Use of Fluoride Products for Young Patients at High Risk of Dental Caries
Abstract:
Extensive education in oral hygiene home care, nutrition counseling, and routine reinforcement of home-care instructions at periodic check-ups lead to better oral health for many young children and teenagers. In addition, resistance to dental caries infection can be increased significantly by intelligent use of bonded resin sealants and systemic and topical fluoride products. This article discusses protocols for use of in-office applied topical fluoride and daily at-home use of topical fluoride products for children and teens at high risk of dental caries.
No matter how successful efforts in preventive dentistry may be for young patients, dentists who treat children and teens routinely encounter patients who continually develop dental caries. Some patients may simply be too young and possibly lack the required manual dexterity or the ability to understand lessons regarding brushing and flossing. Others may have parents or caregivers who are unable or unwilling to perform ideal oral health home care for their youngsters on a daily basis. In addition, socioeconomic factors and poor dietary choices may further place some children and teenagers at greater risk of dental caries. In preadolescent and adolescent orthodontic patients, poor oral healthcare is all too common, often because they lack motivation to take meticulous care of their teeth, and parents have declining influence on their maturing children’s personal behavior.
In the authors’ experience, children at high risk of dental caries can benefit from intensive exposure of their teeth to certain topical fluoride products more frequently than usual, to enhance their resistance to cariogenic acid challenges. Tinanoff1 described the “pre-eruptive” and “post-eruptive” influences of fluoride on human enamel. An important view is that the role of continuing frequent topical fluoride exposure has become known as much more critical than any systemic influence. This does not demean the role of systemic fluoride in the first 13 to 15 years of life; it merely emphasizes the importance of the topical effect.
Tinanoff also revealed the complexities of topical application of fluoride products both in the dental office (professional fluoride solutions and varnishes) and at home (fluoridated toothpastes, rinses, concentrated gels and pastes supplied by dentists or prescription). Issues such as compliance, adult supervision, ingestion of fluoride-containing products (with respect to fluorosis of developing permanent teeth), frequency of use, and nature (chemistry) of individual products all are considerations when one decides how to manage caries-prone young patients.
In the past several years, there has been concern in the profession for using evidence-based research to create guidelines for dental professionals and parents and guardians on the intelligent use of systemic and topical fluoride.2-6 Excessive ingested fluoride in the childhood years, when amelogenesis of permanent teeth is occurring, can cause varying severities of fluorosis.7,8 It is the aim of the dental profession to optimize the anti-dental caries benefits of systemic and topical fluoride use while avoiding the risk that permanent teeth will have intrinsic “enamel dysmineralization”9 associated with excess fluoride. Even though a vast majority of mild and moderate fluorosis can be eliminated or dramatically improved using enamel microabrasion and tooth bleaching methods,10-12 dentists still try to avoid fluorosis enamel color alterations from the start.
Concerns regarding the use of fluoride systemically and topically are not limited to dentistry professionals. Pediatricians have a keen interest in the subject and often are the first to advise parents regarding fluoride in infants, toddlers, and preschoolers. Lewis, who provided a thorough overview of the topic for the medical profession,13 described the characteristics of an ideal dental fluoride product for home use as follows:
• high fluoride uptake into enamel to decrease enamel solubility and interfere with plaque-borne bacterial metabolism
• low fluoride concentration to limit fluoride ingestion
• availability of calcium and phosphate salts to shift the remineralization/demineralization dynamics in the direction of re-mineralization
• good flavor, pleasant to use for the child
• non-irritating to gingival tissues and surrounding mucosa, and biocompatible
With all the above in mind, this article offers protocols for use of “in-office” applied topical fluoride and daily “at-home” use of topical fluoride products for children and teens at high risk of dental caries. The protocols take into consideration safety (to minimize ingestion of the material), costs, practicality, efficacy, frequency of intervention, and types of fluoride products to be used.
In-Office Fluoride
Traditionally, routine preventive dentistry visits for children have been scheduled at 6-month intervals. Such visits generally include an examination, dental prophylaxis, and tray application of fluoride solution. The tray application now is being supplanted by fluoride varnish application. The authors recommend that at-risk patients be seen every 2, 3, or 4 months for such preventive visits. Frequency of such visits can be judged by the dentist and dental hygienist subjectively, depending on an individual patient’s needs and personal or parental (caregiver) home oral healthcare performance. Of course, the frequency can change to more visits, or fewer, as home care improves, or not. Extra professional rubber-cup rotary tooth cleanings are not always needed at each visit; a complete dental cleaning using floss and a toothbrush, and a brush application of topical fluoride solution, followed by a generalized application of fluoride varnish, can be sufficient and achieved rapidly.
Of course, additional attention is required for patients who develop calculus and superficial extrinsic stain. A dental hygienist or assistant (as permitted by state regulations) should perform these services while reinforcing brushing and flossing education for parents and patients. In some dental offices, these added preventive appointments are offered at a greatly reduced or no additional fee, depending on office policies and frequency required.
At-Home Fluoride
Parents or other caregivers are the most important partners in the efforts to achieve a caries-free childhood for their children. They need to supervise and assure that older children and youngsters in orthodontic hardware who are capable of their own home care are actually doing it well. They should also provide hands-on assistance to most children under 10 years of age.14
For high-caries-risk toddlers, preschoolers, and elementary school–aged children, routine after-breakfast and before-bedtime brushing and flossing can be achieved rapidly and efficiently using the “from behind” approach. For this, the child’s head rests in the cradle of the caregiver’s hip and the non-brushing hand supports the child’s head (Figure 1). Using a small dab of the recommended fluoride gel or toothpaste, a thorough brushing can be achieved. Flossing then is performed between contacting teeth (Figure 2). The fluoride solution is carried into proximal spaces with the floss.
Fluoride dentifrices or gels with much more fluoride content than commercial toothpastes are used to enhance enamel exposure and uptake. For many years, 5,000-ppm sodium fluoride toothpastes and gels have been available from dentists directly, or by prescription. Although rinsing with water should be avoided after such fluoride-rich brushing and flossing, care should be taken to wipe away excess fluid, or have the child expectorate, to minimize ingestion of saliva containing the gel or dentifrice.
High-caries-risk children and teens wearing fixed orthodontic hardware need to be taught about angulating brush bristles and judicious use of floss, inserted with floss threaders, while using concentrated fluoride dentifrice products at home (Figure 3 and Figure 4). Figure 3 demonstrates brush bristles extending underneath arch wires and in-between bonded brackets for complete removal of biofilm, plaque, and food debris.
New Fluoride Options for Home Use
New products are being introduced with the intention of helping young patients and their caregivers improve at-home caries prevention efforts. For example, Premier® Dental Products Co. ( www.premusa.com) has introduced Enamelon® Preventive Treatment Gel and Enamelon® Toothpaste. Unlike 5,000-ppm sodium fluoride gels and toothpastes, the Enamelon products are formulated with stannous fluoride. Also, calcium and phosphate salts have been incorporated to provide an additional source of bioavailable mineralizing ions. These ions are intended to work synergistically with the available fluoride to support remineralization and inhibit demineralization. Two highly substantive polymer carriers are also included in the formulas. These agents aid in decreasing the ability of biofilm to adhere to enamel and help to retain the remineralizing agents on the tooth surface significantly longer. Spilanthes, a natural flavorant, is also included to enhance saliva production. Moreover, the Enamelon products are free of sodium laurel sulfate (SLS), die, and gluten.
The value of stannous fluoride (SnF2) formulations in preventive dentistry has been established for several decades. In an important review of the use of stannous fluoride products, Tinanoff reported how inclusion of the tin ion in stannous fluoride dentifrices decreases gingivitis, has an antibacterial effect—particularly on Streptococcus mutans—and also has an anticaries influence.15
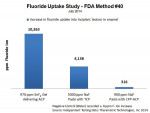
According to the manufacturer, a “pea-sized” (0.25 grams) portion of Enamelon Preventive Treatment Gel (970 ppm fluoride content) (Figure 5) contains 0.24 mg of fluoride, versus 1.25 mg of fluoride in an identical volume of paste in a typical 5,000-ppm fluoride ion prescription-strength toothpaste. When these two products were tested for enamel fluoride uptake (using method #40 in the US FDA Anticaries Drug Products for OTC Human Use, Final Monograph testing procedures), the Enamelon Preventive Treatment Gel (970 ppm F- ion) provided nearly 2-½ times greater increase in fluoride uptake into incipient lesions in enamel than the 5,000-ppm fluoride ion prescription-strength toothpaste. Additionally, the Enamelon Preventive Treatment Gel provided a 30 times greater increase in fluoride uptake into incipient lesions in enamel than a 900-ppm fluoride ion product containing casein phosphopeptide-amorphous calcium phosphate (CCP-ACP) (Figure 6) (independent testing data: Therametric Technologies, Inc., 2014).
With up to 80% less fluoride than the 5,000-ppm F- ion prescription-strength toothpastes, Enamelon may be able to achieve this greater fluoride uptake into incipient lesions due to the bioavailability of the amorphous calcium phosphate. There is a growing body of literature showing how calcium and phosphate supplementation of fluoride treatments can enhance fluoride uptake.16-19 Schemehorn et al demonstrated that a fluoride toothpaste simultaneously delivering calcium and phosphate salts released about 2-½ times as much fluoride into lesioned enamel compared to a reference toothpaste containing a similar amount of fluoride.20
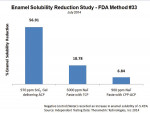
The Enamelon products were then tested to assess resistance of enamel to acid challenges (using method #33 in the US FDA Anticaries Drug Products for OTC Human Use, Final Monograph testing procedures). The Enamelon Preventive Treatment Gel (970 ppm F- ion) provided 3 times greater reduction in enamel solubility than the 5,000-ppm fluoride ion prescription-strength toothpaste and 8 times greater reduction than the 900-ppm fluoride ion product containing CCP-ACP (Figure 7) (independent testing data: Therametric Technologies, Inc., 2014).
For adult patients with exposed root surfaces, Enamelon’s combination of stannous fluoride ions with calcium and phosphate salts occlude dentinal tubules, helping to alleviate discomfort from dentinal hypersensitivity. The authors recommend studies to determine if similar relief from tooth sensitivity can be achieved in teeth with enamel hypoplasia and hypocalcification.21 More studies are underway to determine the full extent of the remineralization dynamics associated with the Enamelon products and the increased resistance of enamel to acid challenge.
Figure 8 through Figure 11 depict Enamelon in use, showing the process of thorough brushing in a toddler whose parents needed multiple lessons in proper home care for their 3-year-old.
Conclusion
The authors acknowledge that the above recommendations are subjective, and there are no studies verifying the exact value of either of these “in-office” or “at-home” models of fluoride use. However, based on logic and decades of experience using these practices, these recommendations are thought to be useful, sensible, and in complete harmony with current recommendations by the American Dental Association and American Academy of Pediatric Dentistry. Controlled clinical studies are encouraged to shed more light on the value of fluoride-use protocols using Enamelon products.
It is important to explain the nature and use of these concentrated stannous fluoride products to parents and especially to children old enough to understand the purpose of these protocols. To date, patients have reported that the Enamelon products have a pleasant taste, and parents have been compliant with having their children use the new gel and toothpaste. In view of the lower amount of fluoride content in the treatment gel, the increased fluoride uptake shown in Figure 6, and the increased resistance to acid challenge of treated enamel as shown in Figure 7, the authors expect Enamelon Gel to be a valuable preventive dentistry adjunct in the overall care of high-caries-risk children and teenagers, especially those wearing fixed orthodontic appliances.
About the Authors
Theodore P. Croll, DDS
Affiliate Professor, Department of Pediatric Dentistry, University of Washington School of Dentistry, Seattle, Washington; Adjunct Professor, Department of Pediatric Dentistry, University of Texas Health Science Center at San Antonio, San Antonio, Texas; Private Practice, Doylestown, Pennsylvania
Joel H. Berg, DDS, MS
Dean, University of Washington School of Dentistry, Seattle, Washington
REFERENCES
1. Tinanoff N. Use of fluoride. In: Berg JH, Slayton RL, eds. Early Childhood Oral Health. Ames, Iowa: John Wiley & Sons; 2009:92-109.
2. Tinanoff N. Policy on Use of Fluoride. Council on Clinical Affairs, American Academy of Pediatric Dentistry. Pediatric Dentistry. 2012;34:43-44.
3. Tinanoff N. Guidelines on Fluoride Therapy. Council on Clinical Affairs, American Academy of Pediatric Dentistry. Pediatric Dentistry. 2012;34:162-165.
4. Weyant RJ, Tracy SL, Anselmo TT, et al. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2013;144(11):1279-1291.
5. Wright JT, Hanson M, Ristic H, et al. Fluoride toothpaste efficacy and safety in children younger than 6 years: a systematic review. J Am Dent Assoc. 2014;145(2):182-189.
6. American Dental Association Council on Scientific Affairs. Fluoride toothpaste use for young children. J Am Dent Assoc. 2014;145(2):190-191.
7. DenBesten PK. Biological mechanisms of dental fluorosis relevant to the use of fluoride supplements. Community Dent Oral Epidemiol. 1999;27(1):41-47.
8. Aoba T, Fejerskov O. Dental fluorosis: chemistry and biology. Crit Rev Oral Biol Med. 2002;13(2):155-170.
9. Croll TP. Enamel microabrasion for removal of superficial dysmineralization and decalcification defects. J Am Dent Assoc. 1990;120(4):411-415.
10. Cvitko E, Swift EJ Jr, Denehy GE. Improved esthetics with a combined bleaching technique: a case report. Quintessence Int. 1992;23(2):91-93.
11. Killian CM. Conservative color improvement for teeth with fluorosis-type stain. J Am Dent Assoc. 1993;124(5):72-74.
12. Croll TP. Esthetic correction for teeth with fluorosis and fluorosis-like enamel dysmineralization. J Esthet Dent. 1998;10(1):21-29.
13. Lewis CW. Fluoride and dental caries prevention in children. Pediatr Rev. 2014;35(1):3-15.
14. Croll TP. ASDC Kids Mouth Book. 2nd ed. Chicago, IL: American Society of Dentistry for Children; 1999.
15. Tinanoff N. Progress regarding the use of stannous fluoride in clinical dentistry. J Clin Dent. 1995;6(spec no):37-40.
16. Hong YC, Chow LC, Brown WE. Enhanced fluoride uptake from mouthrinses. J Dent Res. 1985;64(2):82-84.
17. Crall JJ, Bjerga JM. Enamel fluoride retention after DCPD and APF application and prolonged exposure to fluoride in vitro. J Dent Res. 1986;65(3):387-389.
18. Schreiber CT, Shern RJ, Chow LC, Kingman A. Effects of rinses with an acidic calcium phosphate solution on fluoride uptake, caries and in situ plaque pH in rats. J Dent Res. 1988;67(6):959-963.
19. Chow LC, Guo MK, Hsieh CC, Hong YC. Apatitic fluoride increase in enamel from a topical treatment involving intermediate CaHPO4 .2H2O formation, an in vivo study. Caries Res. 1981;15(5):369-376.
20. Schemehorn BR, Wood GD, Winston AE. Laboratory enamel solubility reduction and fluoride uptake from enamelon dentifrice. J Clin Dent. 1999;10(1 spec no):9-12.
21. Croll TP. Treatment options for hypoplastic and hypocalcified permanent molars in children. Inside Dentistry. 2014;10(8):58-66.