Simplifying the Impression-Taking Process for High-Quality Results
Jennifer Bell, DDS
Abstract: When patients present with erosive tooth wear, which may be caused by such common conditions as gastroesophageal reflux disease, the erosion process must be properly identified and diagnosed before proceeding with a smile design change. In the present case, altered passive eruption of the patient's maxillary anterior teeth was diagnosed as a secondary condition to tooth erosion resulting from a long-standing reflux condition. A three-phase treatment plan included improved management of the patient's reflux symptoms by working with her primary care physician, orthodontics, and full-coverage restorations. A key component of the zirconia-based treatment was the use of an intraoral scanner for digital impressions, which allowed for clear marginal visualization, time efficiency, and a simplified impression process.
A patient at the author's practice had been concerned for years with how much shorter her teeth appeared than when she was younger. The Caucasian woman had presented at age 57 with a history of acid reflux and bulimia, although the latter had been under control for some time. She wanted a "quick fix" to her chief complaint. She thought her length could be restored by simply adding bonding to the edges of her teeth, and believed that the reflux had affected only the incisal edges.
This type of thinking is not surprising, as patients often do not notice the subtle changes that occur over time, like altered passive eruption, buccal collapse, and premature contacts. Patients often can only appreciate that something looks different and is unattractive to them, and in their mind the solution should be relatively quick and easy.
Gastric reflux, whether voluntary or involuntary, can be very destructive to tooth structure. During an intraoral examination, several factors can suggest to the clinician an active or past presence of gastroesophageal reflux disease (GERD). Much like most extrinsic cases of erosive wear (from GERD or bulimia) the wear presents as smooth lingual surfaces of the maxillary anterior teeth and flattened occlusal surfaces of mandibular posterior molars.1 This erosive wear evolves over time and destroys the enamel except along the gingival margin, giving the teeth a darker hue.2 As the lingual surfaces of the maxillary teeth begin to erode, the teeth often respond by undergoing altered passive eruption.3
This process needs to be identified and diagnosed appropriately when proceeding with a smile design change to achieve an ideal cosmetic result. In this patient's case, altered passive eruption of the maxillary anterior teeth was diagnosed as a secondary condition resulting from the long-standing reflux condition.
Three-Phase Treatment Plan
After several years and many consultations, the patient finally agreed to move forward with the recommended treatment. The patient's pretreatment condition is depicted in Figure 1 through Figure 3. A thorough smile design work-up was completed using numerous intraoral and extraoral radiographs and photographs. Then, a treatment plan was developed that would address incisal edge position, which had shortened over time, and the appearance of gingiva versus tooth structure during a full smile.4 In addition, the photographs were used to evaluate the curvature of her smile, the midline of the teeth to the face, and the overall esthetics of the smile.
The treatment plan was then constructed to be in three phases. The first phase was to improve management of the patient's reflux symptoms working through her primary care physician. The second and third phases would be dentally driven changes through orthodontics and full-coverage restorations, respectively.
Working with a local orthodontist, the author's team proceeded with clear aligner therapy to level and align the occlusion and intrude the maxillary anterior teeth back to their original gingival position. Aligner therapy proved to be highly challenging because the patient maintained poor compliance. After 18 months of orthodontics, there was minimal improvement in tooth position (Figure 4 and Figure 5). It was evident that during treatment the patient rarely wore her aligners for as much as 12 hours a day.
The patient was interested in changing her overall tooth shade before new restorations were fabricated. In the author's practice, if patients desire a shade change, a bleaching protocol typically is completed prior to their preparation visit. In this case, after completing 2 weeks of an at-home bleaching regimen (Kör Home 16% carbamide peroxide, Kör Whitening, korwhitening.com), the patient was ready to proceed with anterior restorations. Shade matching can be completed at the preparation visit, as shade regression from at-home bleaching is not shown to be statistically significant when done within 6 months of completion.5 Full-coverage porcelain restorations were chosen over veneers because priority was placed on protecting the lingual surfaces of the teeth from further erosion.6 While the patient's reflux condition was being supervised by a medical physician, there was residual concern that more damage would occur since the reflux continued to be moderately present.
Zirconia Restorations
Preparation of the teeth was completed to allow for monolithic zirconia-oxide restorations. Tissue retraction was managed with two cords (size 1), which were placed as atraumtically as possible. The decision was then made to impress the case using an intraoral scanner (iTero® Element 2, Align Technology, Inc., itero.com). Digital impressions were chosen because they offer clear marginal visualization, time efficiency, and patient comfort.7
Scans of the preparations, opposing arch, and buccal bite were completed. The STL file of the impressions was immediately sent to the laboratory along with a prescription for the restorations. Additionally, the clinical photographs were sent to the laboratory via email to aid in the customization of the final product.
Because the patient was not as compliant as needed during the orthodontic phase of treatment, the amount of clinical overjet that was desired was not achieved (Figure 6 and Figure 7). As a compromise to meet this challenge, the author had to limit the choice of materials for the final restorations. A monolithic zirconia base was selected because of several physical characteristics that made it a well-suited material for this case. First, its high flexural strength at less thickness compared to other ceramic options would allow the restoration to be able to withstand the limited overjet created from the orthodontic treatment without catastrophic failure.8 Monolithic zirconia oxide also is a superior material for minimizing wear on opposing teeth, which was desirable in this case, as other biochemical issues were already creating a caustic environment for the patient's enamel integrity.9 Moreover, monolithic zirconia-oxide restorations require less preparation of the teeth, which allows the clinician to maintain a greater amount of pulpal integrity of the teeth. On the other hand, the laboratory opted to add a layer of pressed porcelain on the zirconia-oxide cores to improve the overall esthetics of the case. Layered zirconia restorations are more susceptible to fracture and chipping over time.8
Based on the clinical photographs emailed to the laboratory, the master ceramist determined that a pressed porcelain veneer on the zirconia core would provide the customization of shade required to match the patient's existing dentition. The final restorations were made of zirconium dioxide (DD Bio ZX2, Dental Direkt, dentaldirekt.de) with a feldspar veneering ceramic (VITA VM® 9, VITA, vita-zahnfabrik.com), shade 1M1, as the pressed layer on porcelain on the facials. The restorations had pressed porcelain only from above the incisal edge to the gingival margin. Monolithic zirconia oxide was used for the lingual and incisal edges of the restorations in an effort to prevent chipping.
Delivery and Final Outcome
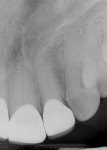
The restorations were delivered a few weeks later. Prior to cementation, marginal integrity of the restorations was reviewed. The author's protocol for approval of restorations for final delivery includes tactile and radiographic evaluation of the margins (Figure 8 and Figure 9). Once the restorations are approved for marginal integrity, occlusion, contacts, and esthetics, the process of isolation and cementation is begun. In this case, it was decided to cement the restorations with resin-modified glass-ionomer cement (RMGIC) (GC FujiCEM® Evolve, GC America, gcamerica.com). The long-term stability of using RMGIC to cement zirconia-oxide restorations, especially for preparations of teeth demonstrating an adequate resistance and retention form, has been shown to be effective in preventing premature loss of restoration and microleakage.10
The final outcome of the case met the patient's primary concerns, achieving the lengthening and lightening of the anterior teeth that she desired (Figure 10). As a clinician, the author noted several areas in the patient's overall smile where a more ideal result could have been achieved. However, because of the patient's continued challenges with GERD, she reported having difficulty with compliance related to clear aligner therapy and whitening protocols. Nonetheless, the patient was pleased with her new smile and the clinician was satisfied with the clinical results of the final restorations.
Digital Impressions
Digital impressions are an effective alternative to conventional impression techniques and may be considered as the first option for impression-taking because of predictable, efficient, and simplified processes for both patients and clinicians.11 Using an intraoral scanner, such as the iTero Element 2 used in this case, affords the clinician many efficiencies that cannot be achieved with traditional polyvinyl siloxane (PVS) impression materials. Preparations can be reviewed and verified, including marginal clarity and restorative clearance, while the patient is still in the office. With a digital platform such as MyiTero (Align Technology, Inc.) clinicians can quickly assess the quality of their preparations, marginal design, marginal visualization, and clearance between arches, as shown in Figure 11 and Figure 12, which are additional digital images of the preparations in this case. If any areas require modification, the clinician can complete those steps and rescan the areas as needed without having to reappoint the patient.
When using PVS impression techniques, clinicians are limited in their ability to assess an ideal impression, marginal integrity, and interarch clearance. Clinicians often will temporize the patient and hope the information captured in PVS, as well as the quality of their preparations, meets the clinical standards to fabricate an ideal restoration. With digital impressions clinicians can avoid unwanted phone calls from the lab requesting more clearance or a better impression of the margin. Digital impressions allow clinicians to be confident that their crown deliveries will be completed with high success rates. By developing a proper smile design treatment plan and executing each phase of treatment completely, practitioners can achieve a high-quality result despite a patient's overall lack of compliance with treatment.
Acknowledgment
The author would like to acknowledge Precision Esthetics Dental Laboratory (precisionesthetics.com), West Palm Beach, Florida, for the laboratory work in this case, and Fritz Orthodontics, Holly Springs, North Carolina, for the orthodontic photographs and work.
Disclosure
This article was commercially supported by Align Technology, Inc.
About the Author
Jennifer Bell, DDS
Private Practice, Holly Springs, North Carolina; Fellow, Academy of General Dentistry
References
1. Donovan T. Dental erosion. J Esthet Restor Dent. 2009;21(6):359-364.
2. Lussi A, Jaeggi T. Erosion-diagnosis and risk factors. Clin Oral Investig. 2008;12(suppl 1):S5-S13.
3. Dolt AH 3rd, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28(6):363-372.
4. Tak On T, Kois JC. Digital smile design meets the dento-facial analyzer: optimizing esthetics while preserving tooth structure. Compend Contin Educ Dent. 2016;37(1):46-50.
5. Velayati Moghadam F, Majidinia S, Chasteen J, Ghavamnasiri M. The degree of color change, rebound effect and sensitivity of bleached teeth associated with at-home and power bleaching techniques: a randomized clinical trial. Eur J Dent. 2013;7(4):405-411.
6. Lambrechts P, Van Meerbeek B, Perdigão J, et al. Restorative therapy for erosive lesions. Eur J Oral Sci. 1996;104(2[Pt 2]):229-240.
7. Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health. 20172;17(1):149.
8. Sun T, Zhou S, Lai R, et al. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J Mech Behav Biomed Mater. 2014;35:93-101.
9. Albashaireh ZSM, Ghazal M, Kern M. Two-body wear of different ceramic materials opposed to zirconia ceramic. J Prosthet Dent. 2010;104(2):105-113.
10. Dogan S, Raigrodski AJ. Cementation of zirconia-based toothborne restorations: a clinical review. Compend Contin Educ Dent. 2019;40(8):536-540.
11. Rutkūnas V, Gečiauskaite A, Jegelevičius D, Vaitiekūnas M. Accuracy of digital implant impressions with intraoral scanners. A systematic review. Eur J Oral Implantol. 2017;10(suppl 1):101-120.