Quantifying Flabby Ridge Tissue Displacement During Impression-Making for Patients With Combination Syndrome
John Antonelli, DDS, MS; Mauricio Guerrero, DDS; Michael Georgescu, DMD; and Julian Ortiz
Alveolar resorption subsequent to tooth extraction and denture wearing has been well documented.1,2 Reduction of residual ridges is chronic, progressive, and irreversible. Traumatic occlusal forces are known to play a role in accelerating residual ridge reduction. Kelly reported that massive resorption of alveolar bone in maxillary and mandibular arches could result in a mobile band of tissue on the crest of the ridge, the so-called "flabby ridge," which could produce symptoms of pain and unretentive dentures.3 Flabby ridges in the edentulous maxilla are almost five times more prevalent than in the mandible (24% versus 5%, respectively).1 Flabby ridges could occur following tooth extractions or as a result of wearing ill-fitting dentures.
A flabby or displaceable anterior maxillary ridge may be detected when the edentulous maxilla is opposed by natural teeth in the anterior mandible. This combination (hence, the term "Combination syndrome") causes trauma to the anterior maxillary ridge as all occlusal forces are directed onto this area, and fibrous replacement of the bony ridge occurs. In patients with Combination syndrome, compressive and rotational forces produced by natural mandibular anterior teeth on maxillary complete dentures cause resorption of alveolar bone in the anterior maxilla.
The effect of mandibular teeth on early loss of bone from the anterior edentulous maxilla has been discussed and investigated. Carlsson et al compared bone resorption of the anterior maxillary alveolar ridge among patients with complete maxillary dentures and (1) complete mandibular dentures; (2) natural mandibular teeth only, including molars; and (3) mandibular anterior teeth only, with or without bilateral distal extension removable partial dentures (RPDs).4 Greater maxillary bone resorption was detected in patients who had mandibular anterior teeth, with or without RPDs.
In two other studies, the anterior maxilla showed no statistically significant bone resorption in patients who wore mandibular overdentures supported by a straight bar attached to both canines.5,6 Patients with fixed, implant-supported mandibular prostheses also did not exhibit significant loss in anterior maxillary ridge height.7 It appears that restoring the edentulous mandible with a bar-supported overdenture or implant-supported prosthesis occluding with a complete maxillary denture does not promote a condition similar to Combination syndrome.
Kelly suggested that the pathogenesis of Combination syndrome progresses sequentially.3 The early loss of bone in the premaxilla heralds the formation of flabby hyperplastic tissue on the anterior maxillary ridge. Under occlusal loading, hyperplastic tissues beneath the complete denture are compressed/deformed anteriorly. Negative pressure within the maxillary denture pulls the tuberosities down as the anterior ridge is driven upward by the occluding mandibular teeth; subsequently, the maxillary tuberosities become fibrotic and enlarged. Functional loads that direct stress to the mandibular distal extension RPD cause bony resorption of the posterior ridge. The occlusal plane migrates upward in the anterior area and downward in the posterior. In time, mandibular anterior teeth super-erupt, and anterior teeth of the complete denture become progressively hidden under the patient's lip, and both dentures migrate downward in the posterior regions.
Esthetics are impacted negatively as (1) maxillary anterior teeth are progressively hidden under the lip and mandibular anterior teeth are increasingly exposed, and (2) the occlusal plane drops down to reveal more of the maxillary posterior teeth. Eventually, the patient loses vertical dimension of occlusion. Chronic stress and movement of the maxillary complete denture leads to an ill-fitting prosthesis and, potentially, papillary hyperplasia of the palate.
When flabby maxillary anterior ridge tissue is compressed by forces exerted during conventional impression-making (ie, using a mucocompressive or pressure-type technique), mobile tissue is invariably captured in a distorted state. If a denture were constructed on a master cast poured from such an impression, the denture would cause displacement of flabby tissues under masticatory loading because tissues conform to the shape of the intaglio surfaces of the denture. In other words, because of the viscoelastic property of tissue, the denture would fit only when seated by occlusal pressure (Figure 1). When unloaded, the denture would become loose as tissues recoil, resulting in a loss of peripheral seal and dislodgement of the denture (Figure 2).
The impression technique required for dealing with these problems is based on the need to avoid over-displacement of flabby tissues when recording the impression. There is a lack of consensus about the manner in which impressions of edentulous arches should be made.8-10 Also, there is a dearth of information in the dental literature to demonstrate the superiority of any impression material over another when the materials are used properly.11,12 To date, no studies quantify the degree of displacement of flabby tissues when various impression materials are used to make final impressions for complete dentures.
Case Reports
Two patients diagnosed with Combination syndrome were studied in an attempt to quantify displacement of anterior flabby maxillary tissues when the following six materials were used for making final impressions: (1) polysulfide, (2) zinc oxide eugenol (ZOE) paste, (3) tissue conditioner, (4) fast-set irreversible hydrocolloid, (5) polyether, and (6) polyvinyl siloxane (PVS).
An edentulous 72-year-old woman (Patient A) was restored with a complete maxillary denture 15 years ago. The patient used a mandibular bilateral distal extension RPD prior to the extraction of her remaining mandibular anterior teeth approximately 5 years ago. She experienced ongoing lack of retention and stability with her maxillary and mandibular complete dentures, which compromised her appearance. Radiographs disclosed severe maxillary anterior alveolar ridge resorption. Clinical examination revealed that masticatory forces exerted on the maxillary denture displaced anterior, flabby, denture-bearing tissue, which resulted in loss of peripheral seal and instability of the denture.
Practitioners should be concerned about the support for a denture when the residual ridge moves more than 2 mm under light pressure or if there is less than 1 mm of mucosa attached firmly to the underlying periosteum.13 Massad et al ranked the displacement of flabby tissue overlying the residual ridge after tactile assessment as (1) attached, low mobility, low displacement; (2) average, clinically acceptable; or (3) high mobility, high displacement.14 Manipulation of this patient's anterior maxilla revealed that hyperplastic tissues moved more than 2 mm with light pressure; therefore, the tissues were ranked as high mobility, high displacement, and very difficult to treat.13
Patient B was a 56-year-old man who was chosen for this investigation because he presented with an edentulous maxillary ridge and symptoms that were nearly identical to those of Patient A. He wore an ill-fitting complete maxillary denture and mandibular bilateral distal extension RPD for 10 years. Hyperplastic, flabby tissue in his anterior maxilla could be moved more than 2 mm with light pressure; accordingly, his tissues were rated as high mobility, high displacement, and very difficult to treat.
Both patients desired an alternative (nonsurgical) treatment plan despite being informed about the potential benefits (and risks) of implants and the problems that flabby ridges could continue to create by displacing the dentures under occlusal loads, potentially causing further bone loss, poor retention, pain, ulcers, and papillary hyperplasia.
Because the denture-bearing areas of the maxilla of both patients exhibited moderate to severe inflammation, they were advised to discontinue wearing their ill-fitting dentures for 48 hours prior to final impressions being made for this study and for the replacement dentures. Both patients refused, however, citing esthetic concerns associated with wearing no dentures. Therefore, to minimize further inflammation during functional loading, it was decided to reline their ill-fitting dentures with tissue conditioner, which was replaced every week for 3 weeks. This had the desired effect, along with the added benefits of enhancing retention, stability, and comfort of the prostheses.
Patient B's ill-fitting RPD was eventually replaced with a prosthesis that was made using the altered cast impression technique to reduce movement of the saddle areas of the denture into the underlying tissues.15 Cingulum rests were incorporated on the canines, and a linguoplate major connector was used to delay overeruption of the mandibular teeth and prevent pressure on the anterior part of the maxillary denture. Posterior occlusal support was maximized, with no contact anteriorly in centric relation. In accordance with Kelly,3 balanced occlusion during eccentric excursions was used to help reduce potentially destructive forces exerted on the anterior maxillary residual ridge.
For this study, light-cured urethane dimethacrylate resin custom trays were used; trays were trimmed so that the periphery was 2 mm short of the functional sulcus. The trays, at 2 mm to 3 mm thick, were sufficiently rigid to avoid flexing during impression-making.
Prior to impression-making, the maxillary arches were captured in their relaxed states by scanning them with an intraoral scanner/CAD/CAM technology (3M True Definition™, 3M ESPE, 3m.com). Acrylic casts of each maxillary arch were milled from the scans and served as the relaxed tissue (control) casts. Next, the same border-molded custom trays were used to make final impressions. For Patient A, final impressions were made with polysulfide, ZOE paste, and tissue conditioner. Irreversible hydrocolloid, polyether, and PVS materials were used to make final impressions for Patient B. Scans of each impression were made with the same CAD/CAM technology to generate milled acrylic (experimental) casts of the maxillary arches in which anterior flabby tissues were registered in their deformed states.
Ultimately, new complete maxillary dentures were fabricated for each patient using a two-stage impression technique in which windows were created in the custom impression trays over flabby tissues (Figure 3 and Figure 4). To obtain optimal support for the dentures, mucocompressive impressions of rigid tissues were made with polysulfide impression material. After polysulfide material polymerized completely, trays were removed from the mouth of each patient and all excess material that flowed into the tray windows was removed using a sharp scalpel blade. After the trays were reseated fully, mucostatic impressions of anterior flabby tissues were made by extruding (with a curved extrusion tip attached to an automixing tip) extra-low-viscosity PVS material into the tray windows to minimize displacement of flabby tissues (Figure 5). The aim of this technique is to maintain the contour of the easily displaced anterior tissues while the rest of the denture-bearing areas are recorded.
Final impressions were inspected for accuracy and poured in vacuum-mixed, type III dental stone to create the master casts. Replacement dentures were fabricated for both patients. The use of polysulfide and extra-low-viscosity PVS materials in a two-stage impression technique helped produce stable and retentive prostheses that required only two post-insertion adjustments each.
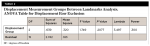
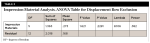
To measure the degree of fibrous tissue displacement in the anterior maxilla during impression-making, six identical points (A, B, C, D, E, and F) were identified on each of the eight casts, using landmarks that were captured in the impressions. Three points (B, D, and F) were chosen on the hard palate, and three points (A, C, and E) were identified on flabby tissues (Figure 6). Distances between points were measured with a digital caliper, purportedly accurate within ±0.03 mm (Table 1). The greatest average tissue displacement (0.95 mm) along all points on the casts was seen when PVS impression material was used. In decreasing order, the average tissue displacements measured between points on the casts were produced by irreversible hydrocolloid (0.67 mm), polysulfide (0.51 mm), polyether (0.50 mm), tissue conditioner (0.19 mm), and ZOE paste (0.15 mm). Average tissue displacement resulting from use of PVS was 6.3 times greater than with ZOE paste, which produced the least displacement. Average tissue displacement with use of PVS was 5 times greater than with use of tissue conditioner; 1.9 times greater than with polysulfide and polyether; and 1.4 times greater than with irreversible hydrocolloid. Although PVS material produced the greatest displacement of flabby ridge tissue, the amount was less than half the distance that these tissues could be moved with light tactile pressure. The P values in this study are not significant because of the variability of the data. The power values are low, which indicates the need to collect more specimens to obtain reliable P values (Table 2 and Table 3).
Discussion
Brignardello-Petersen et al recommended that any benefit to improved health outcomes must be both clinically and statistically significant.16 The authors claimed that to be clinically significant, (1) a change in an outcome must be of interest to someone, either the clinician or patient, so that the effect of one treatment compared to another makes a difference; (2) the difference between groups must result in an important outcome (eg, reduction in symptoms, improvement in quality of life); and (3) the differences should be statistically significant. Lack of long-term patient follow-up makes it impossible to claim that any impression material tested meets the first criterion for clinical significance (ie, does the material impact tissue inflammation, denture retention, comfort, or alveolar resorption rate?).
When making final impressions of highly displaceable ridge tissues, an impression technique is required that will compress rigid tissues that are still capable of bearing a load so that they can be used for retention and absorbing the forces of mastication and, at the same time, displace flabby tissues minimally. Properly executed, the two-stage technique described should record flabby tissue in its minimally displaced state (ie, no impression technique or material will capture tissue without some degree of displacement). The two-stage technique appears to have the most advocates.17 The use of standard mucocompressive impression techniques (ie, impressions that are made with trays without windows over moveable tissues) could cause greater deformation of flabby tissues and should, therefore, be avoided, because such techniques will likely produce dentures that compress tissues under masticatory loading and exhibit a loss of peripheral seal, poor retention, and instability. To date, studies of impression materials for edentulous patients with flabby ridge tissues have centered mainly on techniques for minimizing displacement; the choice of impression materials has depended on individual preference, based on analysis of theoretical principles.18
Petrie et al stated that years of experience had a statistically significant effect on the materials prosthodontists chose for border molding procedures, but not for the materials used for making final impressions of edentulous arches.19 In the absence of rigorous laboratory or clinical tests to support the present authors' contentions about the superiority of any impression material(s) to use for complete denture impressions in different clinical situations, it is the judgment of experienced clinicians that must be called upon because, in the authors' hierarchy of evidence, this is perfectly appropriate.20
Proper diagnosis of the condition of the tissues, as well as consideration of the patient's presenting complaint, should help in determining the selection of impression technique and final impression material(s) for a specific patient.Severely resorbed maxillary and mandibular ridges present a challenge for clinicians attempting to provide functionally successful complete dentures for these patients. This investigation has quantified the degree of tissue displacement caused by six types of popular impression materials. It is recommended that when a custom tray with a window over the flabby ridge is used, any of the impression materials tested could be used in this situation to capture displaceable tissues in a minimally displaced state. Further, the authors recommend vacuum mixing fast-set irreversible hydrocolloid for 20 to 25 seconds (using cold water) to obtain a more homogenous and void-free mix.
The Commission on Dental Accreditation requires dental colleges to adopt an evidence-based approach to teaching oral healthcare that "…uses thorough unbiased systematic reviews and critical appraisal of the best available scientific evidence in combination with clinical and patient factors to make informed decisions about appropriate healthcare for specific clinical circumstances."21 If all faculty members would exemplify this philosophy, it could become rooted in the mindset of students, and moreover, a close connection would be fostered between what students learn in dental college and how they perform in private practice. If the dental community considers the emerging and profound impact that an evidence-based approach has on clinical practice, then clinicians should base treatment on noncontroversial, evidence-based criteria-rather than that which is essentially anecdotal.
Conclusion
Practitioners must seek information from high-quality research so they may be better able to make evidence-based decisions when choosing impression materials for producing complete dentures for patients with ridges that are rated high mobility, high displacement, and very difficult to treat. The paucity of such research, however, prompts the authors to recommend that practitioners continue to rely on information from experienced clinicians and use techniques that produce good results.
About the Authors
John Antonelli, DDS, MS
Professor and Director of Fixed Prosthodontics Courses, Department of Prosthodontics, Nova Southeastern University, College of Dental Medicine, Fort Lauderdale, Florida
Mauricio Guerrero, DDS
Assistant Professor, Department of Prosthodontics, Nova Southeastern University, College of Dental Medicine, Fort Lauderdale, Florida
Michael Georgescu, DMD
Assistant Professor, Department of Cariology and Restorative Dentistry, Nova Southeastern University, College of Dental Medicine, Fort Lauderdale, Florida
Julian Ortiz
Fourth-Year Dental Student, Nova Southeastern University, College of Dental Medicine, Fort Lauderdale, Florida
References
1. Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27(2):120-132.
2. Atwood DA. Some clinical factors related to rate of resorption of residual ridges. J Prosthet Dent. 2001;86(2):119-125.
3. Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 1972;27(2):140-150.
4. Carlsson GE, Bergman B, Hedegärd B. Changes in contour of the maxillary alveolar process under immediate dentures. A longitudinal clinical and x-ray cephalometric study covering 5 years. Acta Odontol Scand. 1967;25(1):45-75.
5. Üçtaşli S, Hasanreisoğlu U, Işeri H. Cephalometric evaluation of maxillary complete, mandibular fixed-removable partial prosthesis: a 5-year longitudinal study. J Oral Rehabil. 1997;24(2):164-169.
6. Carlsson GE, Ragnarson N, Astrand P. Changes in height of the alveolar process in edentulous segments. II. A longitudinal clinical and radiographic study over 5 years of full upper denture patients with residual lower anteriors. Sven Tandlak Tidskr. 1969;62(3):125-136.
7. Gupta S, Lechner SK, Duckmanton NA. Maxillary changes under complete dentures opposing mandibular implant-supported fixed prostheses. Int J Prosthodont. 1999;12(6):492-497.
8. Oh WS, Morris HF. The principles of functional and mucostatic impressions for complete denture bases: a review. Compend Contin Educ Dent. 2017;38(10):664-667.
9. Carlsson GE, Ŏrtorp A, Omar R. What is the evidence base for the efficacies of different complete denture impression procedures? A critical review. J Dent. 2013;41(1):17-23.
10. Allen F. Management of the flabby ridge in complete denture construction. Dent Update. 2005;32(9):524-528.
11. Al-Ahmar AO, Lynch CD, Locke M, Youngson CC. Quality of master impressions and related materials for fabrication of complete dentures in the UK. J Oral Rehabil. 2008;35(2):111-115.
12. Petrie CS, Walker MP, Williams K. A survey of U.S. prosthodontists and dental schools on the current materials and methods for final impressions for complete denture prosthodontics. J Prosthodont. 2005;14(4):253-262.
13. MacEntee MI. The Complete Denture. A Clinical Pathway. Chicago, IL: Quintessence Publishing; 1999:6.
14. Massad J, Lobel W, Garcia LT, et al. Building the edentulous impression-a layering technique using multiple viscosities of impression material. Compend Contin Educ Dent. 2006;27(8):446-451.
15. Phoenix RD, Cagna DR, De Freest CF. Stewart's Clinical Removable Partial Prosthodontics. Chicago, IL: Quintessence Publishing; 2003:363-365.
16. Brignardello-Petersen R, Carrasco-Labra A, Shah P, Azarpazhooh A. A practitioner's guide to developing critical appraisal skills: what is the difference between clinical and statistical significance? J Am Dent Assoc. 2013;144(7):780-786.
17. Crawford RW, Walmsley AD. A review of prosthodontic management of fibrous ridges. Br Dent J. 2005;199(11):715-719.
18. Pai UY, Reddy VS, Hosi RN. A single step impression technique of flabby ridges using monophase polyvinylsiloxane material: a case report. Case Rep Dent. 2014;2014:104541. doi: 10.1155/2014/104541.
19. Petrie CS, Walker MP, Williams K. A survey of U.S. prosthodontists and dental schools on the current materials and methods for final impressions for complete denture prosthodontics. J Prosthodont. 2005;14(4):253-262.
20. Goodacre C. Principles of Tooth Preparation [DVD]. Chicago, IL: The American College of Prosthodontists; 2003.
21. Commission on Dental Accreditation. Accreditation Standards for Predoctoral Dental Education Programs. Chicago IL: 2019. https://www.ada.org/~/media/CODA/Files/pde.pdf?la=en. Accessed July 8, 2019.