Immediate Placement of Dental Implants in Molar Extraction Sockets: An 11-Year Retrospective Analysis
Richard B. Smith, DDS; Dennis P. Tarnow, DDS; and Guido Sarnachiaro, DDS
Abstract: The authors present an 11-year retrospective analysis of 300 immediately placed implants in molar extraction sockets. The protocol used for the placement and restoration of these implants is based upon a previously published article by the authors regarding the classification of molar extraction sockets. Four different implant systems were used during this study, and implants varied in diameter, length, and texture. Some implants were immediately provisionalized, and some were immediately loaded. The overall survival rate of 97.3% is similar to previously reported survival rates in delayed molar implant placement protocols. The benefits of immediate molar implant placement include a reduced number of surgical procedures and patient visits, lower cost of treatment, and shorter time required from beginning to completion of treatment.
First described in 1989, immediate placement of dental implants into fresh molar extraction sockets is an accepted procedure.1-6 Advantages of immediate molar implant placement versus delayed protocol include the need for fewer surgical procedures and patient visits, lower cost of treatment, and less time required from the start of treatment to its completion.7 The cumulative survival rate for immediately placed molar implants is similar to implants placed in healed molar extraction sites.3,8 The critical elements for successful placement of immediate implants are initial stability provided by the apical or lateral bone and a sufficiently high insertion torque value (ITV).9,10
A classification system by Smith and Tarnow describing three categories of molar extraction sockets (types A, B, and C, Figure 1 through Figure 3) based upon the amount of interradicular septal bone and its influence on implant stability has helped establish guidelines for successful immediate molar implant placement.11 Over close to a decade, the authors placed 300 implants into fresh molar extraction sites in accordance with these guidelines. The implant survival rate in the present study has proven to be equal to that expected of implants placed in a delayed protocol.
Materials and Methods
The authors placed 300 immediate molar implants from 2006 through 2014 and conducted this 11-year retrospective analysis in 2017. The implants were all tapered, varied in diameter, length, and surface texture, and were manufactured by four different companies (Biomet 3i, biomet3i.com; BioHorizons, biohorizons.com; Keystone Dental/Southern Implants, southernimplants.com; and Dentium, dentiumusa.com). Teeth were deemed nonrestorable and removed due to advanced decay, advanced bone loss, nontreatable endodontic lesions, or vertical fractures.
Preoperative radiographs and/or cone-beam computed tomography (CBCT) scans were obtained to identify anatomical risk factors and to better predict the potential for immediate implant placement. In some instances an intraoperative radiograph/CBCT was obtained following extraction. Extractions were all performed without elevation of a mucoperiosteal flap to preserve as much buccal plate as possible.12 Maxillary and mandibular multi-rooted molars were sectioned prior to extraction to allow elevation and removal of individual roots, thereby preserving the interradicular and buccal bone.
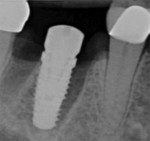
Socket types were identified based upon the aforementioned classification system.11 All sockets had to have intact outer walls with no dehiscence defects present. All implants placed had to exhibit initial stability with ITVs of 15 Ncm or greater and no lateral mobility to ensure successful integration.9 Only those implants with an ITV of 30 Ncm or greater were considered for immediate provisional restoration. The root sockets of type A sites were not grafted, nor were the gaps adjacent to the implants in type B and C sockets. No membranes were placed, and no primary closure was attempted as no flaps were raised in any of the extraction/implant placement procedures. With no grafts, membranes, or soft-tissue closure, it could be anticipated that bone would fill even the largest socket spaces, providing full osseointegration of the implants (Figure 4 through Figure 6).13
11-Year Retrospective Data
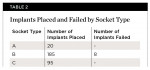
The 300 immediate implants were placed into fresh molar extraction sites. The breakdown according to implant socket type categories is as follows: type A, 20; type B, 185; and type C, 95. The overall survival rate was 97.3% with a total of eight failures. Of the 300 implants placed, 38 received immediate provisional restorations, 10 of which were loaded as part of a multi-unit splinted restoration, while 28 were non-loaded single-tooth provisional restorations. Of these immediately restored implants, only two failed, one at 4 months and one at 9 months, and both were single-tooth replacements in type B sockets. No failures occurred beyond 16 months postoperatively. The failures reported were all encountered in the early phases of developing the current protocol and before wider-diameter implants became available to the authors (Table 1 and Table 2).
One "adverse event" was recorded, as a single implant was removed within the first week after placement due to a dry socket in a mandibular second molar type C socket, but this was not considered a "failure" because the dry socket occurred independent of the implant placement. After implant removal and a usual healing period of 3 months the implant was replaced in a delayed protocol without issue.
Clinical Case Examples
Restoration of a type C socket is depicted in Figure 7 through Figure 10, while restoration of a type B socket is shown in Figure 11 through Figure 13.
Discussion
The keys to successful immediate molar implant placement are flapless extractions, maintenance of interradicular bone where indicated, presence of intact outer bony walls (though not necessary for type A sockets), and adequate initial implant stability. Case selection is paramount.
Most often the osteotomy cannot be extended significantly past the apex of the molar extraction site because of the presence of anatomic structures such as the maxillary sinus and inferior alveolar nerve. Therefore, implant stability becomes the most obvious challenge. In socket types A and B it is critical to preserve as much of the interradicular bone (septum) as possible for implant stabilization. In type C sockets the thickness of the outer walls must be sufficient such that engaging the socket wall will not lead to loss of integration after the inevitable remodeling that occurs regardless of implant placement.14 The buccal walls of molar sockets are, on average, much thicker than those found anteriorly and, therefore, are unlikely to completely resorb upon remodeling.15,16
The vertical positioning of the implant should leave the prosthetic platform 3 mm to 4 mm of space apical to the cementoenamel junction of the adjacent teeth and/or 3 mm to 4 mm of space apical to the soft-tissue margin for proper emergence and crown contours of the restoration. The average molar root trunk length is 3.27 mm (mandibular) and 4.3 mm (maxillary).17 Therefore, using the level of the interradicular septal bone, when present, as the vertical landmark is recommended.
The diameter of the implant placed is limited by the buccal-lingual width of the ridge beyond the internal walls of the socket. For molar restorations the widest prosthetic platform possible is preferred, as it will afford the most appropriate restorative emergence contours. Therefore, it may be advisable to place a wider implant at the expense of the interradicular bone only if the outer walls are intact, effectively turning a type A or B socket into a type C socket for greater prosthetic effectiveness. If, however, either the buccal or lingual (palatal) outer wall is thinner than 1 mm, it may be better to utilize the narrower-diameter implant, stabilized in interradicular bone, so as not to engage a fragile outer wall that is likely to resorb subsequent to implant placement.
Placement of an immediate implant into one of the root sockets of a multi-rooted tooth, which the authors still considered a type B socket, is an alternative that should be considered with caution. While initial stability may be achieved easily within the root socket, the position and diameter of the implant and its prosthetic platform may lead to unfavorable restorative outcomes, including less-than-ideal prosthetic emergence contours, cantilevered crown proportions that are not conducive to good hygiene, and off-angle prosthetic alignment resulting in poorly positioned screw-access openings.
Immediate Provisional Restoration
To preserve the soft-tissue ridge architecture around the immediate implant, either a non-loaded provisional restoration or a customized healing abutment may be placed (Figure 14 and Figure 15).
Conclusion
Immediate implants may be placed successfully into fresh molar extraction sockets when initial implant stability can be attained. The interradicular bone may be used to stabilize or, in some instances, fully contain the implant. Sockets that do not have adequate interradicular bone for implant stability may require the use of wider-diameter implants that can engage the perimeter walls of the molar socket. The survival rate of immediately placed molar implants is similar to that of implants placed in a delayed protocol. Immediate molar implant placement, therefore, could be considered a predictable treatment option when the socket morphology is appropriate.
Disclosure
Drs. Smith and Tarnow are consultants for Keystone Dental. Dr. Tarnow also has received honoraria and/or research support from BioHorizons, Biomet 3i, and Dentium.
About the Authors
Richard B. Smith, DDS
Associate Clinical Professor, Department of Prosthodontics, Columbia University, College of Dental Medicine, New York, New York
Dennis P. Tarnow, DDS
Clinical Professor, Department of Periodontology, Director of Implant Education, Columbia University, College of Dental Medicine, New York, New York
Guido Sarnachiaro, DDS
Assistant Clinical Professor, Department of Prosthodontics, New York University, College of Dentistry, New York, New York
References
1. Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent. 1995;74(1):51-55.
2. Schwartz-Arad D, Grossman Y, Chaushu G. The clinical effectiveness of implants placed immediately into fresh extraction sites of molar teeth. J Periodontol. 2000;71(5):839-844.
3. Atieh MA, Payne AG, Duncan WJ, et al. Immediate placement or immediate restoration/loading of single implants for molar tooth replacement: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2010;25(2):401-415.
4. Fugazzatto PA. Implant placement at the time of maxillary molar extraction: treatment protocols and report of results. J Periodontol. 2008;79(2):216-223.
5. Fugazzatto PA. Implant placement at the time of mandibular molar extraction: description of technique and preliminary results of 341 cases. J Periodontol. 2008;79(4):737-747.
6. Cafiero C, Annibali S, Gherlone E, et al. Immediate transmucosal implant placement in molar extraction sites: a 12-month prospective multicenter cohort study. Clin Oral Implants Res. 2008;19(5):476-482.
7. Barndt P, Zhang H, Liu F. Immediate loading: from biology to biomechanics. Report of the Committee on Research in Fixed Prosthodontics of the American Academy of Fixed Prosthodontics. J Prosthet Dent.2015;113(2):96-107.
8. Ketabi M, Deporter D, Atenafu EG. A systematic review of outcomes following immediate molar implant placement based on recently published studies. Clin Implant Dent Relat Res. 2016;18(6):1084-1094.
9. Walker LR, Morris GA, Novotny PJ. Implant insertional torque values predict outcomes. J Oral Maxillofac Surg. 2011;69(5):1344-1349.
10. Block MS. Placement of implants into fresh molar sites: results of 35 cases. J Oral Maxillofac Surg. 2011;69(1):170-174.
11. Smith RB, Tarnow DP. Classification of molar extraction sites for immediate dental implant placement. Int J Oral Maxillofac Surg. 2013;28(3):911-916.
12. Degidi M, Nardi D, Daprile G, Piattelli A. Buccal bone plate in the immediately placed and restored maxillary single implant: a 7-year retrospective study using computed tomography. Implant Dent. 2012;21(1):62-66.
13. Tarnow DP, Chu SJ. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restorative Dent. 2011;31(5):515-521.
14. Araújo MG, Sukekava F, Wennström JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005;32(6):645-652.
15. Katranji A, Misch K, Wang HL. Cortical bone thickness in dentate and edentulous human cadavers. J Periodontol. 2007;78(5):874-878.
16. Sanz M, Cecchinato D, Ferrus J, et al. A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla. Clin Oral Implants Res. 2010;21(1):13-21.
17. Kerns DG, Greenwell H, Wittwer JW, et al. Root trunk dimensions of 5 different tooth types. Int J Periodontics Restorative Dent. 1999;19
(1):82-91.