Self-adhesive Resin Cements: Characteristics, Properties, and Manipulation
John M. Powers, PhD
Abstract
Self-adhesive resin cements have adhesive components that eliminate the need for separate etchants and primers for bonding to tooth, alloy, or ceramic substrates that are required with the use of other cementation alternatives. Today, a number of commercial self-adhesive resin cements are available. This article reviews the characteristics, properties, and manipulations/use considerations in general of self-adhesive resin cements.
Today, dentistry is rapidly moving from cementation of alloy-based restorations with traditional cements (eg, glass ionomer, resin-modified glass ionomer, zinc phosphate, zinc polycarboxylate) to bonding of all-ceramic restorations with resin-based cements. These resin-based cements include esthetic resins, adhesive resins, and self-adhesive resins.
Esthetic resin cements are tooth-colored or translucent cements based on diacrylate resin that require a bonding agent for adhesion to tooth structure and separate primers for bonding to metal and ceramic substrates. Adhesive resin cements are based on acrylic or diacrylate resin with adhesive monomers that bond well to metal sub-strates. Adhesive resin cements may require a separate primer for bonding to ceramic, metal, and tooth substrates. Self-adhesive resin cements have adhesive components that eliminate the need for separate etchants and primers for bonding to tooth, alloy, or ceramic substrates, and a number of commercial self-adhesive resin cements are available (Table 1).
Composition and Reaction of Self-adhesive Resin Cements
Self-adhesive resin cements are composed of diacrylate resins with acidic and adhesive groups and glass filler. They are usually dual-cured resins that can be light activated and can self-cure. During setting, self-adhesive resin cements typically undergo a change in pH from acidic (pH 2.1 to 2.3) to less acidic (pH 5.6 to 6.0). The early acidity of the cement allows it to be self-etching. The change with time to a less acidic pH may make the cement more hydrolytically stable, although the clinical implications of the less acidic pH have not been demonstrated as yet.
As a result, self-adhesive resin cements demonstrate the following characteristics:
- May require refrigeration; bring to room temperature before using.
- Self-etching; no phosphoric acid or special primer is needed.
- Dual-cured; can be light- or self-cured.
- Fluoride-releasing.
- Usually available in universal, translucent, and opaque shades.
Properties of Self-adhesive Resin Cements
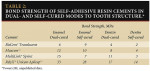
Self-adhesive resin cements bond to tooth structure and other materials with low to medium bond strengths (Table 2). The separate use of a bonding agent is not recommended. Although bonding agents may be compatible with self-adhesive resin cements, their use makes manipulation more complicated and does not dramatically improve bond strength to tooth structure. Higher bond strengths can be obtained with esthetic and adhesive resin cements that are bonded with separate bonding agents or primers.
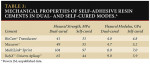
Self-adhesive resin cements generally are not as strong as esthetic and adhesive resin cements. Flexural strength and modulus measured when these cements are light activated are generally higher than when they are self-cured (Table 3).
Self-adhesive resin cements are reported to have values of linear expansion of 0.5% to 1.5% over two months. Use of these cements with all-ceramic restorations is not a concern.
Clinical Observations of Self-adhesive Resin Cements
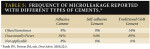
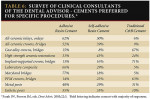
Self-adhesive resin cements have a lower incidence of sensitivity than adhesive or traditional crown and bridge cements (Table 4). Microleakage of self-adhesive resin cements has been reported to be lower than that of traditional cements (Table 5). A recent survey of clinical consultants of The Dental Advisor has shown that self-adhesive resin cements were most commonly selected for cementation of high-strength (ie, zirconia) all-ceramic restorations (Table 6).
In a recent clinical study, one self-adhesive resin cementa was studied over a period of four years. More than 4400 restorations were cemented, and 1560 restorations were observed at recall. The results showed that occasional sensitivity to temperature was less than 1.8%, and microleakage was about 4.2%, with graying noted at the margins. One percent of the restorations required replacement. Retention was excellent, with only 0.7% of the restorations requiring re-cementation. These included 18 ceramic onlays, nine ceramic crowns, and five porcelain-fused-to-metal crowns. Of the 18 ceramic onlays that debonded, 10 had little direct retention; in four of these cases, a portion of the tooth fractured.
In another clinical study, zirconia-based crowns and bridgesb were studied over a period of three years. Sixty-six units were placed in 42 patients in 2003. All restorations were cemented with self-adhesive resin cementa. Fifty-nine units were observed at recall. Eighty percent of the restorations exhibited no signs of microleakage, while 20% had slight graying at the margins.
Other recent clinical studies have compared margin integrity and microleakage of self-adhesive resin cements with esthetic and adhesive resin cements that are bonded with separate bonding agents or primers. In general, the self-adhesive resin cements have performed as well as the esthetic and adhesive resin cements.
Manipulation of Self-adhesive Resin Cements
Self-adhesive resin cements eliminate the etching and priming steps. Most products are paste-paste systems with auto-mix dispensers, but encapsulated products are also available. Manufacturers' recommendations should be followed when bonding self-adhesive resin cements to tooth structure.
Self-adhesive resin cements are generally not recommended for the cementation of porcelain veneers, feldspathic or leucite ceramic restorations, or other all-ceramic restorations contraindicated for cementing procedures. Rather, they are recommended for the cementation of all-ceramic inlays and onlays, cast alloy crowns and bridges, ceramometal crowns and bridges, and high-strength ceramic crowns, bridges, inlays/onlays, and posts (eg, cast metal, ceramic, fiber-reinforced resin).
When manipulating self-adhesive resin cements, it is important to keep the following clinical considerations in mind.
- Don't over dry the tooth; moisten with water if needed.
- Some cementsc,d require a gel barrier for complete setting.
- Use light activation whenever possible. Dual-cured cements typically have increased flexural strength and bond strength when activated with a light vs. self-curing.
- Translucent shades may be sensitive to ambient light.
- Excess cement is easy to remove after several seconds of exposure to the curing light, but hard to clean up if you wait too long.
- Self-adhesive cements are contraindicated where there is insufficient retention.
- Self-adhesive resin cements should NOT be applied directly on exposed pulp or dentin that is close to the pulp.
- Some products provide extension tips for the capsules for post cementation.
- Do not use a lentulo to spin cement into a canal space for post cementation. Place the cement on the post before placing it in the canal.
- Use a silane primer with all-ceramic restorations.
Summary
Self-adhesive resin cements offer improved properties and less technique sensitivity than traditional cements. Therefore, they may be excellent choices for the cementation of appropriate ceramic and alloy-based restorations.
Disclosure
The author is senior vice president of Dental Consultants, Inc., publisher of The Dental Advisor. He is also a member of ADCAA, LLC (Apex Dental Milling), an authorized Lava milling center. Dental Consultants, Inc., has received grant/research support from 3M ESPE, Pentron, GC America, Inc., Kerr, and Ivoclar Vivadent.
References
1. Burke FJ, Fleming GJ, Abbas G, et al. Effectiveness of a self-adhesive resin luting system on fracture resistance of teeth restored with dentin-bonded crowns. Eur J Prosthodont Restor Dent. 2006;14:185-188.
2. Farah JW, Powers JM, eds. Adhesive resin cements. Dent Advis. 2005;22:5.
3. Farah JW, Powers JM, eds. Esthetic resin cements for all-ceramic restorations. Dent Advis. 2005;22:1.
4. Farah JW, Powers JM, eds. Traditional crown and bridge cements. Dent Advis. 2006;23:1.
5. Farah JW, Powers JM, eds. Dental lasers. Dent Advis. 2007;24:8.
6. Farah JW, Powers JM, eds. Composite cores. Dent Advis. 2007;24:8.
7. Federlin M, Krifka S, Herpich M, et al. Partial ceramic crowns: influence of ceramic thickness, preparation design and luting material on fracture resistance and marginal integrity in vitro. Oper Dent. 2007;32:251-260.
8. Frankenberger R, Lohbauer U, Schaible RB, et al. Luting of ceramic inlays in vitro: Marginal quality of self-etch and etch-and-rinse adhesives versus self-etch cements. Dent Mater. 2007;May [Epub ahead of print].
9. Palacios RP, Johnson GH, Phillips KM, et al. Retention of zirconium oxide ceramic crowns with three types of cement. J Prosthet Dent. 2006;96:104-114.
10. Powers JM, O'Keefe KL. Cements: How to select the right one. Dent Prod Rep. 2005;39:76-78.
11. Powers JM, Sakaguchi RL, eds. Craig's Restorative Dental Materials. 12th ed. St. Louis, MO: Mosby Elsevier; 2006.
12. Powers JM, Wataha JC. Dental Materials: Properties and Manipulation. 9th ed. St. Louis, MO: Mosby; 2008.
13. Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: A review of the current literature. J Prosthet Dent. 1998;80: 280-301.
14. Self-adhesive resin cements. CRA Foundation Newsletter. 2007;31(7):1-3.
15. Wang VJ, Chen YM, Yip KH, et al. Effect of two fiber post types and two luting cement systems on regional post retention using the push-out test. Dent Mater. 2007;July [Epub ahead of print].
a RelyX™ Unicem, 3M ESPE, St. Paul, MN
b LAVA™, 3M ESPE, St. Paul, MN
c Embrace™ WetBond™, Pulpdent Corporation, Watertown, MA
d MonoCem™, Shofu Incorporated, San Marcos, CA
About the Author
John M. Powers, PhD
Ann Arbor, Michigan