Efficacy of Ketamine in Pediatric Sedation Dentistry: A Systematic Review
Samuel Oh, DDS; and Karl Kingsley, PhD
Abstract
Background: Ketamine has been used as a safe and effective sedative to treat adults and children exhibiting high levels of anxiety or fear during dental treatment. Pediatric dentistry often involves patients with high levels of anxiety and fear and possibly few positive dental experiences. Patient management can involve behavioral approaches, as well as the use of sedation or general anesthesia with a variety of agents, including midazolam, diazepam, hydroxyzine, meperidine, and ketamine. The aim of this study was to investigate the clinical efficacy of ketamine use in pediatric sedation dentistry through systematic review and analysis. Methods: A systematic review of publications between 1990 and 2015 was conducted using PubMed and MEDLINE databases maintained by the US National Library of Medicine and the National Institutes of Health. The keywords used were (ketamine) AND (dental OR dentistry) AND (sedation). The abstract and title of all potential publications were then screened for clinical trials and to remove non-English articles, non-human or animal trials, and other non-dental or non-relevant studies. Results: A total of 1,657 citations were initially identified, reviewed, and screened, eventually resulting in inclusion of 25 clinical trials in this systematic review. Nineteen studies evaluated ketamine effects in pediatric dental sedation using oral (non-invasive) administration, three involved subcutaneous or intramuscular injection, and three were completed intravenously. Evidence analysis of these trials revealed the majority (n = 22/25) provided strong, positive evidence for the use of ketamine (alone or in combination) to reduce dental anxiety and behavioral non-compliance with the remainder suggesting equivocal results. Additional endpoints evaluated in some studies involved dosage, as well as time to achieve sedation effect. Conclusion: The use of ketamine (alone or in combination) can provide safe, effective, and timely sedation in pediatric patients regardless of the route of administration.
Ketamine has been safely and effectively used as a sedative to treat adults and children exhibiting high levels of anxiety or fear during dental treatment.1,2 Many sedatives, including ketamine, are commonly utilized after unsuccessful attempts at behavioral modification and have been demonstrated to be safe, effective, and inexpensive alternatives for sedation to reduce patient fear and anxiety and improve overall patient satisfaction.3,4 Some studies also have reviewed adverse outcomes associated with pediatric dental sedation involving ketamine to demonstrate comparable outcomes and provide more comprehensive analyses and comparisons of effectiveness.5,6
Pediatric dentistry can often involve patients with high levels of anxiety and fear and who have had relatively few positive dental experiences.7,8 Moreover, other developmental, psychological, and behavioral issues may further contribute to uncooperative patients in the pediatric dental clinic or practice.9,10 In some cases, cognitive impairments and multiple comorbidities may represent a separate category of pediatric patients who have more clearly defined special needs that necessitate dental sedation.11,12
Patient management can involve behavioral approaches and the use of different levels of sedation or general anesthesia utilizing a variety of agents, including midazolam, diazepam, hydroxyzine, meperidine, and ketamine.1,2,10,13,14 Based on this information, the aim of this study was to investigate more specifically the evidence for clinical efficacy of ketamine use in pediatric sedation dentistry through systematic review and analysis of the literature.
Materials and Methods
Human Subjects
The protocol for this study was reviewed and deemed exempt by the University of Nevada Las Vegas Office for the Protection of Research Subjects (OPRS) and the Institutional Review Board (IRB) on March 4, 2016 [875890-1] "A Systematic Review of the Use of Ketamine in Pediatric Sedation Dentistry."
PRISMA
This systematic review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and protocol.15,16 The MEDLINE and PubMed databases were searched using Medical Subject Headings (MeSH) for controlled vocabulary indexing of published evidence related to clinical efficacy of ketamine use in pediatric sedation dentistry. The initial keywords or search terms used were "ketamine" AND "sedation" for published work between January 1, 1990, and December 31, 2015. The inclusion criteria were those related to human subjects that were pediatric patients (<18 years of age) in a dental setting. Exclusion criteria included non-human subjects (animal or in vitro studies), adult patients (>18 years of age), and non-dental clinical applications or settings.
Two-Step Review
This process was initially performed by the lead author and then separately and independently performed and confirmed by the second author. Any discrepancies and questions were marked for discussion and review, which did not influence the final articles selected. The final articles selected were agreed upon by both reviewers prior to full-text review of each study.
Results
Using the PRIMSA protocol and search guidelines, a total of 1,657 citations were found using the initial search criteria "ketamine" and "sedation" (Figure 1). These results were then screened for duplicates and then limited and narrowed by application of the inclusion and exclusion criteria terms, including "pediatric" and "dental," which narrowed the results more specifically. In brief, only 441 articles were found to contain "ketamine," "sedation," and "pediatric," and 49 articles were found with "ketamine," "sedation," "pediatric," and "dental." Removal of non-English articles and studies involving animals further limited these results to the total of 25 studies selected due to their clinical study design and inclusion of pediatric dental patients treated with sedation using ketamine.
An overview of each study17-41 was created to summarize the main qualities and characteristics of that study, including the study authors, publication year, size of patient study sample or clinical trial, type of sedative administered (ketamine alone or in combination) and dosages, and the route of administration (Table 1).
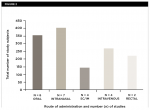
To better describe the main routes of administration, studies were then grouped and the number of subjects from each category were sorted and tallied (Figure 2). This analysis revealed that the majority of studies regarding ketamine sedation among pediatric patients involved oral administration (n = 8, subjects = 353), with several other studies involving intranasal administration (n = 7, subjects = 403), as well as other less commonly studied methods.
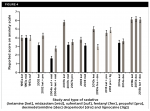
In addition, the dosages and concentrations of ketamine (either alone or in combination with other sedatives) used in each study were then analyzed and graphed (Figure 3). This analysis revealed the average concentration for all studies and subjects combined was 4.8 mg/kg, which corresponded well with the most common dosage administered (5 mg/kg). More than one-third of all studies involved ketamine sedation at 5 mg/kg, with most studies within the range of 3 mg/kg to 8 mg/kg; average = 5.4 mg/kg. The average dosages for oral (6.1 mg/kg) and nasal (4.5 mg/kg) administration were also similar.
Several key features of each study were collated and organized for further review and analysis (Table 2). Major endpoints and outcome variables were collected for each study and included: sedation (anxiety) score, percent (%) of patients with a "good" sedation, time to effect, and time range for each. (Note: "good" sedation was assessed using a standardized sedation rating score, which rates four categories relating to the sedative: sleep, movement, crying, and overall behavior.20) Comparisons between ketamine alone and in combination, along with other sedatives (alone and in combination), were then graphed (Figure 4 and Figure 5).
More specifically, studies that included the comparative evaluations for anxiety score with specific sedatives were graphed for analysis (Figure 4). These data revealed that the average anxiety score for pediatric patients under sedation with ketamine (4.45) or ketamine in combination with another sedative (4.46) such as midazolam or dexmedetomidine was comparable to other sedatives, such as midazolam, sufetanil, fentanyl, or propofol (either alone or in combination) at 3.814.
In addition, a mostly non-overlapping set of 12 studies measured the percent (%) of patients with "good" sedation, which was defined by a broad range of clinical standards and measurements (Figure 5). The compilation and analysis of these studies revealed that the combined average of patients with good sedation for all studies involving pediatric sedation with ketamine (57.8%) or ketamine-containing combination sedatives (64.11%) was 60.56%. These averages are similar and comparable to the average percent of patients with "good" sedation using alternative sedatives, such as promethazine, diazepam, sufentanil, or dexmedetomidine either alone (59.55%) or in combination (73.3%), which was 63.31%.
Discussion
This systematic review was conducted with the purpose of finding evidence for clinical efficacy of ketamine use in pediatric sedation dentistry through systematic review and analysis. Ketamine has been classified as an N-methyl-D-aspartate receptor (DMDAR) agonist, which has been favored for use among specific patients due to fewer and lowered effects on respiration and circulation compared with other anesthetics.42,43 These effects may have been useful considerations for dentists and other clinicians searching for pharmacologic treatments for pediatric patients with special needs.1,7,10 Oral route of administration is most popular, as pediatric patients can tolerate the intake of the sedative. However, oral route is less predictable than the intravenous or intramuscular route.
Ketamine may be used alone or in combination with other medication to achieve synergistic effects. The assessment of the effectiveness of ketamine alone is difficult because many of the studies used various combinations of sedatives/medications along with different routes of administration, which may affect the result of the sedation. Regardless, this systematic review provides strong evidence that the use of ketamine (alone or in combination) can provide safe, effective, and timely sedation in pediatric patients regardless of the route of administration based on the criteria and outcome of the studies using PRISMA protocol and guidelines.
Because behavioral problems may also be associated with specific types of intellectual and cognitive disabilities, such as autism and epilepsy, which in turn may be associated with additional physiologic complications, recent studies have evaluated adverse outcomes associated with pediatric ketamine sedation to provide more specific guidance and reassurance for clinicians considering these procedures.44-46 These studies provide additional evidence that ketamine (alone or in combination) may be used without serious side effects or adverse complications, specifically among these populations, although nausea was reported in a small subset of patients. These studies provide further support for earlier work that demonstrated the administration of anesthetics, including ketamine, may facilitate the completion of technically complex dental treatments to patients with a wide variety of psychosocial, intellectual, and cognitive challenges who might otherwise not be treated.47,48
Other limitations of this review include variables that may have influenced the outcomes of the study, such as the overall weight of the pediatric patient and the relative body mass index (BMI).49,50 These studies may suggest that dosing using propofol is similar for patients who are normal or underweight, but that children who are overweight or obese with high BMI may require dissimilar dosing and can experience different sedation outcomes related to these measures.51 An additional confounding variable may be the age of each patient, which was not necessarily reported in many of these studies but has been the subject of recent debates regarding pediatric dental procedures.52
Conclusion
Although not all studies utilized the same endpoints (anxiety scale, percent of patients with "good" sedation) or similar dosages and concentrations, the analysis of these data demonstrated the evidence from randomized controlled trials provides strong rationale that pediatric sedation with ketamine or ketamine-containing combinations may be effective and comparable to other forms of pediatric sedation, although more research in this area is needed. Any dentist providing sedation for patients, including pediatric patients, must be in compliance with professional guidelines and state board of dentistry requirements for sedation.
Acknowledgments
Dr. Oh would like to thank Cody Hughes, DMD; Connie Mobley, PhD; and Brian Chrzan, DDS, PhD, for their assistance and support on this project. Dr. Kingsley would like to thank Dr. Oh for his extraordinary patience and resilience during the data collection, analysis, and writing of this manuscript.
About the Authors
Samuel Oh, DDS
Department of Advanced Education in Pediatrics, University of Nevada, Las Vegas, School of Dental Medicine, Las Vegas, Nevada
Karl Kinsgley, PhD
Department of Biomedical Sciences, University of Nevada, Las Vegas, School of Dental Medicine, Las Vegas, Nevada
References
1. Corcuera-Flores JR, Silvestre-Rangil J, Cutando-Soriano A, López-Jiménez J. Current methods of sedation in dental patients - a systematic review of the literature. Med Oral Patol Oral Cir Bucal. 2016;21(5):e579-e586.
2. Gazal G, Fareed WM, Zafar MS, Al-Samadani KH. Pain and anxiety management for pediatric dental procedures using various combinations of sedative drugs: A review. Saudi Pharm J. 2016;24(4):379-385.
3. Done V, Kotha R, Vasa AA, et al. A comparison of the effectiveness of oral midazolam-N2O versus oral ketamine-N2O in pediatric patients-an in-vivo study. J Clin Diagn Res. 2016;10(4):ZC45-ZC48.
4. Folayan MO, Faponle AF, Oziegbe EO, Adetoye AO. A prospective study on the effectiveness of ketamine and diazepam used for conscious sedation in paediatric dental patients' management. Eur J Paediatr Dent. 2014;15(2):132-136.
5. Zanaty OM, El Metainy SA. A comparative evaluation of nebulized dexmedetomidine, nebulized ketamine, and their combination as premedication for outpatient pediatric dental surgery. Anesth Analg. 2015;121(1):167-171.
6. Surendar MN, Pandey RK, Saksena AK, et al. A comparative evaluation of intranasal dexmedetomidine, midazolam and ketamine for their sedative and analgesic properties: a triple blind randomized study. J Clin Pediatr Dent. 2014;38(3):255-261.
7. Wilson S. Management of child patient behavior: quality of care, fear and anxiety, and the child patient. Pediatr Dent. 2013;35(2):170-174.
8. Wilson S. Management of child patient behavior: quality of care, fear and anxiety, and the child patient. J Endod. 2013;39(3 suppl):S73-S77.
9. Gao X, Hamzah SH, Yiu CK, et al. Dental fear and anxiety in children and adolescents: qualitative study using YouTube. J Med Internet Res. 2013;15(2):e29.
10. Delli K, Reichart PA, Bornstein MM, Livas C. Management of children with autism spectrum disorder in the dental setting: concerns, behavioural approaches and recommendations. Med Oral Patol Oral Cir Bucal. 2013;18(6):e862-e868.
11. Rutkauskas J, Seale NS, Casamassimo P, Rutkauskas JS. Preparedness of entering pediatric dentistry residents: advanced pediatric program directors' and first-year residents' perspectives. J Dent Educ. 2015;79(11):1265-1271.
12. Wang YC, Lin IH, Huang CH, Fan SZ. Dental anesthesia for patients with special needs. Acta Anaesthesiol Taiwan. 2012;50(3):122-125.
13. Fakhruddin KS, Gorduysus MO, El Batawi H. Effectiveness of behavioral modification techniques with visual distraction using intrasulcular local anesthesia in hearing disabled children during pulp therapy. Eur J Dent. 2016;10(4):551-555.
14. Antunes DE, Viana KA, Costa PS, Costa LR. Moderate sedation helps improve future behavior in pediatric dental patients - a prospective study. Braz Oral Res. 2016;30(1):e107.
15. Agnihotry A, Fedorowicz Z, Worthington HV, et al. Systematic reviews in oral health: a quality imperative. J Evid Based Med. 2016. doi:10.1111/jebm.12189. [Epub ahead of print]
16. Rader T, Mann M, Stansfield C, et al. Methods for documenting systematic review searches: a discussion of common issues. Res Synth Methods. 2014;5(2):98-115.
17. van der Bijl P, Roelofse JA, Stander IA. Rectal ketamine and midazolam for premedication in pediatric dentistry. J Oral Maxillofac Surg. 1991;49(10):1050-1054.
18. Okamoto GU, Duperon DF, Jedrychowski JR. Clinical evaluation of the effects of ketamine sedation on pediatric dental patients. J Clin Pediatr Dent. 1992;16(4):253-357.
19. Abrams R, Morrison JE, Villasenor A, et al. Safety and effectiveness of intranasal administration of sedative medications (ketamine, midazolam, or sufentanil) for urgent brief pediatric dental procedures. Anesth Prog. 1993;40(3):63-66.
20. Alfonzo-Echeverri EC, Berg JH, Wild TW, Glass NL. Oral ketamine for pediatric outpatient dental surgery sedation. Pediatr Dent. 1993;15(3):182-185.
21. Reinemer HC, Wilson CF, Webb MD. A comparison of two oral ketamine-diazepam regimens for sedating anxious pediatric dental patients. Pediatr Dent. 1996;18(4):294-300.
22. Roelofse JA, Joubert JJ, Roelofse PG. A double-blind randomized comparison of midazolam alone and midazolam combined with ketamine for sedation of pediatric dental patients. J Oral Maxillofac Surg. 1996;54(7):838-844.
23. Roelofse JA, Louw LR, Roelofse PG. A double blind randomized comparison of oral trimeprazine-methadone and ketamine-midazolam for sedation of pediatric dental patients for oral surgical procedures. Anesth Prog. 1998;45(1):3-11.
24. Campbell RL, Ross GA, Campbell JR, Mourino AP. Comparison of oral chloral hydrate with intramuscular ketamine, meperidine, and promethazine for pediatric sedation-preliminary report. Anesth Prog. 1998;45(2):46-50.
25. Sullivan DC, Wilson CF, Webb MD. A comparison of two oral ketamine-diazepam regimens for the sedation of anxious pediatric dental patients. Pediatr Dent. 2001;23(3):223-231.
26. Bui T, Redden RJ, Murphy S. A comparison study between ketamine and ketamine-promethazine combination for oral sedation in pediatric dental patients. Anesth Prog. 2002;49(1):14-18.
27. Messieha ZS, Ananda RC, Hoffman WE, et al. Bispectral Index System (BIS) monitoring reduces time to discharge in children requiring intramuscular sedation and general anesthesia for outpatient dental rehabilitation. Pediatr Dent. 2004;26(3):256-260.
28. Roelofse JA, Shipton EA, de la Harpe CJ, Blignaut RJ. Intranasal sufentanil/midazolam versus ketamine/midazolam for analgesia/sedation in the pediatric population prior to undergoing multiple dental extractions under general anesthesia: a prospective, double-blind, randomized comparison. Anesth Prog. 2004;51(4):114-121.
29. Abu-Shahwan I, Chowdary K. Ketamine is effective in decreasing the incidence of emergence agitation in children undergoing dental repair under sevoflurane general anesthesia. Pediatr Anesth. 2007;17:846-850.
30. Rai K, Hegde AM, Goel K. Sedation in uncooperative children undergoing dental procedures: a comparative evaluation of midazolam, propofol and ketamine. J Clin Pediatr Dent. 2007;32(1):1-4.
31. Damle SG, Gandhi M, Laheri V. Comparison of oral ketamine and oral midazolam as sedative agents in pediatric dentistry. J Indian Soc Pedod Prev Dent. 2008;26(3):97-101.
32. Padmanabhan MY, Pandey RK, Saksena AK, Chandra G. A comparative evaluation of agents producing analgo-sedation in pediatric dental patients. J Clin Pediatr Dent. 2009;34(2):183-188.
33. Baygin O, Bodur H, Isik B. Effectiveness of premedication agents administered prior to nitrous oxide/oxygen. Eur J Anaesthesiol. 2010;27(4):341-346.
34. Zanette G, Micaglio M, Zanette L, et al. Comparison between ketamine and fentanyldroperidol for rectal premedication in children: a randomized placebo controlled trial. J Anesth. 2010;24(2):197-203.
35. Bahetwar SK, Pandey RK, Saksena AK, Chandra G. A comparative evaluation of intranasal midazolam, ketamine and their combination for sedation of young uncooperative pediatric dental patients: a triple blind randomized crossover trial. J Clin Pediatr Dent. 2011;35(4):415-420.
36. Pandey RK, Bahetwar SK, Saksena AK, Chandra G. A comparative evaluation of drops versus atomized administration of intranasal ketamine for the procedural sedation of young uncooperative pediatric dental patients: a prospective crossover trial. J Clin Pediatr Dent. 2011;36(1):79-84.
37. Mittal N, Goyal A, Gauba K, et al. A double blind randomized trial of ketofol versus propofol for endodontic treatment of anxious pediatric patients. J Clin Pediatr Dent. 2013;37(4):415-420.
38. Singh C, Pandey RK, Saksena AK, Chandra G. A comparative evaluation of analgo-sedative effects of oral dexmedetomidine and ketamine: a triple-blind, randomized study. Paediatr Anaesth. 2014;24(12):1252-1259.
39. Surendar MN, Pandey RK, Saksena AK, et al. A comparative evaluation of intranasal dexmedetomidine, midazolam and ketamine for their sedative and analgesic properties: a triple blind randomized study. J Clin Pediatr Dent. 2014;38(3):255-261.
40. Flores-Castillo D, Martínez-Rider R, Ruiz-Rodríguez S, et al. Subcutaneous midazolam with and without ketamine for sedation in children undergoing dental treatment: a pilot study. J Clin Pediatr Dent. 2015;39(4):382-386.
41. Zanaty OM, El Metainy SA. A comparative evaluation of nebulized dexmedetomidine, nebulized ketamine, and their combination as premedication for outpatient pediatric dental surgery. Anesth Analg. 2015;121(1):167-171.
42. Ceber M, Salihoglu T. Ketamine may be the first choice for anesthesia in burn patients. J Burn Care Res. 2006;27(5):760-762.
43. Heshmati F, Zeinali MB, Noroozinia H, et al. Use of ketamine in severe status asthmaticus in intensive care unit. Iran J Allergy Asthma Immunol. 2003;2(4):175-180.
44. Wood MN, Manley MC, Bezzina N, Hassan R. An audit of the use of intravenous ketamine for paediatric dental conscious sedation. Br Dent J. 2015;218(10):573-577.
45. Hasan MS, Chan L. Dexmedetomidine and ketamine sedation for dental extraction in children with cyanotic heart disease. J Oral Maxillofac Surg. 2014;72(10):1920.e1-e4.
46. Horacek J, Palenicek T, Malek J, et al. The influence of clonidine on oral ketamine-midazolam premedication in intellectually disabled patients indicated for dental procedures: double-blind comparison of two sedation regimes. Neuro Endocrinol Lett. 2012;33(4):380-384.
47. Shirakami G, Tanimoto K, Matsuura S, Fukuda K. Ambulatory anesthesia for an adult patient with autism and epilepsy: sedation using oral and intravenous dexmedetomidine. Masui. 2008;57(6):735-738.
48. Saxen MA, Wilson S, Paravecchio R. Anesthesia for pediatric dentistry. Dent Clin North Am. 1999;43(2):231-245.
49. Rogerson CM, Abulebda K, Hobson MJ. Association of BMI with propofol dosing and adverse events in children with cancer undergoing procedural sedation. Hosp Pediatr. 2017;7(9):542-546.
50. Street MH, Gerard JM. A fixed-dose ketamine protocol for adolescent sedations in a pediatric emergency department. J Pediatr. 2014;165(3):453-458.
51. Kinder KL, Lehman-Huskamp KL, Gerard JM. Do children with high body mass indices have a higher incidence of emesis when undergoing ketamine sedation? Pediatr Emerg Care. 2012;28(11):1203-1205.
52. Ahmed SS, Hicks SR, Slaven JE, Nitu ME. Deep sedation for pediatric dental procedures: is this a safe and effective option? J Clin Pediatr Dent. 2016;40(2):156-160.