Material Selection for Single-Unit Crown Anterior Restorations
Hernán Lázaro Villa, CDT, MDC; Nathaniel C. Lawson, DMD, PhD; and Marco Brindis, DDS
Abstract: Lithium disilicate and layered zirconia appear to be the most prevalent materials used for single-unit anterior crowns. These materials offer the necessary mechanical properties as well as sufficient optical characteristics needed in this type of restoration. There now are also more translucent versions of zirconia available that can be used for monolithic anterior restorations. This article discusses the factors that clinicians must take into account when determining a restorative material for single-unit anterior crowns. Considerations for lithium-disilicate crowns, 4 and 5 mol% yttria-containing (4Y and 5Y) zirconia materials, and layered 3Y zirconia restorations are provided.
A restorative material for a single anterior crown must have not only sufficient mechanical properties to allow function but also the optical properties to blend with the existing dentition. Based on a 2016 survey, the most commonly selected materials for single-unit anterior crowns were lithium disilicate and layered zirconia.1 The survey did not specify if the lithium-disilicate crowns were layered or monolithic. One aspect of the survey that may not reflect more recent developments is the lack of information about translucent 4 and 5 mol% yttria-containing (4Y and 5Y) zirconia. At the time the survey was administered in 2015, 4Y and 5Y zirconia were not as prevalent as they are today, as the commercially available brands had just been released.
Taking these factors into consideration, this article proposes a simple method for selecting a material for single-unit anterior crowns in which lithium disilicate would remain the default choice, with other material options used for certain clinical indications. Advantages of using a 4Y or 5Y zirconia is that it is less likely to fracture in try-in and has the versatility to be cemented with various types of cements, not just bonded. Layered 3Y zirconia may be indicated for clinical cases in which a dark-colored preparation needs to be blocked or if there is insufficient interocclusal space to meet the minimum requirement for lithium disilicate. This article will describe these materials and clinical scenarios in further detail. It will deal, however, only with the replacement of a single unit. Other considerations may need to be taken into account when restoring multiple units in the anterior or anterior fixed partial dentures.
Considerations for Lithium-Disilicate Crowns
As reported in the aforementioned 2016 survey, lithium disilicate is currently the most commonly used material for single-unit anterior crowns.1 Lithium disilicate was introduced to dentistry with IPS e.max® Press in 2005 and IPS e.max® CAD in 2006 (Ivoclar Vivadent, ivoclarvivadent.com).2 The difference between the two materials is that the former is fabricated when pre-crystallized ingots are heat-pressed into a stone investment, and the CAD version is fabricated when partially crystallized blocks are carved into their final shape in a milling machine and then fully crystallized in a furnace. Many dentists are interested in knowing which of the two fabrication techniques leads to a superior crown. Laboratory research studies have reported that both fabrication techniques are capable of producing clinically acceptable marginal gaps smaller than 140 µm (with most studies reporting between 35 µm and 120 µm).3,4 Of the studies that have compared both fabrication techniques side by side, there is no consensus on which technique produces smaller marginal gaps. Three studies found slightly smaller marginal gaps with heat-pressing, and two studies found slightly smaller marginal gaps with milling.3,4 In the authors' experience, however, pressed lithium-disilicate restorations more reliably produce closed margins. Regarding strength, there is no apparent difference for the materials used for either fabrication technique. One laboratory study reported no difference in the strength of IPS e.max Press and IPS e.max CAD,5 whereas another laboratory study reported a 7% higher strength for the press technique than the CAD.6
These materials are also offered in various translucencies (ie, HT [high translucency], MT [medium translucency], LT [low translucency], MO [medium opacity], HO [high opacity]). The translucency of the material does not seem to be altered by varying crystal composition or density, except for e.max CAD MO, which is produced with higher density of smaller crystals.6 Therefore, all translucencies of lithium disilicate offer a similar strength, other than e.max CAD MO, which is about 17% weaker than the others.5,6
Since the introduction of lithium-disilicate materials in 2005, several other materials with similar compositions have been released to the dental market. This category of ceramic has recently been termed the "lithium-X-silicates" to refer to lithium disilicates (eg, IPS e.max; Initial® LiSi Press, GC America, gcamerica.com; Amber® Press, HASS Bio America, hassbio.com), lithium silicates (eg, Celtra® Press, Dentsply Sirona, dentsplysirona.com; Celtra® Duo, Dentsply Sirona; Suprinity®, VITA North America, vitanorthamerica.com), and a lithium aluminosilicate (eg, Nice®, Straumann, straumann.com).7 Some lithium-silicate materials have been marketed as zirconia-reinforced lithium silicates, however this term is misleading because the zirconia is dissolved within the glass matrix and does not reinforce the ceramic.7 The flexural strength of several of the lithium-X-silicate materials (Amber® Mill, HASS Bio America; Celtra Press; Initial LiSi Press; Livento® Press, Medtech, cmsa.ch/en/medtech) was recently reported to be similar to that of e.max Press.8 Changing the crystalline composition of lithium-X-silicate materials to equigranularity crystals (eg, Celtra Press), however, has a negative effect on fracture toughness.9
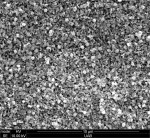
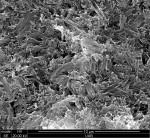
The lithium-silicate materials (Figure 1, Celtra Duo) have smaller crystals than lithium-disilicate materials (Figure 2, IPS e.max CAD), which affects their optical properties.10 Recent studies have reported that Celtra Duo is more translucent than e.max CAD and that Suprinity is less translucent than e.max CAD but has more opalescence.11,12 One of the present authors (HLV) has also noted a natural-looking opalescence of a lithium silicate (Celtra Press) (Figure 3). These optical differences between the lithium-silicate and lithium-disilicate materials do not imply that one is better than the other. However, clinicians should not expect these materials to have interchangeable optical properties.
Lithium disilicate is translucent enough that it may be commonly used as a monolithic material. In the authors' experience, however, a cut-back on the facial surface and/or incisal edge with a layer of porcelain is often needed to obtain the characterization necessary for single anterior crowns (Figure 4). A laboratory trial reported that a 2-mm thick lithium-disilicate crown with a 0.7 mm cut-back demonstrated a 33% reduction in strength when loaded on the area of cut-back.13 The location of the cut-back, therefore, should be discussed with the laboratory.
Considerations for 4Y/5Y Zirconia Materials
As previously mentioned, there are now more translucent versions of zirconia available that can be used for monolithic anterior restorations. The increased translucency of zirconia is achieved by increasing the ratio of cubic to tetragonal phase within the zirconia. Cubic zirconia is more translucent than tetragonal zirconia because the arrangement of atoms in the cubic phase is optically isotropic, or symmetrical. This means that light can pass through in many different directions without being stopped or redirected. The amount of cubic zirconia within a zirconia is determined by the amount of yttria stabilizer with the zirconia. At 3 mol% yttria (3Y), there is between 10% to 15% cubic phase; at 4 mol% yttria (4Y), there is between 25% to 37% cubic phase; and at 5 mol% yttria (5Y), there is between 50% to 58% cubic phase.14,15 As a result, 4Y zirconia is 13% more translucent than 3Y, and 5Y is 33% more translucent than 3Y. 5Y zirconia, however, is still less translucent than lithium disilicate.14 Although translucency is desirable to mimic natural enamel, different clinical situations will require varying degrees of translucency/opacity.
The increased translucency achieved from swapping tetragonal zirconia for cubic zirconia comes with a tradeoff in mechanical properties. Tetragonal zirconia is capable of undergoing transformation toughening, the ability to stop the growth of a crack within a material. 3Y zirconia is capable of transformation toughening. 4Y zirconia undergoes some transformation toughening. 5Y zirconia does not transformation-toughen.14 As a result, the strength and fracture toughness decrease from 3Y zirconia to 4Y zirconia to 5Y zirconia. However, 5Y still has a higher strength and fracture toughness than lithium disilicate.16 There is still limited independent verification of how much yttria stabilizer and cubic content is contained in commercial brands of zirconia. A recent publication reported examples of 3Y zirconia (Lava™ Plus, 3M Oral Care, 3m.com; Cercon® HT, Dentsply Sirona; BruxZir®, Glidewell, glidewelldental.com), 4Y (IPS e.max ZirCAD MT, Ivoclar Vivadent; Katana™ STML, Kuraray Noritake, kuraray.com; Zenostar® MT, Wieland Dental, zenostar.de), and 5Y (Lava™ Esthetic, 3M Oral Care; Cercon® XT, Dentsply Sirona; BruxZir® Anterior, Glidewell; Katana™ UTML, Kuraray Noritake).15
Some clinical situations exist in which 4Y or 5Y zirconia offers clinical advantages over lithium disilicate. First, 4Y or 5Y zirconia may be an option for clinicians who desire to cement their crowns without bonding, particularly if the thickness of the crown is below the minimum recommended thickness for conventional cementation of lithium disilicate. This recommendation is based on a recent study which reported that although the strength of 5Y zirconia and lithium-disilicate crowns (with 0.8 mm to 1 mm thickness) were equivalent if the crowns were bonded with a resin cement, if the crowns were cemented with resin-modified glass-ionomer cements, 5Y zirconia outperformed lithium disilicate.17 This suggestion should only be followed in the absence of the zirconia manufacturer's recommendations, which the clinician should always adhere to. The strength of the crown material also makes these materials more user-friendly prior to bonding, because their strength is not as dependent on bonding to tooth structure as lithium-disilicate materials are. This strength is particularly advantageous to prevent fracturing a ceramic restoration during the process of trying it in.17
Second, 4Y zirconia may offer strength advantages when the length of a restoration exceeds the limit for which bonding to the tooth reinforces the material. Figure 5 and Figure 6 show 4Y zirconia anterior crowns, which were selected to reduce the likelihood of cohesive fracture of the long incisal edges.
In the authors' experience, most 4Y and 5Y crowns have been manufactured as monolithic restorations. Therefore, all characterization must come either from within the crown (multilayer disks or dip stains) or from external staining of the crown (Figure 7). A recent study examined the effects of toothbrushing on the retention of external stains applied to monolithic lithium disilicate, 5Y zirconia, and 3Y zirconia. In the study, visually perceptible changes in the stain were observed on 5Y and 3Y zirconia after 1 year of simulated toothbrushing with a traditional toothpaste (relative dentin abrasion [RDA] 72). No visually perceptible changes in the stain were noted on lithium disilicate, even after 5 years of simulated brushing.18 These findings suggest that internal coloring of zirconia through dip stains and/or multilayer blocks may help ensure that these restorations maintain their ability to blend with surrounding teeth.
Considerations for a Layered 3Y Zirconia Restoration
When selecting a layered 3Y zirconia restoration, the zirconia core should provide strength and blocking ability and the veneering layer should offer translucency and esthetics. Layered 3Y zirconia restorations can attain a high level of esthetics due to the 3-dimensional color and translucency characterization that may be achieved by layering different shades and translucency of porcelain (Figure 8). The disadvantage of using any layered restoration (eg, layered 3Y zirconia and porcelain fused to metal) is an increased risk of delamination as the interface between the veneer and the zirconia core becomes the weakest link.
For example, a laboratory study comparing the chipping rates of monolithic lithium-disilicate crowns to layered zirconia crowns showed that all layered specimens experienced veneer chipping during the fatigue process while no chipping of monolithic lithium disilicate occurred.19 Therefore, clinicians must be cognizant of the coping design of a layered anterior crown to prevent excessive force being placed on the porcelain layer. This may be achieved by designing a zirconia coping in which all functional movements of the opposing teeth are located on the coping (Figure 9 and Figure 10).
Different methods of preventing fracture of the porcelain on layered zirconia crowns have been employed. Initially, the incidence of porcelain fracture was addressed by modifying the coefficient of thermal expansion of the layering porcelain to match that of zirconia20 and then "slow cooling" the layered restoration upon removal from the furnace.21 Different methods of porcelain fabrication, such as hand-layered, milled, and pressed, have been compared with no consistently reported improvements in strength.19
A clinical situation in which a layered zirconia crown can be indicated is when there is limited interocclusal restorative space for maxillary anterior crowns (Figure 11). In such a case, the lingual surface of the crown can be fabricated from monolithic zirconia to take advantage of the reduced restorative thickness required (which may be as little as 0.6 mm for 3Y zirconia). In fact, all layered zirconia maxillary incisor crowns should be designed with monolithic zirconia on their lingual surfaces because the wear of enamel opposing polished zirconia has been reported to be approximately 10 times less than that of porcelain.22 Aside from low antagonist enamel wear, zirconia (3Y, 4Y, and 5Y) does not undergo any material wear.23 There is some concern that lack of wear of zirconia restorations relative to other teeth in the mouth may cause occlusal trauma.
Other clinical situations in which a layered restoration may be indicated instead of a monolithic restoration is when the tooth preparation is discolored, a metal post and core is present, or a metal-based implant abutment is being restored. In these cases, it is advantageous for the crown material to mask the underlying tooth preparation or abutment (Figure 12 through Figure 14).
3Y zirconia copings are the most effective material to use to block out discolored substructures. Alternatively, opaque versions of some lithium-disilicate materials, such as IPS e.max HO, can also block dark substructures. However, a laboratory study reported that 3Y zirconia was more opaque than e.max HO and generally worked better to mask dark backgrounds. This is particularly important for silver-colored substructures (such as titanium abutments), which are more difficult to block than copper-colored or dark VITA shade substructures.24 Monolithic 5Y zirconia or e.max HT at equivalent thickness were not able to block out dark backgrounds.24 An opaque cement was also helpful for blocking an underlying discoloration, however not to the extent that could be achieved by proper material selection. Therefore, layered 3Y zirconia would be the material of choice for difficult blocking cases.
Summary
Monolithic restorations may be fabricated from lithium X-silicates; thus far, there is insufficient evidence to differentiate brand formulations. The advantage of using a 4Y or 5Y zirconia is that it is less likely to fracture in try-in, which may be an issue with lithium disilicate depending on the skill level and experience of the clinician, and has the versatility to be cemented with various types of cements, not just bonded. Layered 3Y zirconia restorations are the most effective among ceramic materials for blocking discolored tooth preparations or metal abutments. Additionally, layered zirconia restorations are useful when interocclusal space is limited. The framework should be designed without lingual veneering porcelain to utilize the strength of the zirconia and reduce the wear of opposing enamel.
About the Authors
Hernán Lázaro Villa, CDT, MDC
Former Director, Master Dental Ceramist Program, Department of Clinical and Community Sciences, University of Alabama at Birmingham School of Dentistry, Birmingham, Alabama
Marco Brindis, DDS
Assistant Professor of Dentistry, Department of Prosthodontics, Louisiana State University Health Sciences Center School of Dentistry, New Orleans, Louisiana
Nathaniel C. Lawson, DMD, PhD
Associate Professor and Division Director of Biomaterials, Department of Clinical and Community Sciences, University of Alabama at Birmingham School of Dentistry, Birmingham, Alabama
References
1. Makhija SK, Lawson NC, Gilbert GH, et al. Dentist material selection for single-unit crowns: findings from the National Dental Practice-Based Research Network. J Dent. 2016;55:40-47.
2. Willard A, Gabriel Chu TM. The science and application of IPS e.Max dental ceramic. Kaohsiung J Med Sci. 2018;34(4):238-242.
3. Papadiochou S, Pissiotis AL. Marginal adaptation and CAD-CAM technology: a systematic review of restorative material and fabrication techniques. J Prosthet Dent. 2018;119(4):545-551.
4. Mounajjed R, Layton DM, Azar B. The marginal fit of E.max Press and E.max CAD lithium disilicate restorations: a critical review. Dent Mater J. 2016;35(6):835-844.
5. Wang F, Yu T, Chen J. Biaxial flexural strength and translucent characteristics of dental lithium disilicate glass ceramics with different translucencies. J Prosthodont Res. 2020;64(1):71-77.
6. Fabian Fonzar R, Carrabba M, Sedda M, et al. Flexural resistance of heat-pressed and CAD-CAM lithium disilicate with different translucencies. Dent Mater. 2017;33(1):63-70.
7. Belli R, Wendler M, de Ligny D, et al. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent Mater. 2017;33(1):84-98.
8. Stawarczyk B, Dinse L, Eichberger M, et al. Flexural strength, fracture toughness, three-body wear, and Martens parameters of pressable lithium-X-silicate ceramics. Dent Mater. 2020;36(3):420-430.
9. Hallmann L, Ulmer P, Gerngross MD, et al. Properties of hot-pressed lithium silicate glass-ceramics. Dent Mater. 2019;35(5):713-729.
10. Awad D, Stawarczyk B, Liebermann A, Ilie N. Translucency of esthetic dental restorative CAD/CAM materials and composite resins with respect to thickness and surface roughness. J Prosthet Dent. 2015;113(6):534-540.
11. Arif R, Yilmaz B, Johnston WM. In vitro color stainability and relative translucency of CAD-CAM restorative materials used for laminate veneers and complete crowns. J Prosthet Dent. 2019;122(2):160-166.
12. Kurt M, Bankoğlu Güngör M, Karakoca Nemli S, Turhan Bal B. Effects of glazing methods on the optical and surface properties of silicate ceramics. J Prosthodont Res. 2020;64(2):202-209.
13. Zhao K, Wei YR, Pan Y, et al. Influence of veneer and cyclic loading on failure behavior of lithium disilicate glass-ceramic molar crowns. Dent Mater. 2014;30(2):164-171.
14. Zhang F, Reveron H, Spies BC, et al. Trade-off between fracture resistance and translucency of zirconia and lithium-disilicate glass ceramics for monolithic restorations. Acta Biomater. 2019;91:24-34.
15. Zhang Y, Lawn BR. Novel zirconia materials in dentistry. J Dent Res. 2018;97(2):140-147.
16. Nassary Zadeh P, Lümkemann N, Sener B, et al. Flexural strength, fracture toughness, and translucency of cubic/tetragonal zirconia materials. J Prosthet Dent. 2018;120(6):948-954.
17. Lawson NC, Jurado CA, Huang CT, et al. Effect of surface treatment and cement on fracture load of traditional zirconia (3Y), translucent zirconia (5Y), and lithium disilicate crowns. J Prosthodont. 2019;28(6):659-665.
18. Sulaiman TA, Camino RN, Cook R, et al. Time-lasting ceramic stains and glaze: a toothbrush simulation study. J Esthet Restor Dent. 2020;32(6):581-585.
19. Alsarani M, De Souza G, Rizkalla A, El-Mowafy O. Influence of crown design and material on chipping-resistance of all-ceramic molar crowns: an in vitro study. Dent Med Probl. 2018;55(1):35-42.
20. Fischer J, Stawarzcyk B, Trottmann A, Hämmerle CH. Impact of thermal misfit on shear strength of veneering ceramic/zirconia composites. Dent Mater. 2009;25(4):419-423.
21. Tan JP, Sederstrom D, Polansky JR, et al. The use of slow heating and slow cooling regimens to strengthen porcelain fused to zirconia. J Prosthet Dent. 2012;107(3):163-169.
22. Janyavula S, Lawson N, Cakir D, et al. The wear of polished and glazed zirconia against enamel [published correction appears in J Prosthet Dent. 2015;114(1):159. Lawson, Nathaniel (corrected to Lawson, Nathaniel C)]. J Prosthet Dent. 2013;109(1):22-29.
23. Kwon SJ, Lawson NC, McLaren EE, et al. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018;120(1):132-137.
24. Bacchi A, Boccardi S, Alessandretti R, Pereira GKR. Substrate masking ability of bilayer and monolithic ceramics used for complete crowns and the effect of association with an opaque resin-based luting agent. J Prosthodont Res. 2019;63(3):321-326.