Novel Direct Injection Chairside Buffering Technique for Local Anesthetic Use in Dentistry
Jason H. Goodchild, DMD; and Mark Donaldson, BSP, ACPR, PHARMD
Abstract
Background: Alkalinization or buffering of dental local anesthetics to raise the pH of these acidic solutions is a well-documented technique that results in clinical benefits such as decreased injection pain, reduced onset time, and the need for less overall volume of local anesthesia. Objective: In a previous study, two options available for buffering local anesthetics in dentistry were compared, one using the Onpharma® mixing system (Onpharma), and the other by hand mixing with 8.4% sodium bicarbonate using a "remove and replace" technique. The results of that study showed no statistically significant difference in buffering outcomes between the two methods. This follow-up in vitro study introduces and examines a less complex, direct injection, chairside hand-mixing approach using four commercially available dental local anesthetic preparations. Materials and Methods: The authors prepared multiple buffered samples of four different commercially available local anesthetic solutions. The buffered samples were mixed to 9:1, 19:1, and 18:1 ratios (local anesthetic to 8.4% sodium bicarbonate). Sample pH was recorded using a pH meter. Two samples of each local anesthetic at each ratio were prepared and sequentially pH tested. The pH was recorded via the same pH meter, which was cleaned between each test. Results: The pH change between unbuffered solutions and all buffered samples was statistically different (P < .01, CI 99%). There was no final pH difference between the 9:1 and 19:1, and 19:1 and 18:1 buffering ratios (P > .01); however, a statistical difference was seen between the final pHs of the solutions resulting from the 9:1 and 18:1 buffering ratios (P = .006, CI 99%). After correction for multiple comparisons, the difference between the 9:1 and 18:1 ratio was marginally significant (P = .048). Conclusions: Each of the buffering ratios tested can be used to alkalinize dental local anesthetic solutions. For practical purposes, a direct injection chairside of 0.1 mL of 8.4% sodium bicarbonate into any of the four local anesthetics tested is easy, simple, and safe compared to the more complex remove and replace method. Further studies are needed to evaluate if a clinically significant difference exists between the 9:1, 19:1, and 18:1 ratio solutions. Clinical Implications: The potential benefits of buffering local anesthetic solutions prior to injection, such as decreased injection pain, faster onset, and greater depth of anesthesia, may be particularly advantageous in patients who have difficulty achieving profound anesthesia for clinical dentistry, and for anesthetizing infected areas. Dentists can effectively buffer local anesthetic preparations using commercially available mixing systems or by utilizing a hand-mixing technique. Rather than using a remove and replace technique, practitioners may consider a direct injection technique, adding 0.1 mL of 8.4% sodium bicarbonate directly into any local anesthetic cartridge regardless of local anesthetic concentration.
Local anesthetic preparations are commonly packaged at an acidic pH to increase their shelf-life and stability.1 Under ordinary conditions local anesthetics exist in two forms: an inactive charged form that is soluble in water, and a clinically active, uncharged base form that is insoluble in water. The relative proportion of these two forms can be calculated using the Henderson-Hasselbalch equation and is dependent on the pH of the solution.2
The pH range of commercially available local anesthetic solutions containing a vasoconstrictor such as epinephrine is between 3 and 5, and this low pH may contribute to slow onset and injection-site pain.3 To mitigate the adverse effects of low pH local anesthetic solutions, the addition of 8.4% sodium bicarbonate to alkalinize or buffer these solutions closer to physiologic pH has been widely studied in dentistry and medicine.4-10 Alkalinization or buffering these solutions drives the stoichiometric relationship toward more uncharged local anesthetic molecules in situ. These molecules are lipid soluble, readily cross lipid membranes, and lead to faster, more profound, and more effective local anesthesia clinically. Catchlove in 1972 was the first to describe the phenomenon of faster, deeper, more profound local anesthesia as "diffusion trapping."11
Early in vitro studies demonstrated that buffering local anesthetics with 8.4% sodium bicarbonate can potentiate the nerve impulse-blocking action on peripheral nerves by these drugs.12,13 More recently, Malamed et al completed an in vivo study demonstrating a statistically significant decrease in onset time when patients received buffered lidocaine with epinephrine compared to an unbuffered solution for an inferior alveolar nerve block.14 In this study, 70% of participants achieved pulpal anesthesia in just 1:57 minutes on average after administration of buffered lidocaine, versus 8:30 minutes in patients receiving unbuffered lidocaine. These findings are consistent with Tortamano and colleagues who found mean onset of pulpal anesthesia for unbuffered lidocaine with epinephrine to be 8:42 ± 3:06 minutes.15
In 2010 the US Food and Drug Administration (FDA) approved the first chairside mixing device for buffering lidocaine known as Onset® (Onpharma, onpharma.com).16 The mixing system consists of three parts: the Onpharma® mixing pen, the Onpharma® cartridge connector, and the Onset® Sodium Bicarbonate Inj., 8.4%, USP Neutralizing Additive Solution. The desired amount of sodium bicarbonate can be selected on the mixing pen via a numbered volume dial; the manufacturer recommends the addition of 0.18 mL for a 9:1 ratio of 2% lidocaine with 1:100,000 epinephrine to 8.4% sodium bicarbonate.
In January 2015, Anutra Medical (anutramedical.com) received 510k approval from the FDA for its disposable, feedback aspiration syringe.17 The Anutra Feedback Aspiration Syringe® holds up to 5 mL of fluid and has been described as a major innovation, because most dental restorative procedures require the use of multiple local anesthetic cartridges and traditional aspiration dental syringes are limited to holding only one cartridge at a time (about 1.8 mL of fluid).18 Coupled with the new Anutra Local Anesthetic Delivery System®, which consists of the Anutra Cassette® (which allows for the mixing of lidocaine and 8.4% sodium bicarbonate in a closed, filtered environment) and the Anutra Dispenser® (that precisely buffers [mixes] at the correct ratio), the Anutra Feedback Aspiration Syringe provides local anesthesia onset within 45 seconds for infiltration and 2 to 3 minutes for blocks with buffered lidocaine. The Anutra system buffers the local anesthetic solution at a 10:1, lidocaine to 8.4% sodium bicarbonate, ratio.
Both the Onpharma and Anutra devices are only FDA approved to buffer lidocaine 2% with 1:100,000 epinephrine. This may be advantageous if the only local anesthetic used is lidocaine; however, recent US market share data shows that articaine and other local anesthetics are increasing in popularity.19,20
Having demonstrated the effectiveness of buffering seven different local anesthetics by hand mixing with 8.4% sodium bicarbonate using a chairside remove and replace technique,21 the authors' intention for this in vitro study is to compare a new, less complex, "direct injection" chairside hand-mixing approach in 2% and 4% commercially available dental local anesthetic preparations.
Materials and Methods
Four commercially available local anesthetic solutions were supplied by Dentsply Sirona Preventive (dentsplysirona.com) for pH testing (Table 1). All samples were prepared and stored in a temperature-controlled room at 23°C ± 2°C for the entire experiment. The study design involved preparation of four separate samples for each local anesthetic solution, unbuffered and buffered solutions of the four different local anesthetic preparations. The buffered solutions were alkalinized with 8.4% sodium bicarbonate at three different ratios (9:1, 19:1, and 18:1) using a hand-mixing methodology. Testing of sample pH was accomplished using an Accumet™ Research AR50 Dual Channel pH/Ion/Conductivity Meter (Fisher Scientific, fishersci.com) calibrated with reference solutions of pH 4, 7, and 10. After each pH reading the probe was wiped clean and the meter was recalibrated before switching to a different local anesthetic solution. Before each sample was tested, it was mixed for 10 seconds with a new mixing stick and then immediately tested.
pH of Unbuffered Solutions
The four local anesthetic solutions tested, including their lot numbers and pH ranges as reported by the manufacturer, are shown in Table 1. In each case, two identical samples were prepared by injecting the contents of two cartridges (3.6 mL) into a clean and dry testing vial. All samples were tested four separate times at 5-minute intervals using the same pH meter and process described above.
pH Levels of Sodium Bicarbonate
Samples of the 50 mL vial of 8.4% sodium bicarbonate (50 mL vial of 8.4% sodium bicarbonate injection, USP [Hospira Inc, pfizerinjectables.com, lot number 53-092-EV]) were created by injecting 2 mL into a clean and dry testing vial. Two sets of samples were created, and each sample was tested four separate times.
Reporting of Local Anesthetic Buffering Ratios
In all cases where a ratio is stated, it is reported as amount of local anesthetic to the amount of 8.4% sodium bicarbonate. For example, to achieve a 9:1 local anesthetic to 8.4% sodium bicarbonate ratio, the total cartridge volume of 1.8 mL consisted of 1.62 mL of local anesthetic and 0.18 mL of 8.4% sodium bicarbonate.
Buffering Local Anesthetic Solutions Using 8.4% Sodium Bicarbonate in a 9:1 Ratio
A 50 mL vial of 8.4% sodium bicarbonate (8.4% sodium bicarbonate injection, USP [Hospira Inc, lot number 53-092-EV]) was used to buffer the four local anesthetic solutions shown in Table 1.
The buffered local anesthetic samples of 9:1 ratio of local anesthesia to 8.4% sodium bicarbonate were hand mixed using the remove and replace strategy previously published (Figure 1). 21 A cartridge volume of 1.8 mL was used for all calculations when preparing the samples.22,23 In each case 0.18 mL of local anesthetic solution was removed from the cartridge using a 0.5 mL syringe with a 28-gauge, 0.5-inch needle (Kendall Monoject Insulin Syringe [Tyco Healthcare, tyco.com] lot number 027501). Using a separate unused syringe, 0.18 mL of the commercially available 8.4% sodium bicarbonate was removed from the 50 mL vial and immediately injected into the local anesthetic cartridge. The buffered local anesthetic solutions were immediately injected into a clean and dry testing vial for pH testing. Each sample consisted of 3.6 mL of buffered local anesthetic solution and was tested four separate times at 5-minute intervals.
Buffering Local Anesthetic Solutions Using 8.4% Sodium Bicarbonate in a 19:1 Ratio
A similar process was followed for the buffered local anesthetic samples of 19:1 ratio of local anesthesia to 8.4% sodium bicarbonate, again using the hand-mixed remove and replace technique (Figure 1). In each case 0.09 mL of local anesthetic solution was removed from the local anesthetic cartridge, and 0.09 mL of the commercially available 8.4% sodium bicarbonate was removed from the 50 mL vial and immediately injected into the local anesthetic cartridge using a separate unused syringe. These buffered local anesthetic solutions were also immediately injected into a clean and dry testing vial for pH testing. Each sample consisted of 3.6 mL of buffered local anesthetic solution and was tested four separate times at 5-minute intervals.
Buffering Local Anesthetic Solutions Using 8.4% Sodium Bicarbonate in a 18:1 Ratio
A new, less complex, direct injection, hand-mixing process was followed for the buffered local anesthetic samples of 18:1 ratio of local anesthesia to 8.4% sodium bicarbonate (Figure 1). In each of these samples 0.1 mL of the commercially available 8.4% sodium bicarbonate was removed from the 50 mL vial and directly injected into the local anesthetic cartridge. These buffered local anesthetic solutions were also immediately injected into a clean and dry vial for pH testing. Each sample consisted of 3.8 mL of buffered local anesthetic solution and was tested four separate times at 5-minute intervals.
Storage and Stability of Buffered Samples
Thirty-two samples were created during the experiment, each in a separate testing vial (eight unbuffered samples and 24 buffered samples using the 50 mL vial of 8.4% sodium bicarbonate). All samples were stored by placing a cover over the vials. Each sample was pH tested four times at 5-minute intervals. In all cases the samples were hand mixed with a new mixing stick for 10 seconds before pH testing at 5-minute intervals.
Reporting of Data
The pH values for each unbuffered and buffered sample are reported as means with standard deviation (Table 2). The pH values of the 8.4% sodium bicarbonate solutions are also reported as means with standard deviation.
The means of the buffered solutions were analyzed using a two-tailed t-test. A Bonferroni adjusted P value was calculated to correct for multiple comparisons. All calculations were done using Excel (Microsoft® Office 2016, Microsoft Corp, microsoft.com).
Results
The combined mean pH of the 8.4% sodium bicarbonate used to buffer the local anesthetic solutions was 7.99 ± 0.072.
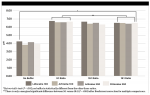
The measured pH values for the four tested local anesthetic solutions are shown in Table 2 and depicted in Figure 2. The initial pH of all of the local anesthetic solutions were within the labeled range as supplied by the manufacturer. The Xylocaine© (lidocaine) solution showed a slightly higher pH than both the Articadent© (articaine) solutions and Citanest© (prilocaine), and the pH range for all four solutions ranged from 3.99 to 4.29.
In all cases, after buffering and regardless of buffering technique, the pH of the local anesthetic solutions increased. The 9:1 buffering ratio produced the highest pH (combined mean 6.97 ± 0.06), whereas the solutions buffered at 19:1 and 18:1 ratios produced a slightly lower pH (combined mean of 6.77 ± 0.12 and 6.82 ± 0.05, respectively), as shown in Figure 3. According to the two-tail t-test, the pH of all buffered solutions significantly differed from unbuffered solutions (P < .001). No statistically significant difference was detected between the combined mean pH of the 9:1 and 19:1, and 19:1 and 18:1 ratio samples, although a slight difference (P = .006) was seen between the 9:1 and 18:1 buffering ratios. After calculating a corrected P value by the Bonferroni adjustment for multiple comparisons this marginal difference was again seen between the 9:1 and 18:1 ratios (P = .048) as shown in Table 3 and Figure 2.
Discussion
Manufacturers typically define a target pH range that local anesthetic preparations must fall within to meet good manufacturing practices in order to be sold; in this study all of the tested local anesthetic solutions were within the appropriate range (Table 1). Under normal conditions, local anesthetics exist in two forms, a clinically inactive charged form that is soluble in water, and a clinically active uncharged base form that is insoluble in water.24,25 The relative proportion of these two forms is dependent on the pH of the solution and can be calculated using the Henderson-Hasselbalch equation.2
The ability to successfully buffer the pH of seven different commercially available local anesthetic preparations at a 9:1 ratio of local anesthetic to 8.4% sodium bicarbonate utilizing a simple remove and replace chairside hand-mixing technique versus the commercially available Onpharma mixing device has been previously described.21 Based on the results of that study showing no statistically significant difference in buffering outcomes, this current follow-up in vitro study introduces a less complex, direct injection, chairside hand-mixing approach in four commercially available dental local anesthetic preparations. A technique that involves just a single step to add a small amount of 8.4% sodium bicarbonate directly into a local anesthetic cartridge versus a technique that requires two manipulations (removal of local anesthetic solution and replacement with sodium bicarbonate) may be easier and more efficient for practitioners, which could potentially decrease propagation of procedural errors. Ultimately, this may lead to more precise buffering outcomes and perhaps be considered a safer practice.
Local anesthetic solutions containing a vasoconstrictor (eg, Xylocaine [lidocaine],Articadent [articaine], and Citanest [prilocaine]) are supplied at an acidic pH (approximately 3 to 5) to prolong shelf life and improve stability of the epinephrine. The addition of sulfites (either sodium metabisulfite or potassium metabisulfite) lowers pH to prevent oxidative degradation of epinephrine; manufacturers use sodium hydroxide to adjust the final pH of the solutions as described in Table 1. After injection, and prior to onset of anesthetic action, the body's physiologic pH naturally alkalinizes the local anesthetic solution; as a result, more anesthetic molecules are converted to the uncharged lipid soluble form (even at physiologic pH, however a roughly 70:30 ratio exists for the charged form to uncharged form).14,23 The initial low pH of the drug in the cartridge therefore contributes to local anesthetic latency, because it takes time for the body to alkalinize low pH solutions and injection-site pain because of direct soft-tissue injury.3,26
Plain (epinephrine-free) solutions such as Citanest(prilocaine)and Polocaine© (mepivacaine) (Dentsply Sirona) are available at a higher pH range (closer to physiologic pH) from the manufacturer.21 This may account for their faster onset of action and reduced injection site pain.24,27-29 This may also explain why previously published studies on buffering of these solutions with 8.4% sodium bicarbonate resulted in a minimal pH change.21 It is unlikely that the buffering of plain solutions adds value in clinical situations, which is why this study was designed to buffer only four common local anesthetic formulations containing a vasoconstrictor. The 2% lidocaine with 1:50,000 epinephrine formulation was excluded from this study because of the assumption that the 1:100,000 concentration is more popular, and that the increased epinephrine concentration should be reserved for previously anesthetized areas where increased local hemostasis is required.
Frank and Lalonde reexamined the question of how much 8.4% sodium bicarbonate should be added to buffer lidocaine to better match physiologic pH levels.30 They noted that the amount of bicarbonate needed to buffer 10 mL of 1% lidocaine was between 1.1 mL and 1.8 mL, which is a buffering ratio of 9:1 to 5.5:1, lidocaine to 8.4% sodium bicarbonate. The authors stated that for practical purposes a 10:1 ratio of 1% lidocaine to 8.4% sodium bicarbonate was appropriate and that there was no risk of precipitate at this concentration.
The two commercially available buffering devices are FDA-approved only for use with 2% lidocaine containing 1:100,000 epinephrine, but as shown previously, other local anesthetic solutions also can be alkalinized. Furthermore, a 9:1 or 10:1 buffering ratio has been established for lidocaine solutions using these devices, but no such ratio has been established for 4% dental local anesthetic solutions of articaine and prilocaine. It has been suggested that for higher-concentration local anesthetic solutions a smaller amount of sulfite preservative is needed.31 This is confirmed in the product monographs and material safety data sheets of lidocaine, articaine, and prilocaine solutions.32-34 Therefore, using the same 9:1 or 10:1 ratios of local anesthetic to 8.4% sodium bicarbonate to buffer these more concentrated solutions, compared to 1% or 2% lidocaine, may overwhelm the buffering capacity of 4% solutions. By doing so, a precipitate of articaine or prilocaine could form, possibly resulting in injection site irritation, pain, and necrosis. To account for this, half the amount of bicarbonate should be used to buffer 4% compared to 2% dental local anesthetic solutions. It should be noted that no visible precipitate formed in the samples in the present study, although this was most likely the result of the quick succession of mixing and pH testing. The authors did not store or observe their samples over an extended time period.
The results of the current study demonstrated that all three buffering ratios tested (9:1, 19:1, and 18:1 local anesthetic to 8.4% sodium bicarbonate) raised the pH of the local anesthetic to approximately 7 (physiologic pH is approximately 7.35), with only the 9:1 and 18:1 ratios showing a statistically significant difference (P = .006, CI 99%). After calculating a corrected P value to account for multiple comparisons, only a marginal difference was seen between the 9:1 and 18:1 ratios (P = .48). This was most likely due to the smaller standard deviation seen with the 18:1 versus 19:1 ratio and the reduced procedural complexity of the direct injection technique compared to the remove and replace technique. This smaller standard deviation further indicates a higher level of precision and increased accuracy of the direct injection technique.
The in vitro results of this study demonstrate that the resulting pH after buffering with both chairside hand-mixing techniques was approximately 7, and while the difference between the 9:1 and 18:1 ratios was statistically significant, further in vivostudies are needed to evaluate if a clinical difference exists between the 9:1, 19:1, and 18:1 buffering ratios. When using a chairside hand-buffering technique regardless of local anesthetic concentration, a direct injection technique using 0.1 mL of 8.4% sodium bicarbonate may be easier and more precise compared to a remove and replace technique at either the 9:1 or 19:1 ratio. This simpler chairside buffering technique may also be safer for the clinician due to fewer manipulations with hypodermic needles. In vitro, adding 0.1 mL to a full dental local anesthetic cartridge is easy to accomplish and will not cause displacement of the rear stopper. Practically, the questions that must be addressed in further studies are whether a clinically significant difference exists between the buffering ratios used in this study and if alternative buffering ratios may be more appropriate for buffering 4% local anesthetic solutions.
This was a laboratory investigation, and as such, clinical implications can only be suggested as a direction of research for future clinical trials. However, the authors determined that there is no difference in pH achieved when buffering of 2% Xylocaine(lidocaine), 4% Articadent (articaine), and 4% Citanest (prilocaine) solutions containing a vasoconstrictor at a 9:1 or 19:1 ratio. A statistically significant difference is seen between the 9:1 and 18:1 ratios of local anesthetic to 8.4% sodium bicarbonate; however, it remains to be evaluated if this difference is clinically significant. Despite the statistical difference between 9:1 and 18:1, all pH readings approximated physiologic pH following the addition of sodium bicarbonate.
Conclusions and Clinical Relevance
Three hand-mixed buffering ratios were used to evaluate the pH change of 2% and 4% commercially available dental local anesthetic solutions containing epinephrine. All of the tested buffering ratios resulted in an increased pH approximating 7, and a statistically significant difference was seen only between the 9:1 and 18:1 local anesthetic to sodium bicarbonate ratio solutions; however, it is unclear if this is clinically significant. Because of decreased complexity, increased ease, and high precision, practitioners may consider utilizing a direct injection technique by adding 0.1 mL of commercially available 8.4% sodium bicarbonate to alkalinize local anesthetic cartridges, regardless of concentration. While all ratios studied-9:1, 19:1, and 18:1-can be used to bring local anesthetic solutions closer to physiologic pH immediately prior to injection, the 18:1 direct injection technique is easier, more precise, and safer due to fewer manipulations compared to the remove and replace method. Additional studies are needed to evaluate whether clinical differences exist between different buffering ratios.
Buffering of local anesthetic solutions prior to injection may provide benefits such as decreased injection pain, faster onset, and greater depth of anesthesia. These benefits may be particularly advantageous in patients who have difficulty achieving profound anesthesia for clinical dentistry, and for anesthetizing infected areas. While not all clinicians may choose to buffer local anesthetic solutions for reasons such as cost, added procedural steps, or complexity, this in vitro study demonstrates that a hand-mixing technique will raise pH similarly to existing commercialized buffering solutions. By using a simple direct injection technique, adding 0.1 mL of 8.4% sodium bicarbonate directly into the cartridge, clinicians can buffer the solution regardless of local anesthetic concentration.
Disclosure
Dentsply Sirona Preventive donated the local anesthetics solutions used in this study. The authors received no financial assistance or remuneration for the completion of this study.
Ackowlegment
The authors thank laboratory technician Vilma Torres for her assistance in testing and storing samples, and Dentsply Sirona for the donation of materials and laboratory time to complete this study. They also thank Sonia Rocha-Sanchez, MS, PhD, MBA, Professor and Research Dean, Creighton University School of Dentistry, for her help with statistical analysis.
About the Authors
Jason H. Goodchild, DMD
Director of Clinical Affairs, Premier Dental Products Co., Plymouth Meeting, Pennsylvania; Associate Clinical Professor, Department of Diagnostic Sciences, Creighton University School of Dentistry, Omaha Nebraska; Adjunct Assistant Professor, Division of Oral Diagnosis, Department of Diagnostic Sciences, Rutgers School of Dental Medicine, New Brunswick, New Jersey
Mark Donaldson, BSP, ACPR, PharmD
Associate Principal, Vizient Pharmacy Advisory Solutions, Irving, Texas; Clinical Professor, School of Pharmacy, University of Montana, Missoula, Montana; Clinical Assistant Professor, School of Dentistry, Oregon Health & Sciences University, Portland, Oregon
References
1. Christoph RA, Buchanan L, Begalla K, Schwartz S. Pain reduction in local anesthetic administration through pH buffering. Ann Emerg Med. 1988;17(2):117-120.
2. Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog. 2012;59(2):90-101.
3. Whitcomb M, Drum M, Reader A, et al. A prospective, randomized, double-blind study of the anesthetic efficacy of sodium bicarbonate buffered 2% lidocaine with 1:100,000 epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2010;57(2):59-66.
4. Curatolo M, Petersen-Felix S, Arendt-Nielsen L, et al. Adding sodium bicarbonate to lidocaine enhances the depth of epidural blockade. Anesth Analg. 1998;86(2):341-347.
5. Al Shahwan MA. Prospective comparison between buffered 1% lidocaine-epinephrine and skin cooling in reducing the pain of local anesthetic infiltration. Dermatol Surg. 2012;38(10):1654-1659.
6. Burns CA, Ferris G, Feng C, et al. Decreasing the pain of local anesthesia: a prospective, double-blind comparison of buffered, premixed 1% lidocaine with epinephrine versus 1% lidocaine freshly mixed with epinephrine. J Am Acad Dermatol. 2006;54(1):128-131.
7. McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesth Analg. 1987;66(6):572-574.
8. Stewart JH, Chinn SE, Cole GW, Klein JA. Neutralized lidocaine with epinephrine for local anesthesia-II. J Dermatol Surg Oncol. 1990;16(9):842-845.
9. Capogna G, Celleno D, Laudano D, Giunta F. Alkalinization of local anesthetics. Which block, which local anesthetic? Reg Anesth. 1995;20(5):369-377.
10. Cepeda MS, Tzortzopoulou A, Thackrey M, et al. Adjusting the pH of lidocaine for reducing pain on injection. Cochrane Database Syst Rev. 2010;(12):CD006581.
11. Catchlove RF. The influence of CO2 and pH on local anesthetic action. J Pharmacol Exp Ther. 1972;181(2):298-309.
12. Gissen AJ, Covino BG, Gregus J. Differential sensitivity of fast and slow fibers in mammalian nerve. IV. Effect of carbonation of local anesthetics. Reg Anesth. 1985;10(2):68-75.
13. Wong K, Stricharzt GR, Raymond SA. On the mechanisms of potentiation of local anesthetics by bicarbonate buffer: drug structure-activity studies on isolated peripheral nerve. Anesth Analg. 1993;76(1):131-143.
14. Malamed SF, Tavana S, Falkel M. Faster onset and more comfortable injection with alkalinized 2% lidocaine with epinephrine 1:100,000. Compend Contin Educ Dent. 2013;34 spec no 1:10-20.
15. Tortamano IP, Siviero SL, Lee S, et al. Onset and duration period of pulpal anesthesia or articaine and lidocaine in inferior alveolar nerve block. Braz Dent J. 2013;24(4):371-374.
16. Onpharma Sodium Bicarbonate Inj., 8.4% USP Neutralizing Additive Solution [package insert]. Carson City, NV: Onpharma Co; 2017. https://www.onpharma.com/pdf/Onpharma_Sodium%20Bicarbonate_Additive_Solution_Package_Insert.pdf. Accessed June 20, 2019.
17. US Dept of Health and Human Services. 510(k) approval letter. Silver Spring, MD: Food and Drug Administration; January 8, 2015. https://www.accessdata.fda.gov/cdrh_docs/pdf14/K143757.pdf. Accessed June 20, 2019.
18. Anutra Medical Receives 510k Approval and Launches New Dental Syringe to Market. Triangle Park, NC: Anutra Medical; January 8, 2015. https://anutramedical.com/wp-content/uploads/2015/04/Anutra-Medical-Receives-510k-Approval-and-Launches-New-Dental-Product.pdf. Accessed June 20, 2019.
19. Strategic Data Marketing. Anesthetics Injectable Carpules. https://sdmnorthcoast.com. Accessed June 26, 2019.
20. Donaldson M, Goodchild JH. Lidocaine turns 70: the evolution of dental local anesthesia. Gen Dent. 2018;66(3):6-9.
21. Goodchild JH, Donaldson M. Comparing the pH change of local anesthetic solutions using two chairside buffering techniques. Compend Contin Educ Dent. 2016;37(5):e6-e12.
22. Robertson D, Nusstein J, Reader A, et al. The anesthetic efficacy of articaine in buccal infiltration of mandibular posterior teeth. J Am Dent Assoc. 2007;138(8):1104-1112.
23. Malamed SF. Clinical action of specific agents. In: Handbook of Local Anesthesia. St. Louis, MO: Elsevier Mosby; 2014:56.
24. Malamed SF. Buffering local anesthetics in dentistry. The Pulse. 2011;44(1):7-9.
25. Phero JA, Nelson B, Davis B, et al. Buffered versus non-buffered lidocaine with epinephrine for mandibular nerve block: clinical outcomes. J Oral Maxillofac Surg. 2017;75(4):688-693.
26. Wahl MJ, Schmitt MM, Overton DA. Injection pain of prilocaine plain, mepivacaine plain, articaine with epinephrine, and lidocaine with epinephrine. Gen Dent. 2006;54(3):168-171.
27. Kramp LF, Eleazer PD, Scheetz JP. Evaluation of prilocaine for the reduction of pain associated with transmucosal; anesthetic administration. Anesth Prog. 1999;46(2):52-55.
28. Wahl MJ, Schmitt MM, Overton DA. Injection pain of prilocaine plain, mepivacaine plain, articaine with epinephrine, and lidocaine with epinephrine. Gen Dent. 2005;54(3):168-171.
29. Wahl MJ, Schmitt MM, Overton DA, Gordon MK. Injection pain of bupivacaine with epinephrine vs. prilocaine plain. J Am Dent Assoc. 2002;133(12):1652-1656.
30. Frank SG, Lalonde DH. How acidic is the lidocaine we are injecting, and how much bicarbonate should we add? Can J Plastic Surg. 2012;20(2):71-73.
31. Grubstein B, Milano E. Stabilization of epinephrine in a local anesthetic injectable solution using reduced levels of sodium metabisulfite and edta. Drug Development and Industrial Pharmacy. 1992;18(14):1549-1566.
32. Lidocaine HCl [package insert]. Cambridge, Ontario, Canada: Cook-Waite; 2013. https://www.septodontusa.com/sites/default/files/2017-11/CW-Lidocaine-PI_0.pdf. Accessed June 20, 2019.
33. Septanest SP and Septanest N [product monograph]. Paris, France: Septodont; June 26, 2007. https://pdf.hres.ca/dpd_pm/00004093.PDF. Accessed June 20, 2019.
34. Citanest Forte Dental [material safety data sheet]. Dentsply. November 2014. https://pdf.hres.ca/dpd_pm/00004093.PDF. Accessed June 20, 2019.