tan JH, Stappert CF, Tarnow DP. Gingival zenith positions and levels of the maxillary anterior dentition. J Esthet Restor Dent. 2009;21(2):113-120.
23. Sterrett JD, Oliver T, Robinson F, Fortson W. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J Clin Periodontol. 1999;26(3):153-157.
24. Narcisi EM, DiPerna JA. Multidisciplinary full-mouth restoration with porcelain veneers and laboratory-fabricated resin inlays. Pract Periodontics Aesthet Dent. 1999;11(6):721-730.
25. Chu SJ. Range and mean distribution frequency of individual tooth width of the maxillary anterior dentition. Pract Proced Aesthet Dent. 2007;19(4):209-215.
26. Stappert CF, Tarnow DP, Tan JH, Chu SJ. Proximal contact areas of the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2010;30(5):471-477.
27. Chu SJ, Okubo S. Range and mean discordance of individual tooth width of the mandibular anterior dentition. Pract Proced Aesthet Dent. 2008;20(5):313-320.
28. Wheeler RC. A Textbook of Dental and Physiology. 4th ed. Philadelphia, PA: WB Saunders; 1968:427-428.
29. Medline Plus. Platelet disorders. https://medlineplus.gov/plateletdisorders.html. Accessed May 24, 2018.
30. Medline Plus. Blood thinners. https://medlineplus.gov/bloodthinners.html. Accessed May 24, 2018.
31. van Slooten T. Xarelto vs Eliquis vs Pradaxa vs Savaysa - Which should you choose? http://www.livingwithatrialfibrillation.com/1369/choosing-noacs/. Accessed May 25, 2018.
32. Gibson N, Ferguson JW. Steroid cover for dental patients on long-term steroid medication: proposed clinical guidelines based upon a critical review of the literature. Br Dent J. 2004;197(11):681-685.
33. Delcanho R, Moncada E. Persistent pain after dental implant placement: a case of implant-related nerve injury. J Am Dent Assoc. 2014;145(12):1268-1271.
34. Veksler AE, Kayrouz GA, Newman MG. Reduction of salivary bacteria by pre-procedural rinses with chlorhexidine 0.12%. J Periodontol. 1991;62(11):649-651.
35. Fine DH, Furgang D, Korik I, et al. Reduction of viable bacteria in dental aerosols by preprocedural rinsing with an antiseptic mouthrinse. Am J Dent. 1993;6(5):219-221.
36. Akesson L, Håkansson J, Rohlin M. Comparison of panoramic and intraoral radiography and pocket probing for the measurement of the marginal bone level. J Clin Periodontol. 1992;19(5):326-332.
37. Goodson JM, Haffajee AD, Socransky SS. The relationship between attachment level loss and alveolar bone loss. J Clin Periodontol. 1984;11(5):348-359.
38. Hausmann E. A contemporary perspective on techniques for the clinical assessment of alveolar bone. J Periodontol. 1990;61(3):149-156.
39. Schulze RK, d'Hoedt B. Mathematical analysis of projection errors in "paralleling technique" with respect to implant geometry. Clin Oral Implants Res. 2001;12(4):364-371.
40. Sewerin IP. Estimation of angulation of Brånemark titanium fixtures from radiographic thread images. Clin Oral Implants Res. 1991;2(1):20-23.
41. Begoña Ormaechea M, Millstein P, Hirayama H. Tube angulation effect on radiographic analysis of the implant-abutment interface. Int J Oral Maxillofac Implants. 1999;14(1):77-85.
42. Sonick M, Abrahams J, Faiella RA. A comparison of the accuracy of periapical, panoramic, and computerized tomographic radiographs in locating the mandibular canal. Int J Oral Maxillofac Implants. 1994;9(4):455-460.
43. Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of space requirements to construct dental implant prostheses: horizontal and vertical dimensions. J Am Dent Assoc. In press.
44. Kendrick S, Wong D. Vertical and horizontal dimensions of implant dentistry: numbers every dentist should know. Inside Dentistry. 2009;5(7):2-5.
45. Lee JY, Kim HY, Shin SW, Bryant SR. Number of implants for mandibular implant overdentures: a systematic review. J Adv Prosthodont.2012;4(4):204-209.
46. Mahoorkar S, Bhat S, Kant R. Single implant supported mandibular overdenture: a literature review. J Indian Prosthodont Soc. 2016;16(1):75-82.
47. Anandh B, Lokesh B, Ebenezer V, et al. All on four - the basics. Biomed Pharmacol J. 2015;8:609-612.
48. Laurito D, Lamazza L, Spink MJ, De Biase A. Tissue-supported dental implant prosthesis (overdenture): the search for the ideal protocol. A literature review. Ann Stomatol (Roma). 2012;3(1):2-10.
49. Kosinski TF. Overdenture design to maximize stability and function. Dent Today. 2017;36(2):108-112.
50. Misch CE. Implant design considerations for the posterior regions of the mouth. Implant Dent. 1999;8(4):376-386.
51.Lemos CA, Ferro-Alves ML, Okamoto R, et al. Short dental implants versus standard dental implants placed in the posterior jaws: a systematic review and meta-analysis. J Dent. 2016;47:8-17.
52. van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000;11(3):256-265.
53. Misch CE, Resnick RR, Misch-Dietsh F. Maxillary sinus anatomy, pathology and graft surgery. In: Misch CE, ed. Contemporary Implant Dentistry. St. Louis, Missouri: Mosby; 2008:910.
54. Uchida Y, Goto M, Katsuki T, Akiyoshi T. A cadaveric study of maxillary sinus size as an aid in bone grafting of the maxillary sinus floor. J Oral Maxillofac Surg. 1998;56(10):1158-1163.
55. Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants. 2008;23(1):48-56.
56. Elian N, Wallace S, Cho SC, et al. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005;20(5):784-787.
57. Malamed SF. Handbook of Local Anesthesia. St. Louis, MO: Mosby; 1986:183-193.
58. Mbajiorgu EF. A study of the position of the mandibular foramen in adult black Zimbabwean mandibles. Cent Afr J Med. 2000;46(7):184-190.
59. Nicholson ML. A study of the position of the mandibular foramen in adult human mandible. Anat Rec. 1985;212(1):110-112.
60. Ikeda K, Ho KC, Nowicki BH, Haughton VM. Multiplanar MR and anatomic study of the mandibular canal. AJNR Am J Neuroradiol. 1996;17(3):579-584.
61. Uchida Y, Noguchi N, Goto M, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67(4):744-750.
62. Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006;77(12):1933-1943.
63. Dario LJ. Implant placement above a bifurcated mandibular canal: a case report. Implant Dent. 2002;11(3):258-261.
64. Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: changes with age. Acta Anat (Basel). 1986;126(1):21-28.
65. Fishel D, Buchner A, Hershkowith A, Kaffe I. Roentgenologic study of the mental foramen. Oral Surg Oral Med Oral Pathol. 1976;41(5):682-686.
66. Mohamed A, Nataraj K, Mathew VB, et al. Location of mental foramen using digital panoramic radiography. J Forensic Dent Sci. 2016;8(2):79-82.
67. Agthong S, Huanmanop T, Chentanez V. Anatomical variations of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg. 2005;63(6):800-804.
68. Butura CC, Galindo DF, Cottam J, et al. Hourglass mandibular anatomic variant incidence and treatment considerations for all-on-four implant therapy: report of 10 cases. J Oral Maxillofac Surg. 2011;69(8):2135-2143.
69. Quirynen M, Mraiwa N, van Steenberghe D, Jacobs R. Morphology and dimensions of the mandibular jaw bone in the interforaminal region in patients requiring implants in the distal areas. Clin Oral Implants Res. 2003;14(3):280-285.
70. Parnia F, Moslehifard E, Hafezeqoran A, et al. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17(3):e420-e425.
71. Yin SK, Yi HL, Lu WY, et al. Anatomic and spiral computed tomographic study of the genial tubercles for genioglossus advancement. Otolaryngol Head Neck Surg. 2007;136(4):632-637.
72. Lee SY, Choi DS, Jang I, et al. The genial tubercle: a prospective novel landmark for the diagnosis of mandibular asymmetry. Korean J Orthod. 2017;47(1):50-58.
73. Mueller HP. Anatomy and physiology. In: Periodontology: The Essentials. Stuttgart, Germany: Thieme Medical Publishers; 2004:5.
74. Goaslind GD, Robertson PB, Mahan CJ, et al. Thickness of facial gingiva. J Periodontol. 1977;48(12):768-771.
75. Studer SP, Allen EP, Rees TC, Kouba A. The thickness of masticatory mucosa in the human hard palate and tuberosity as potential donor sites for ridge augmentation procedures. J Periodontol. 1997;68(2):145-151.
76. Behnia H, Kheradvar A, Shahrokhi M. An anatomic study of the lingual nerve in the third molar region. J Oral Maxillofac Surg. 2000;58(6):649-651.
77. Sujatha N, Manjunath KY, Balasubramanyam V. Variations of the location of the greater palatine foramina in dry human skulls. Indian J Dent Res. 2005;16(3):99-102.
78. Bennet CR. Monheim's Local Anesthesia and Pain Control in Dental Practice. St. Louis, MO: Mosby; 1974:92.
79. Mogensen C, Tos M. Quantitative histology of the maxillary sinus. Rhinology. 1977;15(3):129-140.
80. Hofschneider U, Tepper G, Gahleitner A, Ulm C. Assessment of the blood supply to the mental region for reduction of bleeding complications during implant surgery in the interforaminal region. Int J Oral Maxillofac Implants. 1999;14(3):379-383.
81. Hassell TM. Tissues and cells of the periodontium. Periodontol 2000. 1993;3:9-38.
82. Pommer B, Ulm C, Lorenzoni M, et al. Prevalence, location and morphology of maxillary sinus septa: systematic review and meta-analysis. J Clin Periodontol. 2012;39(8):769-773.
83. Buskin R, Castellon P, Hochstedler JL. Orthodontic extrusion and orthodontic extraction in preprosthetic treatment using implant therapy. Pract Periodontics Aesthet Dent. 2000;12:213- 219.
84. Bennet CR. Local anesthetics and anesthetic solutions. In: Monheim's Local Anesthesia and Pain Control in Dental Practice. 5th ed. St. Louis, MO: Mosby Co; 1974:123-149.
85. Meechan JG. How to overcome failed local anesthesia. Brit Dent J. 1999;186(1)1815-1820.
86. Reiser GM, Bruno JF, Mahan PE, Larkin LH. The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 1996;16(2):130-137.
87. Bevelander G. Outline of Histology. St. Louis, MO: Mosby Co; 1967:10-34.
88. Cavallaro J, Greenstein B, Greenstein G. Extracting teeth in preparation for dental implants. Dentistry Today. 2014;33(10):92-100.
89. Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extraction alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(Suppl 5):1-21.
90. Lee CT, Chiu TS, Chuang SK, et al. J. Alterations of the bone dimension following immediate implant placement into extraction socket: systematic review and meta-analysis. J Clin Periodontol. 2014;41(9):914-926.
91. Younis MHA, Hantash ROA. Dry socket: frequency, clinical picture, and risk factors in a Palestinian dental teaching center. Open Dent J. 2011;5:7-12.
92. Bowe DC, Rogers S, Stassen LF. The management of dry socket/alveolar osteitis. J Ir Dent Assoc. 2011;57(6):305-310.
93. Almazrooa SA, Noonan V, Woo SB. Resorbable collagen membranes: histopathologic features. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(2):236-240.
94. Tal H, Kozlovsky A, Artzi Z, et al. Cross-linked and non-cross-linked collagen barrier membranes disintegrate following surgical exposure to the oral environment: a histological study in the cat. Clin Oral Implants Res. 2008;19(8):760-766.
95. Hassan HK. Dental suturing materials and techniques. Glob J Oto. 2017;12(2):555833.
96.Greenstein G, Greenstein B, Cavallaro JS Jr, Carpentieri C. Alveolar bone and implant therapy decisions in dentistry. Decisions in Dentistry. 2018;4(5):26-32.
97. Misch CE. Bone density: a key determinant for treatment planning. In: Misch CE, ed. Contemporary Implant Dentistry. St. Louis, MO: Mosby; 2008:135.
98. Cochran DL, Hermann JS, Schenk RK, et al. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontal. 1997;68(2):186-198.
99. Linkevicius T, Puisys A, Steigmann M, et al. Influence of vertical soft tissue thickness on crestal bone changes around implants with platform switching: a comparative clinical study. Clin Implant Dent Relat Res. 2015;17(6):1228-1236.
100. Garnero P, Szulic DA. Bone remodeling: cellular activities in bone. In: Orwoll ES, Bilezikian JP, Vanderschueren D, eds. Osteoporosis in Men: The Effects of Gender on Skeletal Health. London, UK: Elsevier; 2010:25-40.
101. Deguchi T, Takano-Yamamoto T, Yabuuchi T, et al. Histomorphometric evaluation of alveolar bone turnover between the maxilla and the mandible during experimental tooth movement in dogs. Am J Orthod Dentofacial Orthop. 2008;133(6):889-897.
102. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2uncovering. Ann Periodontol. 2000;5(1):119-128.
103. Belser UC, Bernard JP, Buser D. Implants in the esthetic zone. In: Lindhe J, Lang NP, Karring T, eds. Clinical Periodontology and Implant Dentistry. Oxford, UK: Blackwell Munksgaard; 2008:1146-1174.
104. Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32(3):261-267.
105. Vacek JS, Gher ME, Assad DA, et al. The dimensions of the human dentogingival junction. Int J Periodontics Restorative Dent. 1994;14(2):154-165.
106. Epperla N, Mazza JJ, Yale SH. A review of clinical signs related to ecchymosis. WMJ. 2015;14(2);61-65.
107. Baab DA, Ammons WF Jr, Selipsky H. Blood loss during periodontal flap surgery. J Periodontol. 1977:48(11):693-698.
108. Gladfelter IA Jr. A review of blood transfusion. Gen Dent.1988;36(1):37-39.
109. Greenstein G, Cavallaro J. Implant insertion torque: its role in achieving primary stability of restorable dental implants. Compend Contin Educ Dent. 2017;38(2):88-95.
110. Al-Nawas B, Wagner W, Grötz KA. Insertion torque and resonance frequency analysis of dental implant systems in an animal model with loaded implants. Int J Oral Maxillofac Implants. 2006;21(5):726-732.
111. Atieh MA, Ibrahim HM, Atieh AH. Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis. J Periodontol. 2010;81(10):1350-1366.
112. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(suppl):43-61.
113. Esposito M, Ekestubbe A, Gröndahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993;4(3):151-157.
114. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
115. Vela X, Méndez V, Rodríguez X, et al. Crestal bone changes on platform-switched implants and adjacent teeth when the tooth-implant distance is less than 1.5 mm. Int J Periodontics Restorative Dent. 2012;32(2):149-155.
116. Shenoy VK. Single tooth implants. Pretreatment considerations and pretreatment evaluation. J Interdiscip. 2012;2(3):149-157.
117. Luthra KK. Implant success!!!…..simplified. J Indian Soc Periodontol. 2009;13(1):27-29.
118. Cavallaro J, Greenstein G. Immediate dental implant placement: a review and technique paper, part 2. Dent Today. 2014;33(2):94-98.
119. Saadoun AP, LeGall M, Touati B. Selection and ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthet Dent. 1999;11(9):1063-1072.
120. Misch CE. Root form surgery in the edentulous mandible: stage I implant insertion. In: Misch CE, ed. Contemporary Implant Dentistry. St Louis, MO: Mosby; 1999:347-370.
121. Misch CE, Bidez MW. Occlusal considerations for implant supported prosthesis: implant protective occlusion. In: Misch CE, ed. Dental Implant Prosthetics. St. Louis, MO: Mosby; 2005:472-507.
122. Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24(suppl):186-217.
123. Tarnow DP, Chu SJ. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restorative Dent. 2011;31(5):515-521.
124. Greenstein G. Therapeutic efficacy of cold therapy after intraoral surgical procedures: a literature review. J Periodontol. 2007;78:790-800.
125. Greenstein G, Greenstein B. Clinical management of acute orofacial infections. Compend Contin Educ Dent. 2015;36(2):96-103.
126. Lardner A. The effects of extracellular pH on immune function. J Leukoc Biol. 2001;69(4):522-530.
127. Esposito M, Grusovin MG, Worthington HV. Interventions for replacing missing teeth: antibiotics at dental implant placement to prevent complications. Cochrane Database Syst Rev. 2013;(7):CD004152.
128. Esposito M, Coulthard P, Oliver R, et al. Antibiotics to prevent complications following dental implant treatment. Cochrane Database Syst Rev. 2003;(3):CD004152.
129. Engler WO, Ramfjord SP, Hiniker JJ. Healing following simple gingivectomy. A tritiated thymidine radioautographic study. I. Epithelialization. J Periodontol. 1966;37(4):298-308.
130. Ramfjord SP, Engler WO, Hiniker JJ. A radioautographic study of healing following simple gingivectomy. II. The connective tissue. J Periodontol. 1966;37(3):179-189.
131. Hiatt WH, Stallard RE, Butler ED, Badgett B. Repair following mucoperiosteal flap surgery with full gingival retention. J Periodontol. 1968;39(1):11-16.
132. Amler MH. Age factor in human alveolar bone repair. J Oral Implantol. 1993;19(2):138-142.
133. Misch CE, Misch-Dietsh F. Keys to bone grafting and bone graft materials. In: Misch CE, ed. Contemporary Implant Dentistry. St. Louis, MO: Mosby; 2008:862.
134. Tischler M, Misch CE. Extraction site bone grafting in general dentistry. Review of applications and principles. Dent Today. 2004;23(5):108-113.
135. Pikos MA. Block autografts for localized ridge augmentation: Part II. The posterior mandible. Implant Dent. 2000;9(1):67-75.
136. Ostman PO, Hellman M, Sennerby L. Direct implant loading in the edentulous maxilla using a bone density-adapted surgical protocol and primary implant stability criteria for inclusion. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S60-S69.
137. Cavallaro J, Greenstein B, Greenstein G. Clinical methodologies for achieving primary dental implant stability. J Am Dent Assoc. 2009;140:1366(11)-1372.
138. Todisco M, Trisi P. Histomorphometric evaluation of six dental implant surfaces after early loading in augmented human sinuses. J Oral Implantol. 2006;32(4):153-166.
139. Froum SJ, Tarnow DP, Wallace SS, et al. The use of a mineralized allograft for sinus augmentation: an interim histological case report from a prospective clinical study. Compend Contin Educ Dent. 2005;26(4):259-268.
140. Davies JE, Hosseini MM. Histodynamics of endosseous wound healing. Bone Engineering. 2000;1:1-14.
141. Cifcibasi E, Karabey V, Koyuncuoglu C, et al. Clinical evaluation of free gingival graft shrinkage in horizontal and vertical dimensions. J Istanb Univ Fac Dent. 2015;49(3):11-16.
142. Sculean A, Gruber R, Bosshardt DD. Soft tissue wound healing around teeth and dental implants. J Clin Periodontol. 2014;41(Suppl 15):S6-S22.
143. Simon B, Von Hagen S, Deasy MJ, et al. Changes in alveolar bone height and width following ridge augmentation using bone graft and membranes. J Periodontol. 2000;71(11):1774-1791.
144. Jung JH, Choi SH, Cho KS, Kim CS. Bone-added osteotome sinus floor elevation with simultaneous placement of non-submerged sand blasted with large grit and acid etched implants: a 5-year radiographic evaluation. J Periodontal Implant Sci. 2010;40(2):69-75.
145. Seddon HJ. Three types of nerve injury. Brain. 1943;66(4):237-240.
146. Banavali KA, Chitnis P, Upadhye K, Kotak B. Comparative clinical evaluation of reduction in tooth mobility using Periotest® in lower anterior teeth post phase-I therapy in patients with mild to moderate gingivitis: a randomized controlled trial. IJCRR. 2014;6(11):87-90.
147. Nagashima T, Ouchi T, Kanaya K. A study on tooth mobility following periodontal surgery. Shigaku. 1999;86(4):854-862.
148. Misch CE. Principles of cement-retained fixed implant prosthodontics: natural teeth and implant abutments. In: Misch CE, ed. Dental Implant Prosthetics. St. Louis, MO: Mosby; 2005:414-451.
149. Saleh SF, Abolfazli N, Nuroloyuni S, et al. Effect of abutment height on retention of single cement-retained, wide- and narrow-platform implant-supported restorations. J Dent Res Dent Clin Dent Prospects. 2012;6(3):98-102.
150. Dozíc, A Kleverlaan CJ, Meegdes M, et al. The influence of porcelain thickness on the final shade of ceramic restorations. J Prosthet Dent. 2003;90(6):563-570.
151. Shirakura, A, Lee H, Geminiani A, et al. The influence of veneering porcelain thickness of all-ceramic crowns on failure resistance after cyclical loading. J Prosthet Dent. 2009;10(2):119-127.
152. Schoenbaum TR. Implant prosthetics in the aesthetic zone.
http://kerncountyds.org/wp-content/uploads/2015/04/The-Art-Science-of-Aesthetic-Implant-Restorations-Handout.pdf. Accessed on June 18, 2018.
153. Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17(4):326-333.
154. Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74(12):1785-1788.
155. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
156. Grunder U. Stability of the mucosal topography around single-tooth implants and adjacent teeth: 1-year results. Int J Periodontics Restorative Dent. 2000;20(1):11-17.
157. Kan JY, Morimoto T, Rungcharassaeng K, et al. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent. 2010;30(3):237-243.
158. Cavallaro J, Greenstein G. Prosthodontic complications related to implant placement. In: Froum S. Dental Implant Complications: Etiology, Prevention, and Treatment. West Sussex, UK: Blackwell Publishing; 2010:156-171.
159. Sanz M, Naert I, Working Group 2. Biomechanics/risk management (Working Group 2). Clin Oral Implants Res. 2009;20(Supp l4):107-111.
160. Aglietta M, Siciliano VI, Zwahlen M, et al. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. Clin Oral Implants Res. 2009;20(5):441-451.
161. Waerhaug J. Effect of toothbrushing on subgingival plaque formation. J Periodontol. 1981;52(1):30-34.
162. Williams KB, Cobb CM, Taylor HJ, et al. Effect of sonic and mechanical toothbrushes on subgingival microbial flora: a comparative in vivo scanning electron microscopy study of 8 subjects. Quintessence Int. 2001;32(2):147-154.
163. Stanford CM, Srikantha R, Wu CD. Efficacy of the Sonicare toothbrush fluid dynamic action on removal of human supragingival plaque. J Clin Dent. 1997;8(1 Spec No):10-14.
164. Pitcher GR, Newman HN, Strahan JD. Access to subgingival plaque by disclosing agents using mouthrinsing and direct irrigation. J Clin Periodontol. 1980;7(4):300-308.
165. Waterpik. The Water Flosser: Your Tool For Optimal Oral Health.
https://www.waterpik.com/oral-health/pro/education/pdf/Waterpik_WaterFlosser_ContinuingEducation.pdf. Accessed June 6, 2018.
166. Eakle WS, Ford C, Boyd RL. Depth of penetration into periodontal pockets with oral irrigation. J Clin Periodontol. 1986;13(1):39-44.
167. Wat PY, Wong AT, Leung KC, Pow EH. Proximal contact loss between implant supported prostheses and adjacent natural teeth: a clinical report. J Prosthet Dent. 2011;105(1):1-4.
168. Byun SJ, Heo SM, Ahn SG, Chang M. Analysis of proximal contact loss between implant-supported fixed dental prostheses and adjacent teeth in relation to influential factors and effects: a cross-sectional study. Clin Oral Implants Res. 2015;26(6):709-714.
169. Greenstein G, Carpentieri J, Cavallaro J. Open contacts adjacent to dental implant restorations: etiology, incidence, consequences and correction. J Am Dent Assoc. 2016;147(1):28-34.
170. Atieh MA, Alsabeeha NH, Faggion CM Jr, Duncan WJ. The frequency of peri-implant diseases: a systematic review and meta-analysis. J Periodontol. 2013;84(11):1586-1598.
171. Holm-Pedersen P, Lang NP, Müller F. What are the longevities of teeth and oral implants? Clin Oral Implants Res. 2007;18(Suppl 3):15-19.
172. Levin L, Halperin-Sternfeld M. Tooth preservation or implant placement: a systematic review of long-term tooth and implant survival rates. J Am Dent Assoc. 2013;144(10):1119-1133.