Performing Orthodontics While Treating OSA
Comprehensive treatment planning is essential to avoid malocclusion
Payam Ataii, DMD, MBA
According to practice parameters published jointly by the American Academy of Sleep Medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM), oral appliance therapy is an effective treatment option for snoring and obstructive sleep apnea (OSA).1,2 The parameters note that when patients are diagnosed with OSA, dentists should provide them with a "custom, titratable appliance over non-custom oral devices" as an alternative to continuous positive airway pressure (CPAP) therapy.1,2
More recently, the American Dental Association (ADA) approved and published an 11-point position statement outlining the role of dentistry in the treatment of sleep-related breathing disorders. Among the many recommendations, the ADA specifies that "a dentist should be the one to fabricate an oral appliance" when treating patients diagnosed with OSA.3
Despite these great practice parameters and position statements, none of these organizations specify which types of oral appliances to choose and, most importantly, what treatment philosophy should be used when treating these patients. These considerations are important because treatment with the most common types of oral appliances for snoring and airway patency has been known to produce unintended consequences, such as creating suboptimal movement of teeth.4
Others have observed that "the use of sleep appliances, which anteriorly reposition the mandible, may produce posterior open bites and maxillary retrusion."5 Therefore, it has been recognized that when utilizing sleep appliances, the design of the appliance and the management of the occlusion are important clinical considerations.6
Depending on the practitioner's treatment philosophy and experience, selection of an oral sleep appliance can become challenging if the patient presents with OSA and malocclusions.
This article will examine two different patients with a diagnosis of mild to moderate OSA and similar apnea-hypopnea index (AHI) scores who were treated using two different treatment philosophies. Comparing these cases highlights the necessity of proper treatment planning and appliance selection when treating patients who suffer from sleep disorders as well as the need for regular, long-term follow-up of these patients.
Case Report No. 1
A 61-year-old man presented with the chief complaint of wanting to have "straighter, whiter teeth." An initial malocclusion exam revealed a Class I skeletal bite with minor lower anterior crowding of < 5 mm and flat, worn down lower incisors with a 1-mm overjet on anterior coupling (Figure 1). Treatment options were reviewed, and a clear aligner treatment plan was accepted by the patient and started shortly after. Correction of the malocclusion was accomplished using clear aligner therapy for a period of 11 months (Figure 2).
During the orthodontic exit assessment, the patient noted experiencing excessive sleepiness and was sent for a sleep study. After taking a home sleep test that resulted in an AHI score of 7.5 in the supine position, he received a diagnosis of mild sleep apnea from a physician. The AHI score indicates the number of times per hour that a patient stopped breathing due to blockage of the airway. To address the patient's airway obstruction, a mandibular repositioning device (MRD) was fabricated (Figure 3). He was also given a morning occlusal guide, which helps reposition the mandible to its pretreatment position by utilizing biting force to reseat the condyles, reestablishing the appropriate occlusal relationship following each night of oral appliance therapy.7 The patient's symptoms were stabilized, and he reported that he was sleeping more and feeling better. Unfortunately, he then moved to another state, and further follow-up was not possible.
Five years later, the patient returned to the office, and an examination revealed that he had developed an anterior bite in an end-to-end relationship. This resulted in moderate to locally severe anterior dental wear and a slight crossbite. He had also developed a unilateral posterior open bite as a result of molar shifting (Figure 4 through Figure 6). The patient reported that he was diligently wearing his oral appliance nightly. He also reported that he was periodically using the morning occlusal guide and felt "it was working." However, during chewing, he was suffering from intermittent, painful cheek biting.
To correct the patient's current malocclusion while also addressing his airway deficiencies, a new treatment plan was developed. The plan involved the provision of combination therapy to simultaneously treat the malocclusions using clear aligners and the OSA using an FDA-approved custom sleep appliance designed to be worn on top of the aligners (Aligner Sleep Appliance®, SleepArchiTx™). With this combination treatment plan, the patient was able to change the aligners and progress on to the next set while also wearing the appliance at night, keeping the airway patent. As the teeth are moved into the proposed positions by the clear aligners, expansion screws on the upper and lower components of the appliance enable it to be adjusted to follow their treatment path. Because the appliance can sit on top of clear aligner trays during any stage of treatment, the clinician has the opportunity to use the same sleep appliance after the completion of orthodontic treatment if he or she chooses to use clear aligners as a retention option (Figure 7).
After 6 months of clear aligner re-treatment, the posterior open bite tracked and was brought back into occlusion, and the end-to-end anterior crowding was resolved (Figure 8). The patient reported that he was no longer experiencing cheek biting and noted that his "back teeth have a bite now."
Case Report No. 2
A 57-year-old man presented with the chief concern of achieving a better smile and suggested potentially replacing his current upper anterior crowns because the gray metal had become visible at the gumline. An oral examination revealed a unilateral class I skeletal occlusion on the patient's right side, a missing molar with drifted space closure on the patient's left side, and a rotation of the opposing bicuspid (ie, No. 13)-all of which had been remodeling into his current occlusion for over 30 years without notable symptoms. The upper and lower anterior arches exhibited < 1 mm of overjet with mild lower anterior overlapping of the incisors (ie, < 4 mm) (Figure 9 through Figure 13). The patient also suffered from excessive daytime sleepiness, which was scored as mild to severe using the Epworth Sleepiness Scale. He was scheduled for a sleep study and was subsequently diagnosed with mild to moderate OSA after receiving an AHI score of 7.
Because the patient suffered from both airway deficiencies and malocclusion, the treatment options presented to him included the option of using CPAP therapy at night along with clear aligners to resolve the lower crowding and gain better upper overjet prior to replacing the crowns on teeth Nos. 8 and 9. However, the patient refused CPAP therapy and instead accepted an alternative treatment plan that called for combination therapy using clear aligners for the orthodontic movement in conjunction with a sleep appliance to help improve his OSA. He was fitted for both devices at the same time and instructed to change the clear aligners weekly and wear the appliance at night during sleep.
At the 2-week follow-up visit, the patient stated that he "felt better right away" and was "getting better rest at night" (Figure 14). The clear aligner treatment plan was finalized to address only the anterior malocclusions, without the rotation of the bicuspid or molar movements, because the patient had no desire to extend the length of treatment beyond what was necessary to resolve his cosmetic concerns and airway deficiencies.
The total clear aligner treatment time lasted less than 1 year. The lower incisor crowding was resolved with an improved anterior overjet of 1 mm, gaining an ideal envelope of function for the upper restorations. During the time of tooth movement, the sleep appliance was adjusted to move along with the clear aligners. In this manner, the mandible was advanced anteriorly while the patient slept at night. At the conclusion of treatment, a follow-up sleep study was performed to ensure ideal airway patency and a reduction of the patient's OSA.
Six-weeks after the completion of orthodontic treatment, passive clear aligners with no built-in movements were ordered to start the restoration of the patient's upper anterior crowns. Because the sleep appliance selected utilizes the convergence of molars and bicuspids to advance the mandibular arch, it's lack of anterior coverage facilitates the performance of cosmetic work in this area without the need to fabricate a new appliance. The patient was advised to continue to wear the clear aligners over his provisional restorations and in conjunction with the sleep appliance at night throughout the restorative phase. After the crowns on teeth Nos. 8 and 9 were replaced, new clear aligners were fabricated over the final restorations to maintain retention in conjunction the same sleep appliance (Figure 15). The patient was placed on a 6-month recall schedule for appropriate follow-up.
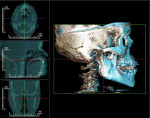
At the 5-year follow-up appointment, the patient exhibited little to no change in his occlusion and also demonstrated improvement in his home sleep test assessment. His OSA had been stabilized from an AHI score of 7 without the oral appliance to an AHI score of 3 with the appliance in place (An AHI score below 5 is considered to be within normal limits.). A cone-beam computed tomography scan of the patient's airway showed stability without constriction, and most importantly, there was no clinical evidence of the teeth shifting or the presence of any malocclusions.
About the Author
Payam Ataii, DMD, MBA
Private Practice
Laguna Hills, California
Conclusion
As evidenced by the contrast between the two cases, beyond following the practice parameters established by the AASM, the AADSM, and the ADA, selecting the proper oral appliance and appropriate treatment philosophy is imperative. Simply delivering any available sleep appliance is not sufficient to treat patients with sleep-related breathing disorders long-term. Clinicians should also include a comprehensive examination of the patient to identify any dental comorbidities, incorporate the joint restorative work needed to properly seat the sleep appliance, and select the most appropriate appliance given the unique condition of the patient's craniofacial complex. In addition, working in conjunction with medical doctors to not only determine the best route of care but also establish the efficacy of the sleep appliance with follow-up sleep studies is important.
These two cases also serve to highlight the importance of ongoing follow-up after delivery of an oral appliance. Because there was no follow-up with the patient in case report No. 1 until 5 years after treatment, there was no opportunity to observe the malocclusions that were forming as the patient wore the sleep appliance and, therefore, no opportunity to intervene. With the patient in case report No. 2, regular follow-up occurred on a long-term basis to ensure that no teeth were shifting and that the sleep appliance continued to function effectively. Regular, long-term follow-up care is essential to success when treating patients with sleep appliances. Indeed, a protocol for long-term follow-up is outlined in the AADSM guidelines.7
Disclosure
Payam Ataii, DMD, is the co-inventor of the Aligner Sleep Appliance® and a paid consultant for SleepArchiTx™.
References
1.Oral Appliance Therapy. American Academy of Dental Sleep Medicine. https://www.aadsm.org/oral_appliance_therapy.php Updated Aug. 7, 2015. Accessed November 30, 2018.
2. Ramar K, Dort C, Katz S, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. Journal of Clinical Sleep Medicine. 2015;11
(7):773-827.
3. American Dental Association. The Role of Dentistry in the Treatment of Sleep Related Breathing Disorders. ADA Website. https://www.ada.org/~/media/ADA/Member%20Center/FIles/The-Role-of-Dentistry-in-Sleep-Related-Breathing-Disorders.pdf?la=en. Accessed November 1, 2018.
4. Pliska BT, Nam H, Chen H, et al. Obstructive sleep apnea and mandibular advancement splints: occlusal effects and progression of changes associated with a decade of treatment. J Clin Sleep Med. 2014;10(12):
1285-1291.
5. Wilkerson DC, Lamberg S, Correa LP. What are the factors that cause malocclusion and how do prescribed sleep appliances affect occlusion? Inside Dentistry. 2018;14(6):34-36.
6. Ramar K, Dort LC, Katz SG, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Dent Sleep Med. 2015;2(3):71-125.
7. Sheats RD, Schell TG, Blanton AO, et al. Management of side effects of oral appliance therapy for sleep-disordered breathing. Journal of Dental Sleep Medicine. 2017;4(4):93-126.