Dental Implant Therapy in Patients with a History of Periodontitis: A Literature Review and Clinical Considerations
Abstract
Inflammatory periodontal disease is regarded as a leading cause of tooth loss in the adult population. As an increasing number of patients elect dental implants to replace tooth loss due to periodontal disease, the influence of this disease on the survival of implants needs to be considered. Patients with a history of periodontal disease represent a unique group of potential candidates for dental implant therapy, therefore it is important to address the management and rate of survival of implants in these patient types. Based upon the literature investigated, the authors observed that when patients with a history of periodontal disease were compared to individuals who were periodontally healthy, the former group manifested significantly greater peri-implant marginal bone loss with a higher incidence of peri-implantitis. With this in mind, dental implant therapy remains a viable option with proper patient selection. It was concluded that the rate of implant survival was acceptable in patients with a history of periodontal disease in periodontal maintenance programs.
Dental implants have become widely recognized as a treatment modality in patients with tooth loss. As an increasing number of patients receive implant therapy to replace missing teeth due to periodontal disease, the question arises as to whether the outcome of dental implants is influenced by a history of periodontitis.1 This patient population is believed to carry an increased risk for implant failure, increased probing depths, and progressive bone loss around implants.2-4 Because inflammatory periodontal disease is regarded as a leading cause of tooth loss in the adult population, the issue in regards to successful implant placement becomes a major consideration for the clinician in treatment planning patients with a history of periodontal disease.5
The literature currently indicates no significant difference in the rate of implant survival between patients with a history of periodontitis and periodontally healthy individuals after 5-year follow-up; however, studies show that patients with a history of periodontitis manifest greater probing depths, more marginal bone loss surrounding implants, and a higher incidence of peri-implantitis.6,7 With carefully monitored supportive periodontal therapy (SPT) and proper management, clinical studies show implant survival at 5- and 10-year follow-up to prove dental implants to be a successful treatment modality with a predictable outcome.2
Periodontal Health
Periodontitis comprises a variety of pathologic conditions that affect the health of the periodontium and is commonly seen in its chronic form.8 In general, patients exhibit gingival inflammation with destruction of tooth-supporting structures including the periodontal ligament, connective tissue, and bone.8,9 Aggressive periodontitis (AP) forms are characterized by rapid attachment loss and alveolar bone destruction in otherwise systemically healthy individuals.10 It has been suggested that patients with aggressive forms of periodontitis are at higher risk for implant failure in comparison to their chronic counterparts.2 Al-Zahrani et al demonstrated 5-year survival rates of 89% in AP patients undergoing SPT; however, bone loss occurred more often in these patients in comparison to patients with chronic periodontitis and periodontally healthy individuals.10
Numerous studies have indicated the composition of bacteria associated with chronic periodontitis and peri-implantitis to be similar, with predominantly gram-negative anaerobes.6,11 Shibli et al demonstrated that implants associated with peri-implantitis showed the same bacterial composition associated with healthy implants; however, higher quantities of bacteria were found at the diseased sites.6,12,13 In partially edentulous patients, periodontal pathogens have been shown to translocate from periodontally involved teeth to the sulcus surrounding implants in the partially edentulous patient.8,14 This highlights the importance of supportive periodontal therapy and treatment of involved teeth prior to the placement of dental implants. With this in mind, extraction of hopeless teeth, ridge augmentation, and possible socket preservation may lengthen treatment duration prior to implantation. Furthermore, the presence of periodontal inflammation and periapical lesions often delays the placement of bone grafts and further placement of implants. 15,16
The current literature demonstrates favorable results among patients with a previous history of periodontitis, with survival rates ranging from 79% to 92.8% at the 10-year follow-up (Table 1).17-23 Inclusion criteria consisted of a control group of periodontally healthy subjects with at least a 3-year follow-up status. Studies also frequently reported marginal peri-implant bone loss, revealing comparable results in both group populations. According to Hardt and colleagues, overall implant survival rates of 94.8% were demonstrated, with a survival rate of 92% in patients with chronic periodontitis and 96.7% in periodontally healthy patients.17 In comparing differences in mean bone loss after 5 years between these two groups, there were no statistically significant differences found; periodontitis subjects showed loss of 2.2 mm at 5 years and periodontally healthy subjects demonstrated 1.7 mm.17 A 10-year prospective study conducted by Karoussis et al found that, although patients with a previous history of periodontal disease had a significantly higher incidence of peri-implantitis (28.6% vs. 5.8%) than their healthy counterparts, implant survival rates were still clinically favorable, with results of 90.5% seen in patients with a past history of chronic periodontitis compared to 96.5% in periodontally healthy subjects.18
Patients with generalized aggressive periodontitis (GAP) did demonstrate a higher failure rate than chronic periodontitis patients as well as periodontally healthy subjects. Mengel et al found that implant survival rate after 10 years was 83.33% in patients with GAP in comparison to 100% in periodontally healthy patients.22 Studies also show an increase in interleukin-1 beta (IL-1ß) in patients with GAP. Throughout the course of the study, periodontal health was shown to continually decline in patients with GAP, even in the presence of maintenance and plaque-control programs.
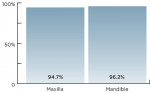
Supportive periodontal therapy was shown to be an effective method of periodontal maintenance when placing implants in patients with chronic periodontitis. Roccuzzo and colleagues demonstrated successful management of implants, with a survival rate of 94.7% in 15 of the subjects with a history of advanced periodontitis who were maintained and treated periodontally before implants were placed.23 A lack of compliance to SPT was correlated with a higher incidence of marginal peri-implant bone loss at follow-up as well as an increased incidence of implant failure. Furthermore, a higher implant survival rate was observed in the mandible (96.2%) than in the maxilla (93.5%).23
Discussion
The survival rates of implants were generally high in all subject groups, including chronic and aggressive forms of periodontitis; the survival of implants was not significantly different in individuals with periodontal disease and periodontally healthy subjects after 5- and 10-year follow-up. When comparing outcomes, implant placement in patients with periodontal disease, peri-implantitis, bleeding on probing, and radiographic signs of marginal bone loss was significantly higher. Karoussis and colleagues reported peri-implantitis around eight of the 21 implants (38%) in eight patients in the periodontitis group in comparison to five of the 91 implants (5%) in five periodontally healthy patients (Figure 1).18 In comparing progressive bone loss around implants, 64% of subjects with periodontitis demonstrated > 2 mm of bone loss at 5 years in comparison to 24% of periodontally healthy patients (Figure 2).17
Implant failure was frequently shown to be higher in the maxilla when compared with implants placed in the mandible.14,21,24 Leonhardt et al demonstrated a 94.7% success rate in implants placed in the maxilla in comparison to a 96.2% survival in those placed in the mandible at a 10-year follow-up, suggesting a possibility of intraoral location differences (Figure 3).14
Supportive periodontal therapy, defined as regular visits to the clinician for periodontal control and maintenance, formed the basis of long-term success after periodontal implant placement.25 SPT was shown to be an effective method in maintaining implant success and preventing periodontitis recurrence. All patients revealed improvement in plaque control, with statistically significant differences between initial plaque scores and 10-year follow-up values.23 Patients with chronic periodontitis who did not completely adhere to SPT demonstrated a higher incidence of implant loss.23
Prophylactic antibiotics are frequently administered prior to placement of implants to minimize the risk of infection. Amoxicillin is commonly prescribed pre- and postoperatively in addition to a chlorhexidine rinse. Studies have shown an increased incidence of infection after implant placement in periodontitis-susceptible individuals.26
Currently, innovative methods exist for the clinician in screening patients for increased risk factors for periodontal disease. Among them are salivary diagnostic tests, which evaluate the composition of individual saliva samples, indentifying individual genetic susceptibility to periodontal disease by evaluating samples for high-, moderate-, and low-risk pathogens, as well as interleukin-1 alpha (IL-1α) and IL-1β, potential inflammatory mediators associated with periodontal disease.27 The assessment of salivary composition aids the dental clinician in determining periodontal disease types, therapeutic treatment options, and whether the need for more aggressive treatment is required. The effectiveness of salivary diagnostic tests, however, has yet to be elucidated.
In reviewing the literature, there has been no appropriate scientific evidence to conclude definitively that individuals with a previous history of periodontitis demonstrate increased failure rates when rehabilitated with dental implants. Many studies lacked control groups when reporting implant survival rates in periodontal patients, and sample sizes were frequently small and possibly not large enough to detect significant values. Variables such as whether implants were single units or multiple-unit bridges, and whether placement was immediate or delayed were frequently not reported. The current literature should be interpreted with caution, as further research is necessary to ascertain the role of risk factors in the progression of periodontal disease.
Conclusion
Patients with a history of periodontal disease should be informed that there is a higher risk of peri-implant disease. The survival of dental implants in this population was not significantly different from periodontally healthy patients. However, patients with a history of periodontitis demonstrate a significantly higher frequency of peri-implantitis and peri-implant bone loss. Supportive periodontal therapy seems to be a key factor in enhancing long-term implant survival.
With proper management and patient compliance, the literature suggests that clinically acceptable results can be achieved when placing dental implants in patients with a history of periodontitis. However, there is a need for stronger evidence in the form of longitudinal studies in much larger samples in the future.
References
1. Heitz-Mayfield LJ, Huynh-Ba G. History of treated periodontitis and smoking as risks for implant therapy. Int J Oral Maxillofac Implants. 2009;24(suppl):39-68.
2. Safii S, Palmer RM, Wilson RF. Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: a systematic review and meta analysis. Clin Implant Dent Relat Res. 2010;12(3):165-174.
3. Tonetti MS, Schmid J. Pathogenesis of implant failures. Periodontol 2000. 1994;4:127-138.
4. Esposito M, Hirsch JM, Lekholm U, Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur J Oral Sci. 1998;106(3):721-764.
5. Nevins M, Langer B. The successful use of osseointegrated implants for the treatment of the recalcitrant periodontal patient. J Periodontol. 1995;66(2):150-157.
6. Greenstein G, Cavallaro J Jr, Tarnow D. Dental implants in the periodontal patient. Dent Clin North Am. 2010;54(1):113-128.
7. Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 2007;18(6):669-679.
8. Evian CI, Emling R, Rosenberg ES, et al. Retrospective analysis of implant survival and the influence of periodontal disease and immediate placement on long-term results. Int J Oral Maxillofac Implants. 2004;19(3):393-398.
9. Listgarten MA. Pathogenesis of periodontitis. J Clin Periodontol. 1986;13(5):418-430.
10. Al-Zahrani MS. Implant therapy in aggressive periodontitis patients: a systematic review and clinical implications. Quintessence Int. 2008;39(3):211-215.
11. Paster BJ, Boches SK, Galvin JL, et al. Bacterial diversity in human subgingival plaque. J Bacteriol. 2001;183(12):3770-3783.
12. Ong CT, Ivanovski S, Needleman IG, et al. Systematic review of implant outcomes in treated periodontitis subjects. J Clin Periodontol. 2008;35(5):438-462.
13. Shibli J, Melo L, Ferrari DS, et al. Composition of supra- and subgingival biofilm of subjects with healthy and diseased implants. Clin Oral Implants Res. 2008;19(10):975-982.
14. Leonhardt A, Gröndahl K, Bergström C, Lekholm U. Long-term follow-up of osseointegrated titanium implants using clinical, radiographic and microbiological parameters. Clin Oral Implants Res. 2002;13(2):127-132.
15. Schou S, Holmstrup P, Worthington HV, Esposito M. Outcome of implant therapy in patients with previous tooth loss due to periodontitis. Clin Oral Implants Res. 2006;17(suppl 2):104-123.
16. Bencharit S, Schardt-Sacco D, Border MB, Barbaro CP. Full mouth rehabilitation with implant-supported prostheses for severe periodontitis: a case report. Open Dent J. 2010;4:165-171.
17. Hardt CR, Gröndahl K, Lekholm U, Wennström JL. Outcome of implant therapy in relation to experienced loss of periodontal bone support: a retrospective 5-year study. Clin Oral Implants Res. 2002;13(5):488-494.
18. Karoussis IK, Salvi GE, Heitz-Mayfield LJ, et al. Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2003;14(3):329-339.
19. Rosenberg E, Cho S, et al. A comparison of characteristics of implant failure and survival in periodontally compromised and periodontally healthy patients: a clinical report. Int J Oral Maxillofac Implants. 2004;19(6):873-879.
20. Evian C, Emling R, Rosenberg ES, et al. Retrospective analysis of implant survival and the influence of periodontal disease and immediate placement on long-term results. Int J Oral Maxillofac Implants. 2004;19(3):393-398.
21. Mengel R, Flores-de-Jacoby L. Implants in patients treated for generalized aggressive and chronic periodontitis: a 3-year prospective longitudinal study. J Periodontol. 2005;76(4):534-543.
22. Mengel R, Behle M, Flores-de-Jacoby L. Osseointegrated implants in subjects treated for generalized aggressive periodontitis: 10-year results of a prospective, long-term cohort study. J Periodontol. 2007;78(12):2229-2237.
23. Roccuzzo M, De Angelis N, Bonino L, Aglietta M. Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: implant loss and radiographic bone loss. Clin Oral Implants Res. 2010;21(5):490-496.
24. Mengel R, Schröder T, Flores-de-Jacoby L. Osseointegrated implants in patients treated for generalized chronic periodontitis and generalized aggressive periodontitis: 3- and 5-year results of a prospective long-term study. J Periodontol. 2001;72(8):977-989.
25. Quirynen M, Abarca M, Van Assche N, et al. Impact of supportive periodontal therapy and implant surface roughness on implant outcome in patients with a history of periodontitis. J Clin Periodontol. 2007;34(9):805-815.
26. Rosenquist B, Grenthe B. Immediate placement of implants into extraction sockets: implant survival. Int J Oral Maxillofac Implants. 1996;11(2):205-209.
27. Tsai CC, Ho YP, Chen CC. Levels of interleukin-1 beta and interleukin-8 in gingival crevicular fluids in adult periodontitis. J Periodontol. 1995;66(10):852-859.
About the Authors
Michael Courtney, DMD, MA
Goldman School of Dental Medicine
Boston University
Boston, Massachusetts
David Cottrell, DMD
Associate Professor
Director of Residency Training in Oral and Maxillofacial Surgery
Goldman School of Dental Medicine
Boston University
Boston, Massachusetts
Srinivas Ayilavarapu, BDS, CAGS, DSc
Associate Professor of Periodontology
Goldman School of Dental Medicine
Boston University
Boston, Massachusetts