Using Project Management Principles to Facilitate Interdisciplinary Collaboration
Konstantinos Vazouras, DDS, MPhil, MDSc; Gayathri Shenoy, BDS, DMD, MS; and Irina F. Dragan, DDS, DMD, MS
Abstract
The impact of interdisciplinary collaboration should always be evaluated from the perspectives of different stakeholders, including patients (and their families/caregivers), healthcare providers, third-party insurance providers, researchers, and companies that provide materials/supplies, to name a few. In an educational environment, the healthcare provider team consists of a dental student/resident and a faculty member. The assessment of outcomes for interdisciplinary collaborations can be multilayered from patient care to education and research. The aim of this article is to review the different layers of assessment (ie, patient care, education, and research) and provide an overview of the benefits and limitations of interdisciplinary care. In addition, the authors compare the varied processes involved in the synergistic care of a patient to a project delivery in an agile environment.
The goal of general practitioners and dental specialists is to ultimately achieve successful, reliable, and efficient dental care for their patients. According to the Institute of Medicine (US) Committee on Quality of Health Care in America, "all health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics."1 This, however, is not always an easy task.
To tackle the complexities of oral healthcare problems, solutions often require an interdisciplinary collaboration, one that identifies the values and needs of patients.2,3 This collaborative approach places patient interests at the center of the healthcare delivery model and requires effective communication among clinical team members, patients, and other key stakeholders (eg, insurance companies, corporations). This, in turn, should lead to improved treatment outcomes. Successful interdisciplinary care is by no means an easy process.4 With advancements in science and the recognition of 12 different dental specialties (the latest being orofacial pain),5 there is a need to define a process for assessment and delivery of interdisciplinary care.
Timing of the Interdisciplinary Collaboration
In the past, diagnosis and patient management were not always integrated. Different dental disciplines were either non-existent or practitioners ignored their existence.6 Today, dental treatment has become significantly more sophisticated and, consequently, far more complex. Patient expectations have increased dramatically,7 and this has led to the development of several different disciplines, such as orofacial pain, oral medicine, and dental anesthesiology. Clinicians are often faced with the challenge of differentiating between phased treatment and synchronous treatment, as "timing" is an important factor. Still, unfortunately some practitioners may bypass a team approach and instead rush into procedures that they may feel comfortable with, without evaluating or visualizing the final result.
It is critical for practitioners to identify the patient's chief complaint, expectations, and actual needs while acknowledging the need for referral to a specialist to maximize the quality of care. A single dental practitioner cannot be a "master" in all aspects of modern dentistry; therefore, a careful step-by-step process is necessary to identify and evaluate the best options for each and every patient.
To secure the best possible treatment outcome, effective interdisciplinary coordination among the key stakeholders, general dentist, and dental specialists is essential. The general practitioner plays a pivotal role in collaborating with specialists early in the treatment planning process to achieve the best possible treatment outcome, and he or she should not be undermined. This model can enable successful planning and delivery of treatment while incorporating a carefully designed backup solution if needed. Treatment options should be clearly communicated to and discussed with the patient, who will then be able to make an informed decision on the most predictable and optimal treatment modality. This, in turn, should lead to a desired outcome and, most importantly, a satisfied patient. Interdisciplinary collaboration is crucial to a successful solution and outcome in all healthcare fields, and dentistry is no exception.
Often, the collaboration between general practitioners and dental specialists takes place after a complication has occurred. The risks, benefits, and alternatives of all treatment options should be reviewed in detail before the procedure to avoid such mishaps. Prevention of complications or having an already-set plan in place in case they occur is preferable. The goal should always be to execute an evidence-based treatment plan that supports a favorable long-term prognosis and is well aligned with the patient's actual needs and expectations.8
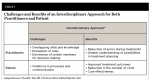
The decision-making process should consist of a careful and well-designed sequence of delivery of a treatment plan with a focus on clear communication with all involved practitioners regarding when and how their intervention will occur. When interdisciplinary care is carefully planned and well coordinated, excellent results can be achieved in a timely and cost-effective manner with maximum benefit for the patient and all key stakeholders; conversely, several challenges are likely to surface when interdisciplinary care is poorly planned (Table 1).2
It is presently widely accepted that the value of an evidence-based practice approach includes the "triangle" of patient's chief complaint, practitioner's clinical experience, and related scientific evidence.9 The contribution of research toward improving the quality of clinical dentistry has been well documented.10 Such research has broadened the scope of treatment options and increased the quality of care for patients. However, most research findings are contributions from individual disciplines.9 A shift in curriculum that is occurring at academic institutions to integrate interdisciplinary clinical education is a testament to the growing focus on interdisciplinary treatment.6 Interdisciplinary research studies can facilitate the collaboration of knowledge from different disciplines to provide scientific and clinical evidence to improve treatment outcomes.11 The results obtained from these studies might encourage providers to seek engagement with colleagues from different disciplines to collaborate on interdisciplinary "evidence-based" treatment plans. For example, findings from appropriate restorative planning prior to surgical implant placement versus surgically driven implant placement could be utilized. This could be particularly important when treatment planning a complex case.
Challenges and Benefits of Synchronous Interdisciplinary Care
The sharing of interdisciplinary expertise can be both challenging and rewarding (Table 1).12 Challenges of an interdisciplinary approach can include conflict of perceptions of team member roles, competition among team members with overlapping skills and knowledge, and the dominance of some team members with regard to decision-making and execution of the treatment plan. To address these challenges, role expectations must be made clear, common goals must be defined, and a flexible, iterative decision-making process must be incorporated. Since the treatment plan is guided by the final restorations, the general dentist or prosthodontist usually is the lead team member, depending on the complexity of the case. Each provider must demonstrate a level of competence as per the demands of the case. This approach is dependent on open, real-time communication among team members and, most importantly, a strong commitment toward functioning as a team to provide optimum patient care and treatment outcomes.
According to Ramaswamy et al, there is sparse evidence of an educational model in postgraduate programs at US dental schools that fosters interdisciplinary dental education.6 However, educational institutions worldwide are adopting a comprehensive treatment planning mentality at an increasing rate, thus helping facilitate a more thorough approach to dental care.13 In addition, traditional family dental practices used to provide all dental care to their patients, thus patients did not typically perceive the need for interdisciplinary care, nor did overconfident dental practitioners who often saw referrals to dental specialists as a potential threat to their own practice cultivate such a perception.
According to the American Dental Association Health Policy Institute, recent graduates and academic institutions should consider two trends for dentistry going forward: "adopt the value agenda" and "collaborate much more."14 Patients are becoming increasingly aware of the different dental disciplines that may be able to provide them with a higher level of care. An increased number of dental specialists, even in rural areas where access has traditionally been limited, has significantly contributed to greater awareness and accessibility. This combined with the mentality of a newer generation of dental graduates, who are generally more receptive to an interdisciplinary approach, is leading toward the redefining of the role of the general dentist. This role can be of dual nature and similar to that of a primary care provider who coordinates a comprehensive dental treatment among various specialties. This dual approach-practitioner and coordinator-encourages and facilitates collaboration with different dental specialists as needed, with the ultimate goal of achieving optimal oral health for patients while also meeting their treatment goals.
Pathways to Integrating Interdisciplinary Treatment Planning
Following a structured sequence for integrating interdisciplinary planning as a treatment approach can be helpful to coordinate the team.15 The steps in the interdisciplinary approach proposed are: (1) assessment, (2) planning, (3) implementation, and (4) evaluation.
Assessment of the case entails diagnosis and an understanding of the involved disciplines that will be brought on board as per the case requirements and treatment goals. The initial assessment can be framed using fundamentals of project management, the discipline that addresses delivery of unique solutions under the constraints of complexity and interdisciplinarity (Table 2).
Synchronous treatment planning is needed along with a defined timeline, with the roles and expectations defined for each provider. At this point, the final treatment plan and treatment sequence should also be visualized. In addition to an ideal treatment plan, an alternative treatment plan should also be presented to the patient. The risks and benefits of each treatment option, as well as any alternatives and the commitment required for each option, must be clearly explained to the patient prior to beginning treatment.
Implementation of the case involves performing the treatment as per the treatment plan and maintaining effective (clear and real-time) communication among providers during the process, in case changes occur.
A continuous evaluation of the performed treatment is done at the completion of treatment and during follow-up care. This step is essential for outlining the success and challenges encountered during each step of treatment, thereby improving the interdisciplinary team's approach for future cases.
The following case example demonstrates the application of this approach, highlighting the change in the patient's overall smile. The outcome was well received by both the practitioners involved in the care and the patient.
Case Synopsis
A 43-year-old African American man presented with the chief complaint of needing "help with my teeth." He indicated that his maxillary teeth were his top priority, while the mandibular teeth "can wait." The patient was highly cooperative and was interested in a fixed restorative option. He had been involved in a bicycle accident more than 20 years ago and lost some of his maxillary teeth (teeth Nos. 5 through 8). The edentulous areas had been restored with a fixed partial denture (FPD) 7 years before the initial presentation. The FPD was now loose and came off repeatedly. Clinical findings are shown in Figure 1 (top row); radiographic and periodontal findings are presented in Figure 2 through Figure 5.
Using evidence-based practices, the interdisciplinary team assessed the complexities of the case, compiled a comprehensive treatment plan, and delivered care. Among the findings was that the patient presented with restored and unrestored partial edentulism in both arches. Failing restorations were noticed, especially on the maxillary arch. The radiographic examination revealed existing root canal therapies (teeth Nos. 2, 14, 15, and 29). Teeth Nos. 9 and 10 had well-defined, non-corticated periapical radiolucencies. The periodontal condition was diagnosed as localized slight chronic periodontitis.
The patient was, thus, presented with various treatment options and preferred a fixed option that involved multiple phases. After medical clearance was obtained and oral hygiene instructions were given, the patient underwent a synergistic periodontal, restorative, endodontic, and orthodontic therapy, as presented in Figure 1. The disciplines involved in this collaborative care included prosthodontics, periodontology, endodontics, orthodontics, oral-maxillofacial radiology, and oral-maxillofacial pathology. The duration of the treatment was 5 years, and some changes to the initial treatment plan occurred over time. During the surgical therapy, a guided bone regeneration procedure for the maxillary right quadrant was performed. Initially two fixed prostheses supported by implants were planned: No. 3-x-No. 5 and No. 6-x-No. 8. Considering the ridge remodeling during the ridge augmentation and to allow for adequate mesiodistal space between the adjacent implants, the final prosthesis in that area was No. 3-x-No. 6 (No. 5)-x-No. 8. This reduced the number of implants used in the area from four to three, as presented in Figure 1. Other changes incorporated in the treatment plan can be reviewed in Figure 1.
Applying an interdisciplinary approach from the early stages of the case allowed the team of clinicians to share their knowledge and accommodate changes during the treatment using a structured framework with integrated goals. A comparison of the initial clinical situation versus the treatment rendered is shown in Figure 6 (pretreatment) and Figure 7 (post-treatment). The final treatment rendered included endodontic therapy for teeth Nos. 2, 14, and 15; orthodontic therapy to correct space management on the mandibular arch; fixed implant-supported restorations (No. 3-x-No. 6 [No. 5]-x-No. 8; No. 9-x; No. 18-No. 19; No. 30); and periodontal maintenance recare every 3 months.
Conclusion
Solutions to complex oral healthcare problems often require interdisciplinary collaboration, with the general practitioner playing a pivotal role in coordinating communication among specialists early in the treatment planning process and throughout the case. The general steps of an interdisciplinary approach include assessment, planning, implementation, and evaluation. When evaluating an interdisciplinary approach, it is essential to review how each discipline contributed to the treatment. By working together, clinicians in various disciplines can expand their clinical knowledge and utilize the experience they gain from a given case to facilitate the care of other patients with similar clinical complexities.
ACKNOWLEDGMENT
The authors would like to acknowledge all the faculty, residents, and administrators that were part of the Complex Cases program developed at Tufts University School of Dental Medicine. In particular, they would like to acknowledge some of the residents and faculty that were involved in this clinical case: Drs. Harp, Shiromoto, Alssafar, Huang, Kai, Seetner, El Rafie, Kanavakis, and Amato.
ABOUT THE AUTHORS
Konstantinos Vazouras, DDS, MPhil, MDSc
Assistant Professor and Program Director, Post-Graduate Prosthodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Fellow, American College of Physicians
Gayathri Shenoy, BDS, DMD, MS
Private Practice limited to Periodontology and Implant Dentistry, Tuscaloosa, Alabama
Irina F. Dragan, DDS, DMD, MS
Adjunct Associate Professor and Former Director of Faculty Education and Instructional Development, Tufts University School of Dental Medicine, Boston, Massachusetts; Private Practice limited to Periodontology and Implant Dentistry, Brookline, Massachusetts
References
1. Greiner AC, Knebel E, eds. Health Professions Education: A Bridge to Quality. Washington, DC: Institute of Medicine, The National Academies Press; 2003.
2. Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29(6):351-364.
3. Valachovic RW. Integrating oral and overall health care: building a foundation for interprofessional education and collaborative practice. J Dent Educ. 2019;83(2 suppl):S19-S22.
4. Walji MF, Karimbux NY, Spielman AI. Person-centered care: opportunities and challenges for academic dental institutions and programs. J Dent Educ. 2017;81(11):1265-1272.
5. Heir GM. Orofacial pain, the 12th specialty: the necessity. J Am Dent Assoc. 2020;151(7):469-471.
6. Ramaswamy V, Karimbux N, Dragan IF, et al. The status of interdisciplinary education in advanced education programs at U.S. dental schools. J Dent Educ. 2018;82(11):1213-1219.
7. Colvin J, Dawson DV, Gu H, Marchini L. Patient expectation and satisfaction with different prosthetic treatment modalities. J Prosthodont. 2019;28(3):264-270.
8. Ni Riordain R, Glick M, Al Mashhadani SSA, et al. Developing a standard set of patient-centred outcomes for adult oral health - an international, cross-disciplinary consensus. Int Dent J. 2020. doi: 10.1111/idj.12604.
9. Shaikh S, Dragan IF, Nevius A, et al. Using evidence-based dentistry in the clinical management of combined periodontal conditions. J Evid Based Dent Pract. 2018;18(4):290-297.
10. Shenoy GM, Dragan IF, Pagni S, et al. Factors associated with evidence-based clinical questions presented in a vertically integrated seminar series at a U.S. dental school. J Dent Educ. 2018;82(6):625-629.
11. Ramesh A, Ganguly R, Qualters DM. An interdisciplinary, team-based design for an oral and maxillofacial radiology course for postdoctoral dental students. J Dent Educ. 2014;78(9):1339-1345.
12. Abramson JS, Mizrahi T. When social workers and physicians collaborate: positive and negative interdisciplinary experiences. Soc Work. 1996;41(3):270-281.
13. Wolcott MD, Quinonez RB, Tittemore AJ, et al. Developing a curriculum blueprint and taxonomy: process, progress, and pivots. J Dent Educ. 2020;84(12):1368-1377.
14. Yarbrough C, Vujicic M. Oral health trends for older Americans. J Am Dent Assoc. 2019;150(8):714-716.
15. Rosen EB, Donoff RB, Riedy CA. U.S. dental school deans' views on the value of patient-reported outcome measures in dentistry. J Dent Educ. 2016;80(6):721-725.